-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(9): 897-899
doi:10.5923/j.ajmms.20221209.09
Received: Aug. 15, 2022; Accepted: Aug. 29, 2022; Published: Sep. 15, 2022

Minimally Invasive Technologies in the Correction of Intraoperative Bile Ducts Injuries
Kadirov Rustam Nadirovich, Nurillaev Hasan Jamshidovich, Yarashev Sultonbek Saloxiddinovich, Abdukadirov Ulug’bek Qaxramonovich
Samarkand Branch of the Republican Scientific Center for Emergency, Medical Care
Correspondence to: Kadirov Rustam Nadirovich, Samarkand Branch of the Republican Scientific Center for Emergency, Medical Care.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The paper analyzes the results of surgical treatment of 3266 patients for various forms of cholelithiasis. Bile leakage in the postoperative period was observed in 34 patients due to damage to the peripheral bile ducts (aberrant hepatocystic ducts of the gallbladder bed - Luschka passages, leakage of the cystic duct stump, dislocation of the installed drainage in the hepaticocholedochus). The developed surgical tactics, based on the data of ultrasound and RPCH, can improve the results of treatment and avoid laparotomy in 94.2% of patients with bile leakage from the peripheral bile ducts.
Keywords: Cholecystectomy, Bile leakage, Surgical tactics
Cite this paper: Kadirov Rustam Nadirovich, Nurillaev Hasan Jamshidovich, Yarashev Sultonbek Saloxiddinovich, Abdukadirov Ulug’bek Qaxramonovich, Minimally Invasive Technologies in the Correction of Intraoperative Bile Ducts Injuries, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 897-899. doi: 10.5923/j.ajmms.20221209.09.
Article Outline
1. Relevance
- The leading place in the structure of postoperative complications after cholecystectomy (CE) is occupied by external or intra-abdominal bile leakage (BI) in the early postoperative period, which should be considered as an independent problem, since it can have serious consequences and be life-threatening [1,2,3,10,11,14,16,17]. The main causes of postoperative GI are damage to the peripheral bile ducts (aberrant hepatocystic ducts of the gallbladder bed - Luschka's ducts, leakage of the cystic duct stump) and "large" - iatrogenic damage to the main bile ducts [5,19,21].The outflow of bile through the drainage contributes to the early diagnosis of biliary complications, but even a small bile leakage into the abdominal cavity can lead to serious complications [4,6,7,13,20]. Diagnosis of intra-abdominal bile leakage is a difficult task, the presence of safety drainage in the subhepatic space contributes to early diagnosis and prevention of biliary peritonitis [8,9,12,15,18].
2. Purpose of the Study
- To improve the results of surgical treatment of patients with cholelithiasis (GSD) who developed external or intra-abdominal GI by standardizing the indications and technical improvement of the use of relaparoscopy, transduodenal endoscopic interventions, ultrasound-guided puncture methods to reduce the number of repeated laparotomic operations.
3. Materials and Methods
- The analysis of the results of surgical treatment of 3266 patients operated on in the period 2012-2021 was carried out. regarding various forms of cholelithiasis, which underwent CE: - laparoscopic access - 1947, mini-access - 1093, wide laparotomy - 216.The diagnostic program included a standard general clinical examination, ultrasound, endoscopy, according to the indications of ERCP, MSCT, MRCP. All interventions were completed by draining the abdominal cavity with one or two drains.In the early postoperative period, 49 patients had FI. Women - 37, men - 12, the average age of patients was 49±5.1 years. In 34 patients, the cause of VE was peripheral damage, in 15 - damage to the main bile ducts. The cause of bile leakage in 34 (69.3%) patients (i.e., in more than 2/3 of cases) was damage to the peripheral bile ducts - aberrant hepatic - cystic ducts of the gallbladder bed (Lushka's passages) - 8, failure of the stump of the cystic duct - 6 and dislocation of the established drainage in hepaticocholedochus - 3. However, in 17 patients, the source was not identified due to independent cessation of bile leakage. This study did not include patients with iatrogenic lesions of the main bile ducts.
4. Results and Discussion
- GI was observed in 16 (47.1%) patients operated on for chronic cholecystitis and in 18 (52.9%) patients with acute cholecystitis. In 22 patients, the flow of bile through the drainage was noted, and in 12 patients, the accumulation of bile in the abdominal cavity was diagnosed according to ultrasound data.To assess postoperative GI, we took into account both the daily flow of bile from the abdominal cavity drains and ultrasound data - we determined the volume of delimited fluid accumulation in the projection of the removed gallbladder bed, as well as the localization and volume of free fluid in the abdominal cavity.In 24 patients with GI with bile discharge through the drainage in a volume of 150-200 ml per day and in the absence of signs of peritonitis, a satisfactory condition of patients, no changes in blood tests, dynamic monitoring was performed with obligatory ultrasound control and conservative treatment (antispasmodics, infusion, anti-inflammatory and antibacterial therapy). In 9 patients, the treatment was effective, bile leakage through the drainage progressively decreased and completely stopped within 5-7 days, so no other diagnostic and therapeutic procedures were required.3 patients required punctures of the biloma under ultrasound control in order to evacuate the accumulation of fluid in the subhepatic space, and in 1 patient the cause of bile leakage was the loss of drainage from the choledochus (Fig. 1).
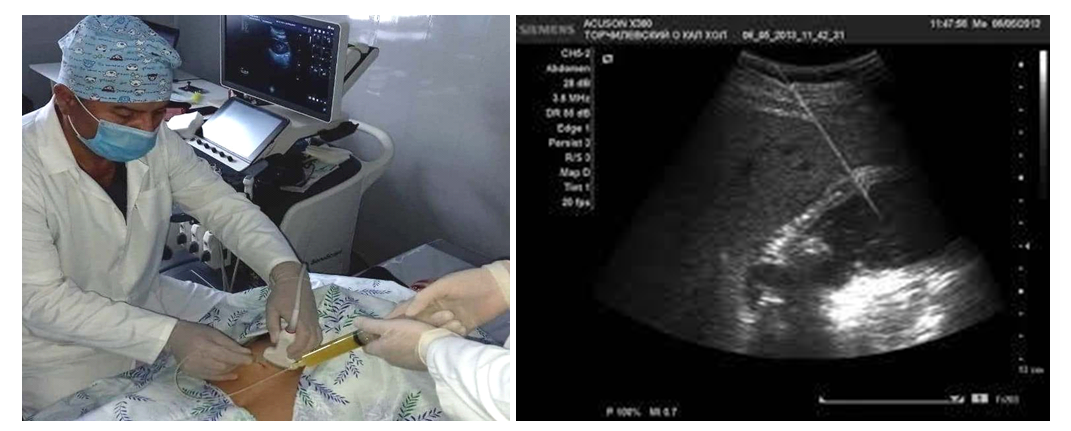 | Figure 1. Puncture of the Biloma under ultrasound control |
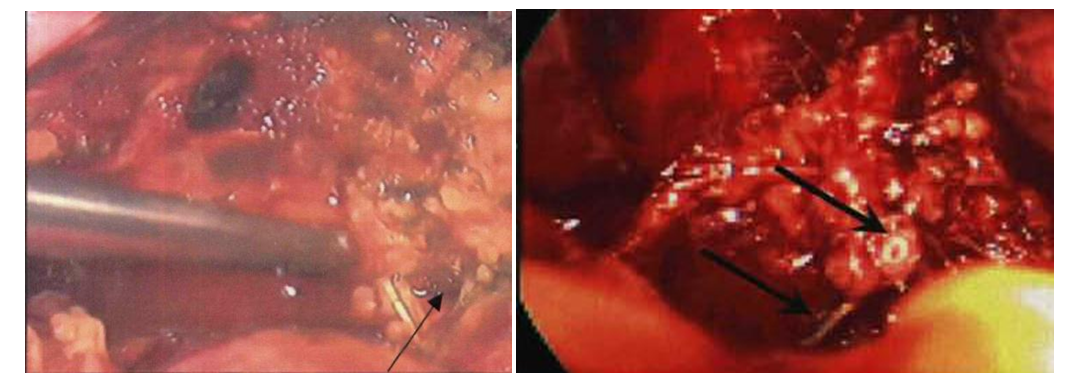 | Figure 2. Relaparoscopy, additional clipping of the cystic duct stump |
5. Conclusions
- 1. Ultrasound examination contributes to the choice of adequate surgical tactics for bile leakage.2. With the appearance of bile discharge through the control drainage in a volume of not more than 200 ml per day with a tendency to decrease and the absence of accumulation of bile intraperitoneally and the clinic of bile peritonitis, conservative therapy can be limited.3. The use of minimally invasive endoscopic transduodenal interventions, diapeutical methods and relaparoscopy, as well as active conservative therapy allowed patients with peripheral bile duct injuries after CE to avoid laparotomy in 94.2% of patients.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML