Kadirov Rustam Nadirovich, Yarashev Sultonbek Saloxiddinovich, Nurillaev Hasan Jamshidovich
Samarkand Branch of the Republican Scientific Center for Emergency, Medical Care
Correspondence to: Kadirov Rustam Nadirovich, Samarkand Branch of the Republican Scientific Center for Emergency, Medical Care.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The paper analyzes the results of surgical treatment of 57 patients with acute cholecystitis and choledocholithiasis. Staged surgical treatment with the use of preliminary decompressive interventions on the bile ducts made it possible to stop the phenomena of cholestasis and purulent intoxication, improve the results of radical operations. At the same time, 81.8% of patients with severe, 61.6% of moderate severity and 24.1% with mild severity of acute purulent cholangitis needed to use diapeutic and endoscopic transduodenal interventions. Optimization of the tactical and technical aspects of the complex surgical treatment of patients with acute cholecystitis and choledocholithiasis complicated by acute purulent cholangitis made it possible to significantly reduce postoperative purulent-septic and cholemic complications to 12.1%, mortality to 2.4%.
Keywords:
Cholelithiasis, Acute cholecystitis, Choledocholithiasis, Surgical tactics
Cite this paper: Kadirov Rustam Nadirovich, Yarashev Sultonbek Saloxiddinovich, Nurillaev Hasan Jamshidovich, Minimally Invasive Interventions in Surgical Treatment of Complications of Choleliyhiasis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 900-903. doi: 10.5923/j.ajmms.20221209.10.
1. Relevance
The leading place in the structure of postoperative complications after cholecystectomy (CE) is occupied by external or intra-abdominal bile leakage (BI) in the early postoperative period, which should be considered as an independent problem, since it can have serious consequences and be life-threatening [1,2,3,10,11,14,16,17]. The main causes of postoperative GI are damage to the peripheral bile ducts (aberrant hepatocystic ducts of the gallbladder bed - Luschka's ducts, leakage of the cystic duct stump) and "large" - iatrogenic damage to the main bile ducts [5,19,21].The outflow of bile through the drainage contributes to the early diagnosis of biliary complications, but even a small bile leakage into the abdominal cavity can lead to serious complications [4,6,7,13,20]. Diagnosis of intra-abdominal bile leakage is a difficult task, the presence of safety drainage in the sub hepatic space contributes to early diagnosis and prevention of biliary peritonitis [8,9,12,15,18].
2. The Aim of the Study
The aim of the study was to improve the results of surgical treatment of patients with acute cholecystitis and choledocholithiasis by differentiated use of minimally invasive methods for correcting bile flow.
3. Material and Research Methods
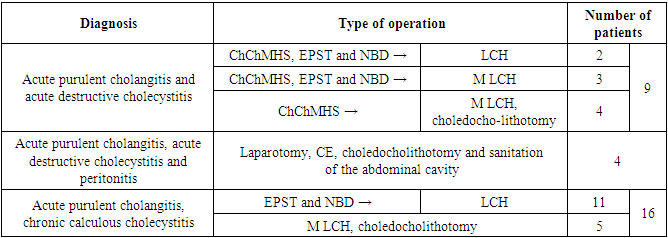
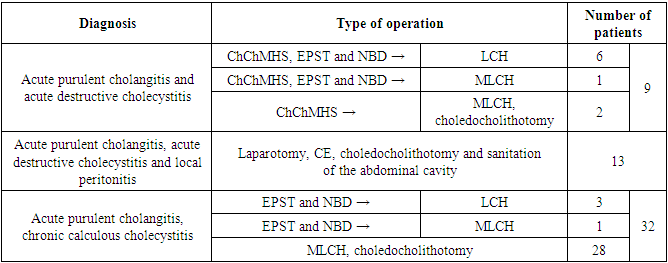
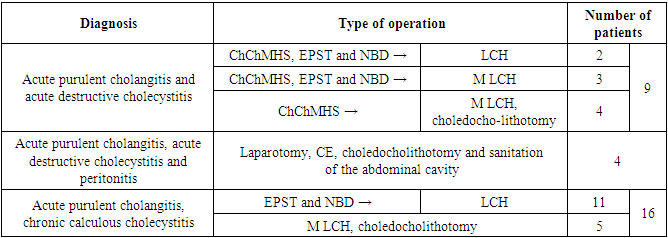
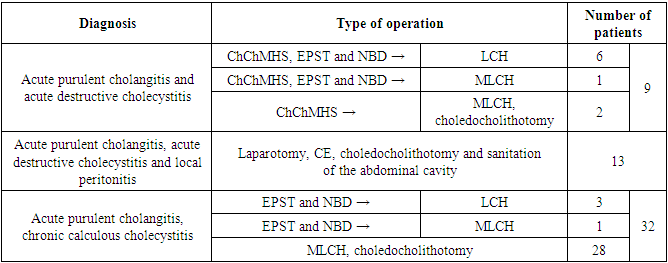
In a group of 83 patients with acute cholecystitis and choledocholithiasis operated on in 2010-2019. treatment was carried out taking into account the severity of acute suppurative cholangitis (AHC) proposed at the conciliation conference in Tokyo (2013). In accordance with these criteria, mild severity was noted in 54 (65%) patients, moderate in 18 (21.6%), and severe in 11 (13.2%) patients.The patients were subjected to various minimally invasive and open surgical interventions, taking into account the proposed severity criteria, as well as the presence of a clinic of acute destructive cholecystitis and peritonitis.In patients with moderate severity (n=18) and severe AHC (n=11), minimally invasive decompressive interventions were used as the first stage of treatment in 20 patients. (Table 1).Table 1. Surgical interventions in patients with AHC of moderate and severe severity in the main group (n=29)
 |
| |
|
At the same time, in 9 patients with acute destructive cholecystitis, decompression of the gallbladder was performed by means of percutaneous transhepatic microcholecystostomy (PCMCS) under ultrasound control. Then, 5 of them underwent endoscopic papillosphincterotomy (EPST) and nasobiliary drainage (NBD). In the remaining 4 patients, PTCS significantly stopped the clinical manifestations of AHC. In 11 patients without a clinical picture of acute cholecystitis, the first stage was endoscopic transduodenal intervention - EPST with lithoextraction and NBD of the choledochus. The second stage in these 20 patients on days 7-12 was laparoscopic cholecystectomy (LCE) -13, minilaparotomic cholecystectomy (MLCE) -7, while in 4 LCCE it was supplemented with choledocholithotomy.In 4 patients with clinical peritonitis, according to emergency indications, laparotomy, CE, choledocholithotomy and sanitation of the abdominal cavity were performed. Another 5 patients with a progressive AHC clinic with an unsuccessful attempt at EPST underwent CE with choledocholithotomy from an open mini-access.Thus, two-stage surgical treatment was performed in 11 (61.1%) patients with moderate severity and 9 (81.8%) with severe AHC.In mild AHC, two-stage surgical treatment was performed in 13 (24.1%) patients, one-stage radical surgery was performed in 41 patients (Table 2).Table 2. Surgical interventions in patients with acute purulent cholangitis of mild severity in the main group (n=54)
 |
| |
|
In total, 18 (21.7%) patients of the study group performed PTCS in the surgical treatment of patients with AHC. Drainage of the gallbladder under ultrasound control was performed through the area of the liver parenchyma in order to seal the canal and prevent leakage of bile into the abdominal cavity.Drainage in all cases was performed with an "umbrella" stylet - a catheter with a "basket" at the end, catheter diameter 4F and 9F.After performing microcholecystostomy, the contents of the gallbladder were completely evacuated, its cavity was washed with saline to a clean discharge, and the drainage was lengthened. The drainage discharge was assessed visually and sent for bacteriological examination. The completeness of the emptying of the cavity of the gallbladder was controlled echographically.In this study group, EPST was performed in only 27 patients. At the same time, 15 patients without a clinic of destructive cholecystitis underwent EPST and NBD at the first stage. In 12 patients with a prevalence of acute destructive cholecystitis, this intervention was performed after PTCS. At the same time, it should be noted that in 9 patients, attempts at EPST and installation of NBD were unsuccessful, and in one case, the patient developed acute pancreatitis with a fatal outcome.Thus, 2-stage surgical treatment was performed in 33 patients of the study group, which amounted to 39.7%. These patients, after preliminary minimally invasive decompression of the biliary tract, underwent CE at the second stage on days 7-12, moreover, 22 - LCE, 11 - MLCE, and in 6 of them, MLCE was supplemented with choledocholithotomy.In 50 (60.3%) patients of the study group, a radical operation - CE and choledocholithotomy was performed both from a wide laparotomic approach in 17 patients with a combination of AHC with acute destructive cholecystitis and peritonitis, and from a minilaparotomic approach in 33 patients. Thus, LC was performed in 22 (26.5%) patients, CE from mini-access 44 (53%), CE from wide laparotomy access 17 (20.5%).All surgical interventions in the main group of patients were completed with drainage of the choledochus, of which 56 (67.5%) had external drainage, and 27 (32.5%) had NBD with endoscopic transduodenal intervention.
4. Results and Its Discussion
In the study group, postoperative complications developed in 10 patients, which amounted to 12.1%. At the same time, bilomas of the subhepatic region formed in 3 (3.6%) patients who were successfully sanitized by ultrasound-guided punctures. In 2 (2.4%) patients there was cholemic bleeding from the liver from the area of transhepatic puncture of the gallbladder. External bile leakage was observed in 2 patients, during relaparoscopy, in 1 case, a failure of the cystic duct stump was detected, which was repeatedly clipped, in another 1 case, the gallbladder bed was coagulated as a source of bile leakage into the abdominal cavity. Duodenal bleeding was noted in 1 patient after EPST, the bleeding was stopped. In 1 patient, a subdiaphragmatic abscess was formed, sanitized by repeated punctures under ultrasound control. In 3 patients suppuration of the postoperative wound was observed.Died 2 out of 83 operated patients, mortality was 2.4%. The reason for the poor outcome was acute pancreatitis as a complication of transduodenal endoscopic intervention in 1 patient and ongoing peritonitis in 1 case.Thus, a differentiated approach in the surgical treatment of patients with acute cholecystitis and choledocholithiasis using minimally invasive decompressive interventions contributed to the early relief of cholangitis, the prevention of liver abscesses and the development of biliary sepsis. Achieved a decrease in purulent - septic complications from 24.5% to 12.1%, mortality from 8.2% to 2.4%.
5. Conclusions
1. Staged surgical treatment of patients with acute cholecystitis and choledocholithiasis, taking into account the severity of acute purulent cholangitis and the use of preliminary decompressive interventions on the bile ducts, made it possible to stop the phenomena of cholestasis and purulent intoxication, improve the results of radical operations. At the same time, 81.8% of patients with severe, 61.6% of moderate severity and 24.1% with mild severity of acute purulent cholangitis needed to use diapeutic and endoscopic transduodenal interventions.2. Differentiated use of minimally invasive methods of surgical treatment of patients with acute cholecystitis and choledocholithiasis complicated by acute purulent cholangitis contributed to the improvement of treatment results due to early relief of cholangitis, prevention of liver abscess formation and development of biliary sepsis. Achieved a decrease in postoperative purulent - septic and cholemic complications up to 12.1%, mortality up to 2.4%.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
References
| [1] | Abdurakhmanov D.Sh. et al. Analysis of surgical treatment options for different types of Mirizzi syndrome // Bulletin of science and education. – 2021. – №. 5-1 (108). – P. 71-76. |
| [2] | Abdurakhmanov D.Sh. et al. Biliary peritonitis as a complication of chronic calcular cholecystitis // Bulletin of science and education. – 2021. – №. 5-1 (108). – P. 77-80. |
| [3] | Akhmedov B. A. et al. Surgical approach to the treatment of patients with posttraumatic scar structures of the main bile ducts // VolgaMedScience. – 2021. – P. 341-342. |
| [4] | Aliev Yu.G. Minimally invasive interventions in the surgical treatment of complications of cholelithiasis / Yu. G. Aliev // Surgery. Journal them. I.I. Pirogov. - 2013. - N 5. - S. 73 -75. |
| [5] | Borisov A.E. Ways to optimize the standards for the treatment of acute cholecystitis / A.E. Borisov, V.A. Kashchenko, K.G. Kubachev // Bulletin of Surgery. I.I. Grekov. –2012. - N 6. - S. 80-85. |
| [6] | Cao J. Risk factors for post-ERCP cholecystitis: a single-center retrospective study / J. Cao, C. Peng, X, Ding [et al.] // BMC Gastroenterol. – 2018. – N 18(1). – P. 128. |
| [7] | Deo K. Laparoscopic Choledochotomy in a Solitary Common Duct Stone: A Prospective Study / K. Deo, S. Adhikary, S. Khaniya, V. Shakya, C. Agrawal // Minim Invasive Surg. - 2018. - P. 5. |
| [8] | Galperin E.I., Akhaladze G.G., Vetshev P.S., Dyuzheva T.G. A differentiated approach to the use of minimally invasive methods for the treatment of neoplastic obstructive jaundice // Annals of Surgical Hepatology. - 2019. - T. 24. - No. 2. - S. 10-24. |
| [9] | Gomi H. Tokyo Guidelines 2018: antimicrobial therapy for acute cholangitis and cholecystitis / H. Gomi, J. Solomkin, D. Schlossberg, K. Okamoto, T. Takada, S. Strasberg, M. Yamamoto // Journal of Hepato- Biliary-Pancreatic Sciences. – 2018. – N 25(1). – P. 3-16. |
| [10] | Hanau L. Acute (ascending) cholangitis / L. Hanau, N. Steigbigel // Infect Dis Clin North Am. - 2020. - N14 (3). – P. 521-546. |
| [11] | Kasymov S. Z., Davlatov S. S. Hemoperfusion as a method of homeostasis protection in multiple organ failure syndrome // Academic Journal of Western Siberia. – 2013. – Т. 9. – №. 1. – P. 31-32. |
| [12] | Khadzhibaev F.A. Role and place of minimally invasive endobiliary interventions in purulent cholangitis // Bulletin of emergency medicine. – 2018. – no. 3. |
| [13] | Kharbutli B. Management of preoperatively suspected choledocholithiasis / B. Kharbutli, V. Velanovich // Gastrointest. Surg. - 2018. |
| [14] | Korolkov A.Yu., Popov D.N., Kitaeva M.A., Tantsev A.O., Teplov V.M., Bagnenko S.F. Cholangitis and biliary sepsis on the background of cholecystocholedocholithiasis. Criteria for diagnosis, therapeutic tactics in the hospital emergency department // Ambulance. - 2018. - T. 19. - No. 1. - S. 31-35. |
| [15] | Kurbaniyazov Z. B. et al. Surgical treatment of patients with intraoperative damages of the main cholic ducts // Academic Journal of Western Siberia. – 2013. – Т. 9. – №. 1. – P. 32-32. |
| [16] | Nazirov F.G., Akilov Kh.A., Akbarov M.M. Tactics of treatment of patients with obstructive jaundice complicated by cholangitis and liver failure // Annals of surgical hepatology. - 2011. No. 2. S. - 117-118. |
| [17] | Rakhmanov K. E. et al. The treatment of patients with major bile duct injuries // Academic Journal of Western Siberia. – 2013. – Т. 9. – №. 1. – P. 33-34. |
| [18] | Saydullaev Z. Y. et al. Minimally invasive methods of treatment of patients with acute cholecystitis //Annals of the Romanian Society for Cell Biology. – 2021. – P. 1956-1961. |
| [19] | Shapovalyants S.G. Complicated choledocholithiasis is the result of belated surgical treatment of gallstone disease / S.G. Shapovalyants, T.B. Ardasenov, A.G. Pankov, S.A. Budzinsky, V.S. Veselova // Russian Journal of Gastroenterology, Hepatology, Coloproctology. - 2013. - N 4. - S. 15-21. |
| [20] | Vetshev P.S. Ways to improve the results of surgical treatment of patients with obstructive jaundice / P.S. Vetshev // Annals of the surgeon. hepatology. - M., 2014. - 198 p. |
| [21] | Zagidullina G.T. Modern technologies in the diagnosis of choledocholithiasis / G.T. Zagidullina, A.I. Kurbangaleev // Practical medicine. - 2015. - N 4-2(89). – C. 45-49. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML