-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(7): 748-752
doi:10.5923/j.ajmms.20221207.13
Received: Jun. 15, 2022; Accepted: Jul. 6, 2022; Published: Jul. 15, 2022

Сare Clinical Decision-Making Tool for Diagnosing and Managing Chronic Instability of the Shoulder Joint
M. E. Irismetov1, S. A. Zhongirov2, B. V. Soleev2, D. Sh. Mansurov3, Shirov B. F.3
1Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Tashkent, Republic of Uzbekistan
2Samarkand Branch of the Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Samarkand, Republic of Uzbekistan
3Samarkand State Medical University, Samarkand, Republic of Uzbekistan
Correspondence to: D. Sh. Mansurov, Samarkand State Medical University, Samarkand, Republic of Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

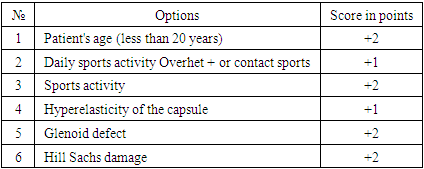
This article describes the treatment patients with chronic instability of the shoulder joint need a reliable diagnosis, and based on the identified pathological process of the shoulder joint, it is necessary to choose the tactics of surgical treatment. The purpose of the study is to substantiate the developed algorithm for choosing the tactics of diagnosis and surgical treatment of chronic instability of the shoulder joint. Based on the analysis of the main and current approaches to the diagnosis and treatment of instability of the shoulder joint, the author's Program for choosing the tactics of surgical treatment of chronic anterior instability of the shoulder joint was developed, which allows you to accurately assess the pathology of the shoulder joint, as well as determine the necessary tactics of surgical treatment. The developed algorithm makes it possible to carry out a minimally costly diagnostic procedure and choose the least traumatic and most anatomical method of surgical intervention.
Keywords: Chronic instability of the shoulder joint, Treatment and diagnostic algorithm, ISIS instability index, HS on track / off track lesion
Cite this paper: M. E. Irismetov, S. A. Zhongirov, B. V. Soleev, D. Sh. Mansurov, Shirov B. F., Сare Clinical Decision-Making Tool for Diagnosing and Managing Chronic Instability of the Shoulder Joint, American Journal of Medicine and Medical Sciences, Vol. 12 No. 7, 2022, pp. 748-752. doi: 10.5923/j.ajmms.20221207.13.
Article Outline
1. Introduction
- Shoulder pain is a widespread condition and a major cause of morbidity and functional disability [1]. Some patients experience minor symptoms that last relatively short (ie, less than 3 months) [2]. Other patients show more severe symptoms, lasting for a long time (i.e. more than 12 months), with a chronic course and relapses, which is an actual problem [3,4]. Pain, stiffness and weakness in the shoulder often lead to chronic pain, disability and loss of performance, which affect the quality of life and burden both the patient and society [5,6]. Shoulder pain also results in a financial burden for both the patient and the healthcare system. Direct costs include physician services, additional and related medical procedures, home care, prescription drugs, inpatient and outpatient hospital care, outpatient services, and non-health sector costs [7]. Indirect costs include the cost of lost productivity due to disability as well as the cost of lost earnings [8]. From a health services perspective, shoulder pain is the second most common musculoskeletal (MS) complaint, a complaint at the primary care level, and the third most common site of MS pain in the population [9]. Patients with shoulder pain account for a third of all visits to primary care physicians [2,10]. These patients frequently return for follow-up consultations, further increasing the strain on public health resources. A significant number of patients also go to private health care clinics for shoulder treatment, although this scale becomes a skill challenge due to limitations in public-private communication. However, the prevalence of shoulder pain will only increase as the population ages [5].Patients with shoulder pain need confident assessment, treatment, and appropriate therapies. However, current evidence suggests that many patients with shoulder pain do not receive such care at the primary care level. Instead, the current system suffers from process inefficiencies, overuse of diagnostic tests, inappropriate referrals, and underuse of appropriate therapeutic interventions; all this leads to a long waiting time and poor quality of service [12]. Management of shoulder pain at the primary care level is challenging, as many disorders share similar clinical features and lack consensus on diagnostic criteria and consistency in clinical evaluation [13]. Unfortunately, primary care physicians often lack the necessary training and self-confidence to properly treat shoulder pain. Many primary care physicians are routinely referred for costly investigations such as magnetic resonance imaging (MRI), which are usually unnecessary and do not provide a clear answer to the clinical question [10]. In addition, patients seeking primary health care are often referred to specialized care, resulting in long waiting times for specialist consultations. This is problematic because most patients do not require surgery but are referred to orthopedic surgeons when they could easily be treated at the primary care level with conservative treatment. [12]. Therefore, there is still a certain level of variation and inappropriateness in the treatment of shoulder pain at the primary health care level.Decision making in primary health care is complex and can potentially affect the quality of care provided and patient outcomes. Patient-centered care requires a structured approach that supports evidence-based decision making in primary health care settings. Therefore, the goal of this project is to develop a clinical decision-making tool to standardize care and minimize uncertainty in the assessment, diagnosis, and treatment of patients seeking primary care for shoulder pain. The development of this clinical decision-making tool required two steps: 1) defining evidence-based clinical decision-making tools for shoulder pain; and 2) the creation of an algorithm for the evaluation, diagnosis and treatment of patients with chronic instability of the shoulder joint. This includes consensus on indications for diagnostic imaging and distinction between patients who are eligible for surgical and non-surgical treatment options.
2. Purpose of the Research
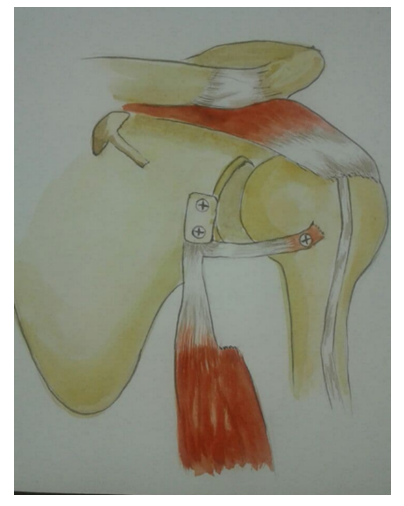
- To substantiate the developed algorithm for choosing the tactics of surgical treatment of chronic instability of the shoulder joint.Based on the analysis of the main and current approaches to the diagnosis and treatment of shoulder joint instability, the author's "Program for choosing the tactics of surgical treatment of chronic anterior shoulder joint instability" (Fig. 1) was developed, which allows to accurately assess the pathology of the shoulder joint, as well as determine the necessary tactics of surgical treatment.
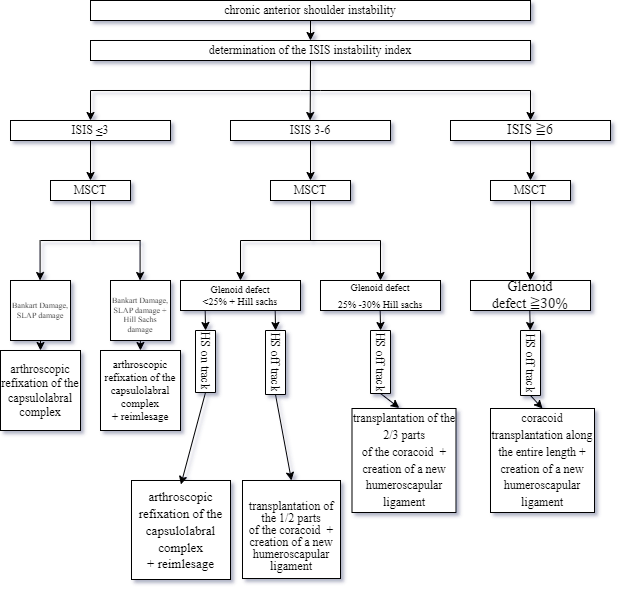 | Figure 1. The program for choosing the tactics of surgical treatment of chronic anterior instability of the shoulder joint |
|
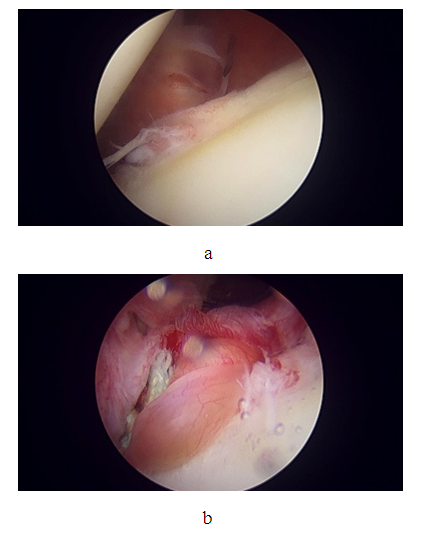 | Figure 2. a - Arthroscopic picture of the Bankart injury, b - arthroscopic picture of refixation of the capsular-labral complex |
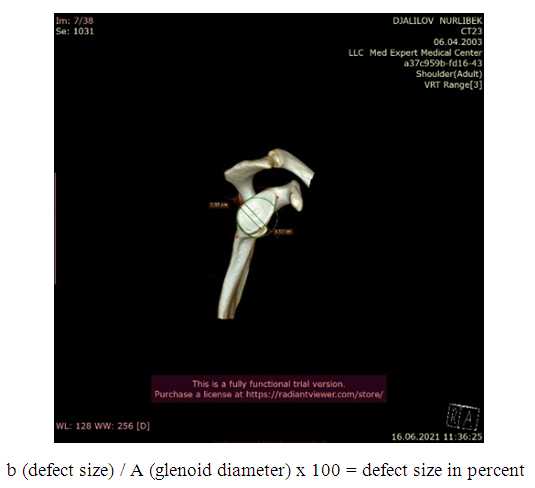 | Figure 3. Estimation of the size of the glenoid defect on a computed tomogram in the 3D reconstruction mode |
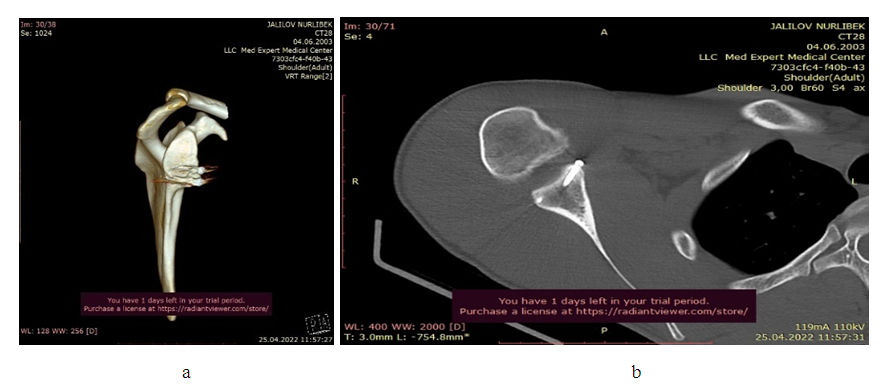 | Figure 5. a, b. Computed tomography of the shoulder joint after glenoid plasty with a bone autograft from ½ of the lateral part of the coracoid process |
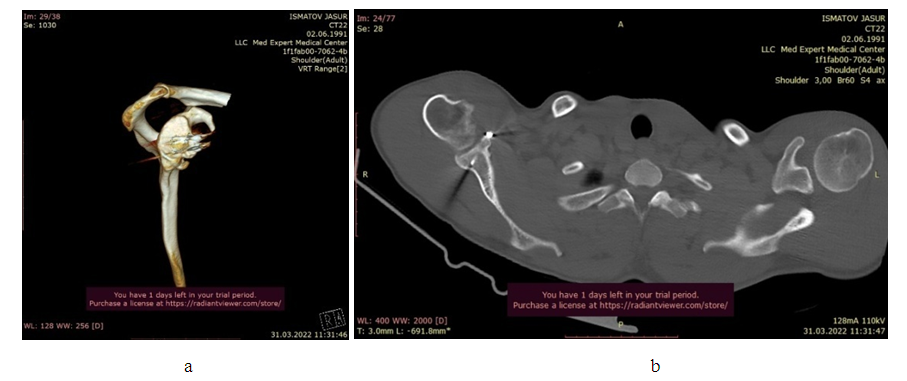 | Figure 6. a, b. Computed tomography of the shoulder joint after plastic surgery of the articular process of the scapula |
3. Discussion of the Obtained Results
- The developed algorithm suggests that a comprehensive preoperative examination to identify underlying and concomitant intraarticular pathology, assess the nature of damage to individual structures, and identify predictors that increase the risk of postoperative recurrence of dislocations is the key to successful restoration of the damaged joint.The result of the implementation of the algorithm is the choice of the least traumatic, most anatomical and, in turn, reliable surgical tactics with the lowest risk of developing biomechanical disorders in the immediate and long-term follow-up periods. The implemented algorithm for diagnostics and surgical intervention in the treatment of anterior instability of the shoulder joint demonstrates the complexity of the approach to this problem. It reflects the modernized tendency to consider shoulder joint surgery as complex, requiring to take into account the variety of structural damage, age, the specifics of physical activity, and to achieve long-term stability of the joint by performing low-traumatic, pathogenetically substantiated operations.
Ethical Aspects
- Ethics committee approval. The study was approved by the ethical committee of the Samarkand State Medical University.
Agreement
- The patients agreed to publish the message and post information on the Internet about the nature of their disease, the treatment performed and its results for scientific and educational purposes.
Financing
- The work was carried out in accordance with the research plan of the Samarkand State Medical University.
Conflict of Interest
- The authors declare no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML