-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(8): 802-805
doi:10.5923/j.ajmms.20221208.06
Received: Jul. 23, 2022; Accepted: Aug. 5, 2022; Published: Aug. 15, 2022

Determinants of Post-Operative Complications in Patients with Ventral Hernia: Retrospective Cohort Study
Saidmurad Ibragimovich Ismailov1, Safarboy Tukhtabaevich Khujabaev2, Murodulla Isomiddinovich Rustamov2, Qodir Usmankulovich Sherkulov2, Inoyatullo Murodullaevich Rustamov2
1Republican Specialized Scientific and Practical Medical Centre on Surgery after V. Vahidov, Tashkent, Uzbekistan
2Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: Safarboy Tukhtabaevich Khujabaev, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

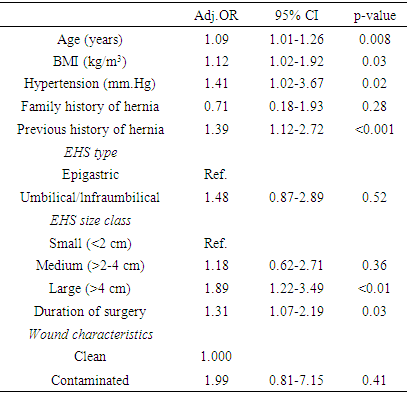
Surgical treatment of ventral hernia is associated with complications, but no apparent risk factors were described. We evaluated potential predictors of 1-month postoperative complications after hernioplasty using the patients' database of the 1st Clinic of Samarkand State Medical Institute.We conducted a prospective cohort study. All included patients underwent ventral surgery on repairment of ventral hernia in the 1st Clinic of Samarkand State Medical Institute between January 1, 2014, and January 1, 2021. We performed logistic regression analyses to identify risk factors. In this study, we included 348 patients, of whom 87 (25%) patients had more than one complication within 1-month after surgery. According to the multivariable logistic regression analysis, older age was associated with slightly increased odds of postoperative problems (OR=1.09; 95% CI, 1.01-1.26, p<0.01). Furthermore, patients with BMI over 25 kg/m3 were more likely to experience post-hernioplasty complications (OR 1.12; 95% CI, 1.02-1.92, p=0.03). Interestingly, larger size of hernia (OR 1.89; 95% CI, 1.22-3.49, p<0.01) and previous history of hernia surgery (OR 1.39; 95% CI, 1.12-2.72, p<0.001) were associated with relatively higher risk of postoperative complications compared to other variables. Lastly, as longer surgery last as more likely experience postsurgical complications (OR 1.31; 95% CI, 1.07-2.19, p=0.03). Age, BMI, hypertension, previous history and size of hernia, and duration of surgery were associated with complications. Clinicians should take into account the patient's age, BMI and high blood pressure as the potentially important preoperative examination factors in individuals with a primary hernia.
Keywords: Ventral hernia, Complications, Risk factors, Age, BMI, Hypertension
Cite this paper: Saidmurad Ibragimovich Ismailov, Safarboy Tukhtabaevich Khujabaev, Murodulla Isomiddinovich Rustamov, Qodir Usmankulovich Sherkulov, Inoyatullo Murodullaevich Rustamov, Determinants of Post-Operative Complications in Patients with Ventral Hernia: Retrospective Cohort Study, American Journal of Medicine and Medical Sciences, Vol. 12 No. 8, 2022, pp. 802-805. doi: 10.5923/j.ajmms.20221208.06.
Article Outline
1. Introduction
- The treatment of ventral hernia (VH) continues to be a problem for general practitioners, surgeons and patients. There is a wide variation in the treatment of VHs in such patients. Even under optimal conditions, VH occurs in up to 30% of patients who had any abdominal surgery [1, 2]. Some studies report high rates of hernia recurrence (from 24% to 43%), even when a mesh is used during primary hernioplasty. Hernial recurrence is associated with the increased cost of treatment and elevated morbidity in patients with a high risk of multiple plastic surgeries [3]. The European Hernia Society (EHS) classifies ventral hernias by type and size. This classification was developed to create a unique method of scientific and clinical description of hernias [4]. It represents the perceived risk of complications and recurrence after primary hernioplasty. Despite the wide availability of the EHS classification, it has not yet undergone rigorous external validation.Recent studies demonstrated that over 10% of all patients experienced short- or long-term complications that occurred after primary hernioplasty. Additionally short and longr term complications were in correlation with the frequency of patient readmission [5-7]. It is also hypothesized that a history of postoperative adhesion may lead to post-surgery complications of primary hernia repair [8-9]. This finding demonstrates how important it is to identify potential risk factors for postoperative complications of ventral hernia. The present study aimed to evaluate potential predictors of 1-month post-hernioplasty complications using the patients' database of 1st Clinic of Samarkand State Medical Institute.
2. Materials and Methods
- We performed a clinic-based, retrospective cohort study. Patients who underwent primary ventral hernia surgery in 1st Clinic of Samarkand State Medical Institute were included between January 1, 2014, and January 1, 2021. All the data was extracted from the central patients' registry of the clinic. Personal data were anonymized and approval from Samarkand State Medical University ethical review board was obtained. Patient demographic characteristics such as age, sex, body mass index (BMI), and smoking habits were taken from the registry of the hospital. Data on clinical characteristics included diabetes mellitus, COPD, hypertension, previous corticosteroid use and chemotherapy, connective tissue disorders, anticoagulants use or coagulopathies. Also, for the purpose of analysis, we collected data on the previous history of hernias and hernia characteristics such as location, width, length, and class by EHS classification. Data was grouped different features of hernia surgeries performed (open or laparoscopic, emergency surgery, the technique of mesh placement and duration).We used R studio 3.6.2 for all statistical analyses. We used Kolmogorov–Smirnov criteria to test the distribution of continuous variables. Mean values with corresponding standard deviations (SDs) were presented for continuous variables and absolute numbers with corresponding percentages were presented for categorical variables. We used the Mann-Whitney U test for continuous variables and the chi-square test for categorical data to compare risk factors. Fisher exact test was utilized in case of a small number of groups. Clinically significant factors and potential risk factors associated with postoperative complications in the univariate analysis (with p-value of <0.05) were included in the multivariate regression analysis.
3. Results
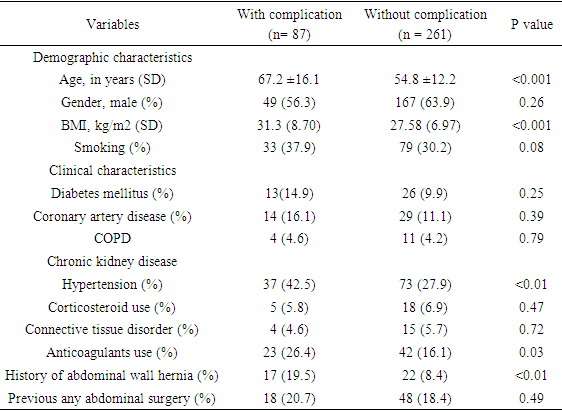
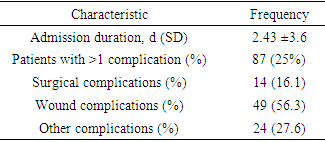
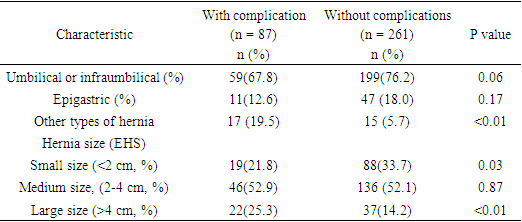
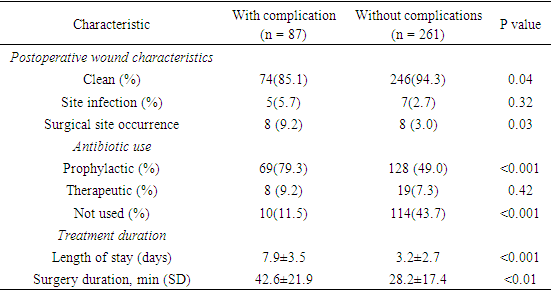
- A total of 348 surgically treated patients with primary ventral hernia were included in the study. The baseline characteristics of the patients are shown in table 1. According to the results, patients with postoperative complications were older (67.2 ± 16.1 years vs 54.8 ± 12.2, p<0.001). Higher BMI was also observed among patients with postoperative complications (31.3 ± 9.6 kg/m2 vs 25.1 ± 8.6 kg/m2, p<0.001). More patients with postoperative complications had hypertension (42.5% vs 27.9% p<0.01) and previous history of abdominal hernia (19.5% vs 8.4%, p<0.01). Anticoagulant use was also statistically significant (26.4% vs 16.1%, p<0.001). We found no significant association in patient characteristics.
|
|
|
|
|
4. Discussion
- This study shows that patient characteristics such as age, BMI, hypertension, previous history and size of hernia, as well as the surgery duration were found to be the risk factors for post-hernioplasty complications at one month.In contrast to previous studies, our analysis showed that larger hernia size correlated with a higher incidence of postoperative complications, which could be explained by the relatively high number of patients with complications in this study.The most significant correlation was seen between BMI and surgical complications. This link has been proven in the previous studies [6-8], and it is essential for determining the patient's status before the operation, even though the precise mechanism behind this relationship is unknown [9-10]. Patients should be informed about potential risks and encouraged to lose weight prior to hernia surgery. Patients who have postoperative difficulties often have longer operation times and remain in the hospital for more extended periods of time.Although a family history of hernia, a medium-sized hernia, and a postoperative wound infection were all anticipated to be related to problems, these factors were not shown to be significantly different in this research [2,6,7,10]. These results may have several plausible explanations, one of which is that the incidence of postoperative complications is relatively low, which indicates the possibility that some of these characteristics may turn out to be associated with postoperative complications in subsequent studies with bigger cohorts.There is a possibility of bias in patient selection due to the use of the patients' registry in this research. In addition, this cohort includes patients who have had surgery performed by many general surgeons, resulting in the possibility of varying levels of skill and a variety of approaches to the technical aspects of the procedure.
5. Conclusions
- Age, BMI, hypertension, prior history and size of hernia, as well as the length of operation, are significantly linked with postoperative problems following VH surgery. We observed no statistically significant correlation between the hernia size and surgical complications. Clinicians should take into account the patient's age, BMI and high blood pressure as the potentially important preoperative examination factors in individuals with a primary hernia. Postoperative complications may lead to increased spendings for patients and the hospital as it might necessitate extended operation length and hospital stays.
ACKNOWLEDGEMENTS
- The authors express gratitude to Khasan Ibragimov for the help in manuscript preparation and translation into English.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML