-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(8): 806-808
doi:10.5923/j.ajmms.20221208.07
Received: Jul. 9, 2022; Accepted: Aug. 10, 2022; Published: Aug. 15, 2022

Histopathology in Primary Atelectasis in Infants and Risk Factors
Zebo I. Ruzieva
Assistant of Department of Physicians the Tashkent Academy of Medicine, Tashkent, Uzbekistan
Correspondence to: Zebo I. Ruzieva, Assistant of Department of Physicians the Tashkent Academy of Medicine, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Primary atelectasis of the lungs “enters the respiratory distress syndrome and occurs in the form of a separate nosological unit. This article examines the specific pathomorphological features of primary pulmonary atelectasis. As material, the lungs of infants who died of atelectasis in the neonatal period were studied microscopically. Microscopic examination revealed that the lung tissue had an underdeveloped appearance at a glance. Alveolar interstitial tissue is composed of dense connective tissue and cell clots, the blood vessels are wide and full, surrounded by a hemorrhagic structure. If primary atelectasis develops 2-3 days before infant death, inflammation of the lung tissue is observed, ie macrophages, neutrophils, migrating alveocytes are detected in the alveolar cavity. After 7-10 days, it is determined that the alterative-proliferative processes are exacerbated and turn into atelectatic pneumonia. It results in pneumosclerosis, bronchiectasis, and the development of retinal cysts of the bronchi. Often, connective tissue grows in place of atelectasis and sclerosis develops.
Keywords: Infant, Lung, Distress syndrome, Primary atelectasis
Cite this paper: Zebo I. Ruzieva, Histopathology in Primary Atelectasis in Infants and Risk Factors, American Journal of Medicine and Medical Sciences, Vol. 12 No. 8, 2022, pp. 806-808. doi: 10.5923/j.ajmms.20221208.07.
1. Introduction
- The urgency of the problem. Respiratory disorders account for 8.8% of infantile diseases, ranking 2nd, and are more common in premature infants due to the morphofunctional characteristics of the respiratory system. In particular, respiratory distress syndrome in infants is generally 6-12%, in premature infants - 1-1.8%, in very low birth weight infants - 0.4-0.5% [2,4]. The main reasons for the development of this disease are the lack of internal surfactant in the lungs of infants, the weakness of the respiratory muscles and the inability to breathe independently. In the foreign scientific literature, the terms "respiratory distress syndrome" and "primary atelectasis of the lungs" are synonymous and develop in the form of a separate nosological unit. The clinical differential diagnosis of these infantile lung diseases is very difficult. Primary atelectasis from respiratory disorders is a direct cause of infant mortality in pathological examinations. Primary atelectases and hyaline membranes are the most common morphofunctional forms of respiratory disorders in preterm infants. The main risk factors are intranatal aspiration of amniotic fluid, damage to the alveolar epithelium and increased capillary wall permeability [1,3].
2. Result and Discussion
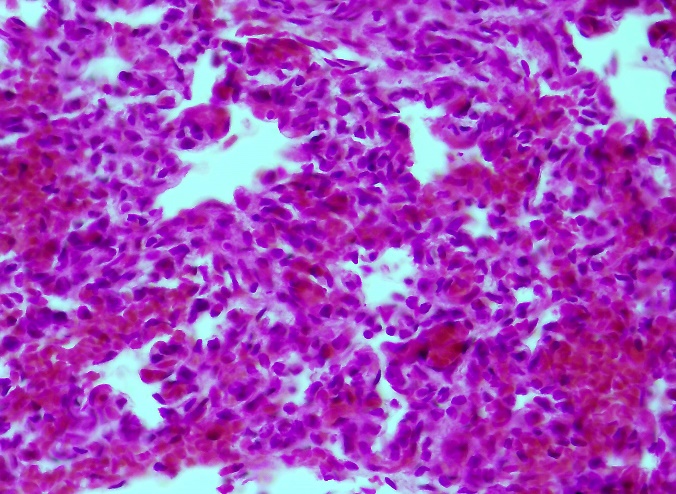
- The results of the microscopic examination showed that when the lung tissue is seen under a small lens of the microscope, it is determined at a glance that it has an underdeveloped appearance. In lung tissue, only the bronchi and bronchioles are found to have a tubular structure of varying size, indeterminate shape. The reticular appearance of the alveolar tissue is indistinguishable. Respiratory alveoli and their interconnected cavities are not identified. The interstitial alveolar tissue consists of densely packed tissue and cellular tufts joined together (Fig. 1). In such a dense lung tissue, the blood vessels are wide and full, with a structure around which blood flows.
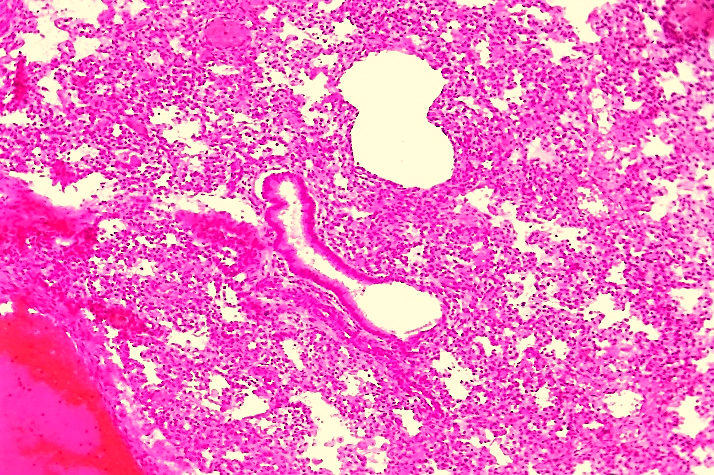 | Figure 1. Alveolar interstitial tissue is formed from dense tissue and cellular tufts that are fused together. Paint: G-E. X: 10x10 |
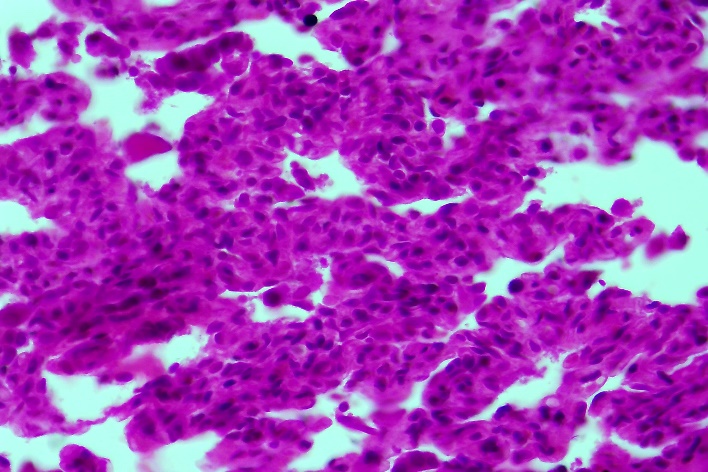
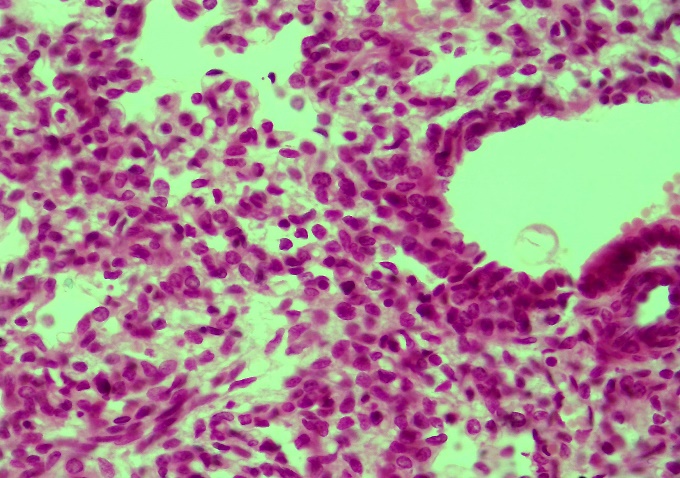 | Figure 2. Primary atelectasis foci are found to be dense and composed of tissue without alveolar cavities. Paint: G-E. X: 10x40 |
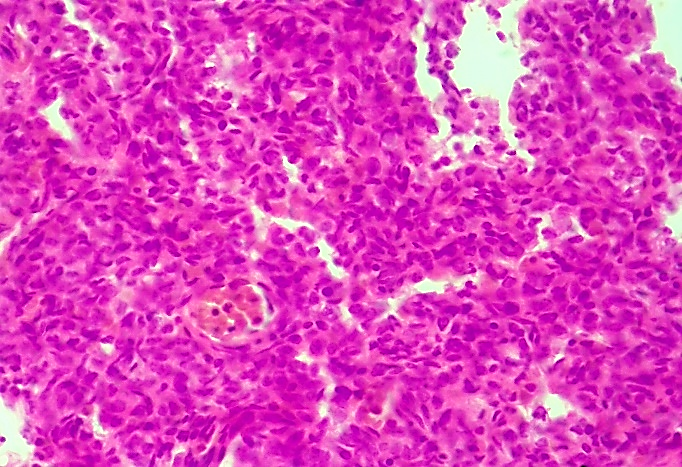
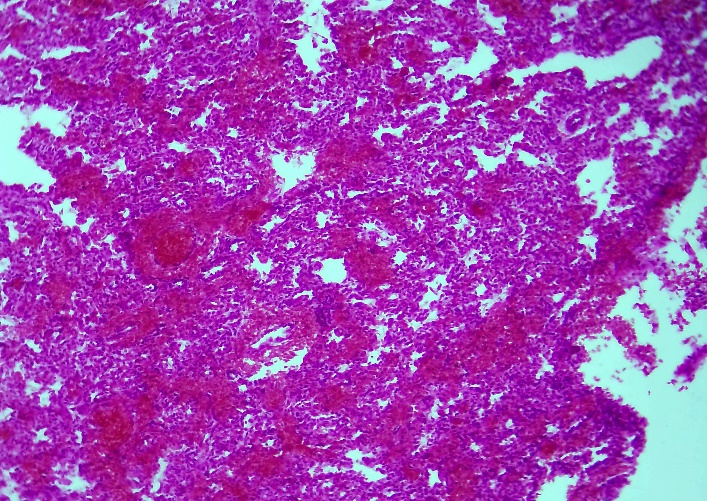 | Figure 3. Primary atelectasis resulted in vascular occlusion and massive hemorrhage in the lung tissue. Paint: G-E. X: 10x40 |
 | Figure 4. In the unformed lung tissue, the vessels dilate, and massive blood is infused into most areas. Paint: G-E. X: 10x40 |
 | Figure 5. Hypertrophy of proliferative inflammatory histiocytic cells between the alveoli, the formation of dense proliferative inflammatory infiltrate. Paint: G-E. X: 10x40 |
 | Figure 6. Growth of connective tissue in alveolar tissue, i.e., the appearance of sclerotic tumors. Paint: G-E. X: 10x40 |
3. Conclusions
- 1. Infantile pulmonary atelectasis is referred to as “respiratory distress syndrome (NBS)” and its incidence is 1% of all infants and 14% of preterm infants. The urgency of the problem of atelectasis for pediatrics lies in the large number of causes of pulmonary alveolar tissue collapse in infants at one month of age.2. Microscopic examination reveals that the lung tissue has an underdeveloped appearance at a glance. In lung tissue, only the bronchi and bronchioles appear in a tubular structure of varying size, indeterminate shape. The reticular appearance of the alveolar tissue is indistinguishable. Respiratory alveoli and their interconnected cavities are not identified.3. It is observed that the interstitial tissue of the alveoli consists of dense tissue and cellular tufts connected to each other, the blood vessels are wide and full, having a structure around which blood flows.4. If the primary atelectasis develops 2-3 days before the death of infants, the development of inflammation in the lung tissue is observed, that is, macrophages, neutrophils, migrating alveocytes are detected in the alveolar cavity.5. After 7-10 days it is determined that the alterative-proliferative processes are exacerbated and turn into atelectatic pneumonia. It results in pneumosclerosis, bronchiectasis, and the development of retinal cysts of the bronchi. Often, connective tissue grows in place of atelectasis and sclerosis develops.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML