-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(9): 904-907
doi:10.5923/j.ajmms.20221209.11
Received: Aug. 15, 2022; Accepted: Aug. 29, 2022; Published: Sep. 15, 2022

Clinical and Morphological Substantiation of Correction of the Course of Chemotherapy in the Surgical Treatment of Liver Echinococcosis
Kurbaniyazov Zafar Babazhanovich, Rakhmanov Kosim Erdanovich, Mizamov Furkat Ochilovich
Samarkand State Medical University, Uzbekistan
Correspondence to: Kurbaniyazov Zafar Babazhanovich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Experimental studies on sheep have shown that stimulation of a proliferative-productive cellular reaction around the germinal cyst of a parasite with an inhibitory effect when using albendazole at a dose of 10-15 and 20 mg/kg occurs within 2 weeks, while at a dose of 5-7 mg/kg the effect came to 3-4 weeks of observation. Studies allow us to adjust the recommended dose of albendazole from 10-12 mg/kg in cases of a possible risk of developing toxic reactions (diffuse liver disease) to 5-7 mg/kg, taking into account the prolongation of the course of treatment. Clinically justified is the use of an adjusted dose of albendazole 5-7 mg/kg for the prevention of recurrence of liver echinococcosis in patients with concomitant chronic diffuse liver pathology, which made it possible to reduce the likelihood of adverse reactions and the frequency of recurrence of the disease from 11.9% to 2.6%.
Keywords: Liver echinococcosis, Surgical treatment, Chemotherapy
Cite this paper: Kurbaniyazov Zafar Babazhanovich, Rakhmanov Kosim Erdanovich, Mizamov Furkat Ochilovich, Clinical and Morphological Substantiation of Correction of the Course of Chemotherapy in the Surgical Treatment of Liver Echinococcosis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 904-907. doi: 10.5923/j.ajmms.20221209.11.
1. Introduction
- According to the World Health Organization, more than 1 million people are affected by echinococcosis in the world, while among various organs and tissues in 44-84% of cases the process is localized in the liver. [5,6,7]. Due to the absence of a downward trend in the number of patients and the existence of endemic regions, where the incidence rate varies from 1.2 to 9.0 per 100,000 population, this parasitic disease continues to be a serious medical and social problem [4,8,10]. At the present stage, the diagnosis of liver echinococcosis (EP) does not present significant difficulties, largely due to the emergence of non-invasive imaging methods, the informativeness of the complex application of which reaches 95-100% [1,10]. However, the lack of alertness in relation to echinococcosis contributes to late diagnosis, and, consequently, an increase in complicated forms of the disease [2,3,7,11]. A fairly high incidence of postoperative complications (34-50%) and numerous cases of postoperative recurrence of the disease (15-64%) indicate a lack of effectiveness and reliability of common surgical tactics [7,9]. In the light of the foregoing, it becomes obvious that there is a need to improve the known and develop new effective measures for the prevention and treatment of this formidable disease.
2. Target
- Improving the quality of treatment of patients with liver echinococcosis by developing effective methods to reduce the recurrence of the disease.
3. Material and Methods
- For the purpose of research the influence of albendazole in various dosages on the germinal forms of echinococcosis, a morphological study of the internal organs of experimental animals (32 sheep, whose age ranged from 2 to 5 years, and of both genders) infected with echinococcosis in natural conditions was carried out. On the basis of ultrasound, all these animals were diagnosed (with the participation of specialists - veterinarians) liver echinococcosis.To determine the effect of albendazole, at the first stage of the experimental study, liver tissues of sheep that did not receive chemotherapy were studied. Morphological study was carried out on serial sections of the liver, stained with hematoxylin - eosin. In all animals, newly formed germinal cysts were found in the liver. The rest of the animals were treated with albendazole for 2 and 3 weeks at different dosages of the drug (5, 10, 15 and 20 mg/kg body weight).The clinical study included 371 patients with EP. The vast majority of echinococcectomy performed (99.8%) was of an organ-preserving nature, 412 (77.6%) residual cavities were treated according to the type of closed echinococcectomy, and only 116 (21.8%) fibrous capsules were sutured by a semi-closed method on drainage.
4. Results and Discussion
- When studying the liver of animals treated with albendazole at a dose of 5 mg/kg of body weight for 3 weeks, microscopically, the walls of the germinal cyst were homogeneous, significantly thickened. On the periphery, a rather powerful framework of lymphoid-histiocytic cells was formed. At a dose of 10 mg/kg of body weight for 2 weeks, it was determined that among the lobules of the liver, the emerging germinal blisters of echinococcus, consisting of a layered chitinous membrane, filled with amorphous masses, are visible. Among them are visible scolex. There is marked delamination and swelling of the wall of the chitinous membrane.Microscopic examination of the liver while taking albendazole at a dose of 15 mg/kg of animal weight for 2 weeks revealed that the newly formed germinal capsule of the echinococcal bladder was edematous and the walls were loosened. Along the periphery of the bladder wall, lymphoid-histocytic infiltrates appear, which were not noted at a dose of 10 mg / kg. When studying the liver of sheep treated with albendazole at a dose of 20 mg/kg of animal weight for 2 weeks, it was microscopically revealed that the peripheral zones of the germinal capsule of echinococcus are significantly enriched in lymphoid cell infiltrates. The cavity forming the cyst gapes, it contains an amorphous mass. The walls of the capsule are homogeneous, homogeneous.Before the start of chemotherapy, during and at the end of the course of chemotherapy, a complete blood count, biochemical parameters, and a coagulogram were examined. In sheep treated with albendazole at a dose of 5 mg/kg, no pathological changes were observed in the blood test. Sheep treated with albendazole at a dose of 10 and 15 mg/kg had minor changes in blood biochemical parameters. At a dose of 20 mg/kg, blood enzymes were moderately elevated at the end of the first week, and increased significantly at the end of the second week.Studies have shown that in remote areas of the liver from the primary echinococcal bladder, microscopically identifiable germinal echinococcal microcysts were found. They were represented by formed or emerging chitinous membranes without signs of a macrophage-cellular reaction around the embryonic formation, or with a pronounced cellular reaction. Treatment with albendazole at a high dose of 10 mg/kg of body weight for 2 weeks and a lower dose of 5 mg/kg of body weight for 3 weeks contributed to the stimulation of a proliferative-productive cellular reaction around the germinal cyst of the parasite and had a depressing effect on echinococcus scolex (Fig. 1, 2.).
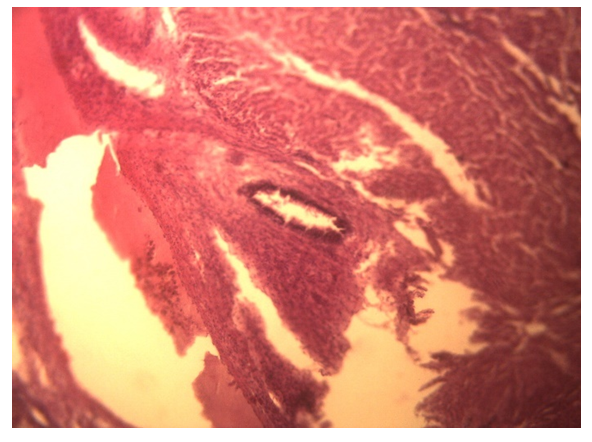 | Figure 1. Sheep liver not treated with albendazole. Thickened chitinous membrane with a tendency to invade. No cellular infiltrates. Hematoxylin-eosin staining. Enlarged. 10×15 |
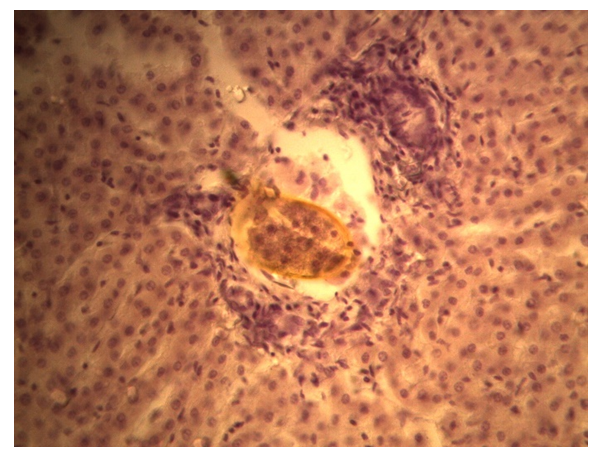 | Figure 2. Sheep liver not treated with albendazole. Forming germinal cyst of echinococcus. Hematoxylin-eosin staining. Enlarged. 10×40 |
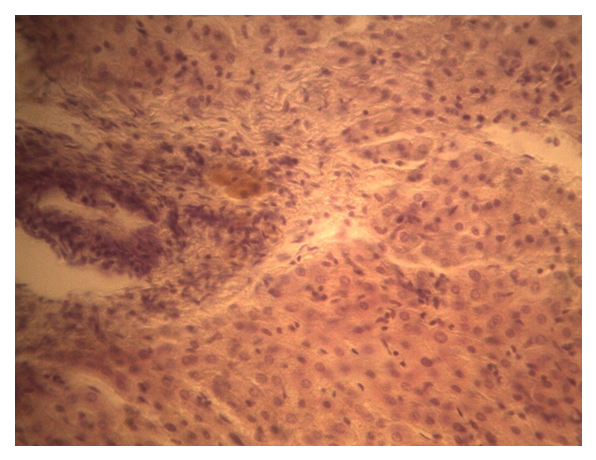 | Figure 3. Sheep liver not treated with albendazole. Forming germinal cyst of echinococcus without any cellular reaction along the periphery. Hematoxylin-eosin staining. Enlarged. 10×15 |
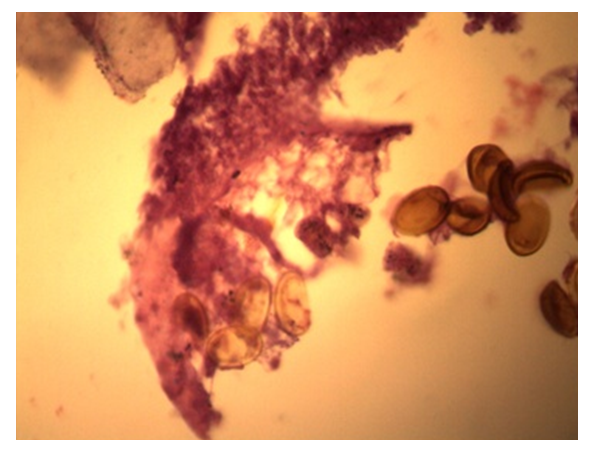 | Figure 4. Sheep liver not treated with albendazole. Protoscolexes and scolexes are visible in the bladder cavity. Hematoxylin-eosin staining. Enlarged. 10×40 |
5. Findings
- Experimental studies on sheep have shown that stimulation of a proliferative-productive cellular reaction around the germinal cyst of a parasite with an inhibitory effect when using albendazole at a dose of 10-15 and 20 mg/kg occurs within 2 weeks, while at a dose of 5-7 mg/kg the effect came to 3-4 weeks of observation. Studies allow us to adjust the recommended dose of albendazole from 10-12 mg/kg in cases of a possible risk of developing toxic reactions (diffuse liver disease) to 5-7 mg/kg, taking into account the prolongation of the course of treatment.Clinically justified is the use of a dose of albendazole 5-7 mg/kg for the prevention of recurrence of liver echinococcosis in patients with concomitant chronic diffuse liver pathology, which made it possible to reduce the likelihood of adverse reactions from 52.7% to 18.3%, and, accordingly, indicators of hepatic aminotransferases: ALT in the group comparisons from 1.14±0.11 to 0.62±0.05 mmol/l in the main group and AST from 0.72±0.07 to 0.52±0.04 mmol/l.Correction of the course dose of prophylactic chemotherapy improved the quality of care provided by reducing the frequency of recurrence of the disease from 11.9% (19 patients in the comparison group) to 2.6% (in 2 patients in the main group).Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML