-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(7): 743-747
doi:10.5923/j.ajmms.20221207.12
Received: Jul. 1, 2022; Accepted: Jul. 13, 2022; Published: Jul. 15, 2022

Comparative Evaluation of Treatment Outcomes in Patients with Hypertensive Intracerebral Hemorrhages without and with a Penetration into the Ventricular System
L. B. Maksudova1, B. G. Gafurov2, Sh. R. Mubarakov1
1Republican Research Center of Emergency Medicine
2Center for the Development of Professional Qualifications of Medical Workers
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

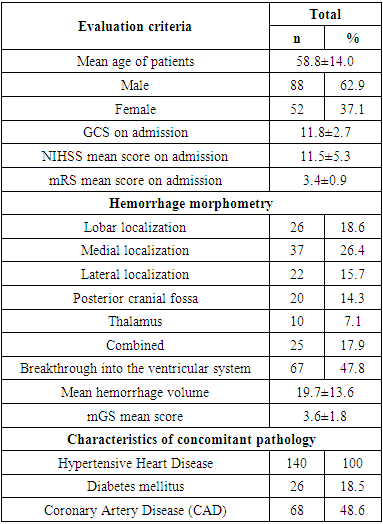
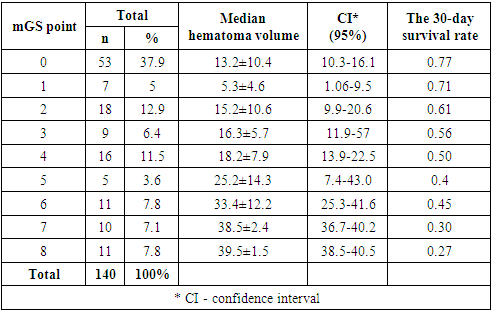
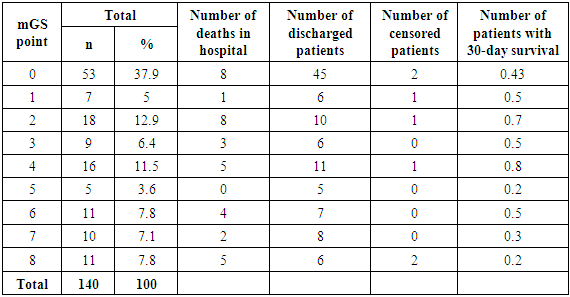
Aim of study was prediction of 30-day survival and 90-day functional outcome in patients with hypertensive intracerebral hemorrhages without and with blood penetration into the ventricular system. Material and methods. We conducted a retrospective analysis of 140 patients with hypertensive intracerebral hemorrhages of the brain. There were 52 (37.1%) females and 88 (62.9%) males. The age of patients varied from 15 to 88 years (mean age was 58.8±14.0 years). We used a modified Graeb scale (mGS) and a modified Rankin scale (mRS) to predict the 30-day survival and 90-day functional outcome of patients with hypertensive intracerebral hemorrhages that were not complicated and complicated with intraventricular hemorrhage. To assess the 90-day functional outcome by the mRS scale, patients were conditionally divided into three subgroups depending on the gradation by the mGS scale and the degree of disability by the mRS scale. The 30-day survival rate was estimated using the Kaplan-Mayer method. Results. A comparative assessment of survival in patients depending on the gradation of mGS showed the following results: thus, with mGS <5 points, the 30-day survival averaged 0.63 ± 0.15, and with mGS >5 points, this indicator was 0.3± 0.14. In the subgroup of patients with mGS 0 points, mRS scores from 0 to 3 points were 90.4% and 9.6% - with mRS 4-5 points. In the subgroup of patients with mGS <5, mRS indicators were characterized as follows: so mRS from 0 to 3 points was 74.5%; mRS 4-5 points – 10.6%; mRS 6 points – 14.9%, respectively. In the subgroup of patients with mGS>5, when assessed on the mRS scale, it was noted that mRS from 0 to 3 points was 41.5%, mRS 4-5 points - 41.5% and 6 points - 17.1%, respectively. Conclusion. Patients with hypertensive intracerebral hemorrhages complicated by intraventricular hemorrhage have a significantly increased risk of death and poor functional outcome. Assessment of intraventricular hemorrhage gradation is important in predicting patient survival. The use of the mGS scale in patients with intraventricular hemorrhage allows to differentiate the severity of the patient's condition and predict 30-day survival and 90-day functional outcome.
Keywords: Hypertensive intracerebral hemorrhages, Intraventricular hemorrhage
Cite this paper: L. B. Maksudova, B. G. Gafurov, Sh. R. Mubarakov, Comparative Evaluation of Treatment Outcomes in Patients with Hypertensive Intracerebral Hemorrhages without and with a Penetration into the Ventricular System, American Journal of Medicine and Medical Sciences, Vol. 12 No. 7, 2022, pp. 743-747. doi: 10.5923/j.ajmms.20221207.12.
1. Introduction
- Hypertensive intracerebral hemorrhage (ICH) is one of the urgent problems of modern neurology, the incidence of which is on average 24.6 cases per 100,000 population. Hypertensive ICH accounts for 10-15% of all strokes and is characterized by a 3-month mortality rate in 30-50% of cases [1-4]. In 35-45% of cases, Hypertensive ICH is complicated by a breakthrough of blood into the ventricular system, the so-called intraventricular hemorrhage, which is an independent predictor of unsatisfactory outcome and functional result in 32-43% of cases [5-8]. Based on numerous studies on improving the treatment results of patients with Hypertensive ICH complicated by intraventricular hemorrhage (IVH), it has been established that breakthrough of blood into the ventricular system of the brain is one of the independent factors leading to high mortality rates and unsatisfactory functional outcomes [9-11]. It has been proven that the installation of external ventricular drainage is the method of choice in the treatment of Hypertensive ICH complicated by IVH, which contributes to improving survival rates. However, the conducted meta-analyses proved that the rates of lethality and severe disability remain high to this day. The issues of choosing a treatment method, as well as the role of IVH in Hypertensive ICH and its influence in predicting 30-day survival and 90-day functional outcome in patients with Hypertensive ICH remain debatable. The aim of the study was a prediction of 30-day survival and 90-day functional outcome in patients with hypertensive intracerebral hemorrhages without and with a breakthrough of blood into the ventricular system.
2. Material and Methods
- There were 52 (37.1%) females and 88 (62.9%) males. The age of patients varied from 15 to 88 years (mean age was 58.8±14.0 years). All patients underwent neurological examination and assessment of the condition severity according to the National Institutes of Health Stroke Scale (NIHSS). Impaired consciousness was evaluated using the Glasgow coma scale (GCS). All patients were prescribed computed tomography (CT) after studying the anamnesis of the disease and physical examination. Based on the CT results obtained, we evaluated the following characteristics of intracerebral hemorrhage: localization and volume of the hematoma, the presence of a breakthrough of blood into the ventricular system, the condition of the bypass cistern, deformation or expansion of the ventricular system and its size, displacement of the median structures of the brain, perifocal edema around the hematoma in its presence and secondary brain changes (Tab. 1).
|
|
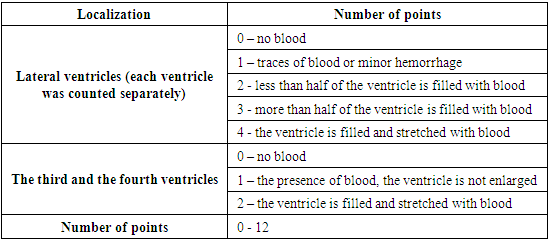
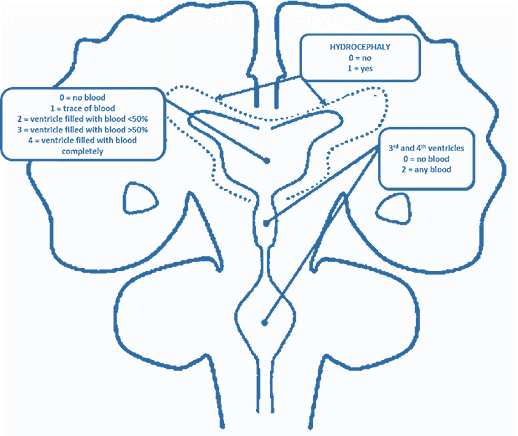 | Figure 1. Scheme for evaluating intraventricular hemorrhages according to the mGS scale |
3. Results
- The results of our study showed that the mean score of patients with Hypertensive ICH on the NIHSS scale was 11.5±5.3 points. When evaluating the level of consciousness by GCS, the mean score made up 11.8 ± 2.7 points. The mean volume of the Hypertensive ICH was 19.7±13.6 cm3. There was an intraventricular breakthrough of blood in 47.8% of cases. The mean mGS score was 3.6±1.8 points. When analyzing the localization of hemorrhage, the following was noted: the medial localization of Hypertensive ICH prevailed, amounting to 26.4% (n=37); in 18.6% (n=26) of cases Hypertensive ICH was localized lobar; there was a mixed localization of Hypertensive ICH in 17.9% (n=25) of cases; lateral localization of Hypertensive ICH was observed in 15.7% (n=22) of cases; in 14.3% (n=20) of cases the Hypertensive ICH was located in the posterior cranial fossa; there was a thalamic location in 7.1% (n=10) of cases. When evaluating the state of hemorrhage on the mGS scale, the following was noted: in 37.9% (n=53) of cases, mGS was 0 points; in 5% (n=7) of cases – 1 point; in 12.9% (n=18) of cases – 2 points; in 6.4% (n=9) of cases 3 points, in 11.5% (n=16) of cases – 4 points; in 3.6% (n=5) of cases – 5 points; in 7.8% (n=11) of cases – 6 points; in 7.1% (n=10) of cases – 7 points and in 7.8% (n=11) of cases mGS was 8 points. Patients with 10-12 points on the mGS scale were not observed in our study (Tab. 3).
|
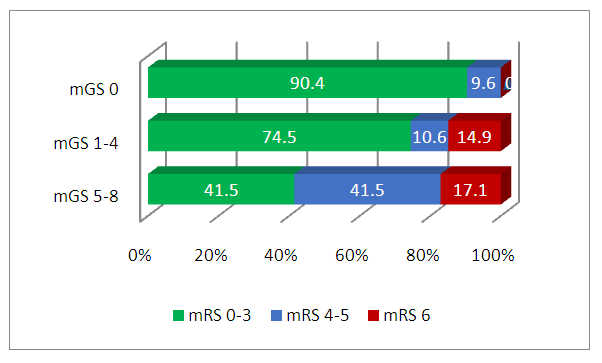 | Figure 2. 90-day functional outcome measure evaluated by the mRS scal, depending on mGS degree |
4. Discussion
- It was noted in the results of Trifan G et al. that mGS >5 points was the most important predictor of poor outcome, and in patients where mGS was <5 points, the outcomes were favorable [3]. Also the data obtained by Hansen B. et al. showed greater variability in Hypertensive ICH patients with IVH as evidenced by patient survival outcomes [8]. For the first time, Tuhrim et al. proved in their studies that IVH volume was associated with lower 30-day survival rates [12]. In the research results of Young et al. it was determined that the threshold volume of IVH 20 ml was a prognostic factor of an unfavorable outcome [13]. Also, in this study, it was proved that even a small volume of IVH, such as 6 ml, negatively affected the 90-day functional result after Hypertensive ICH. Evaluation of the 30-day survival results of patients with Hypertensive ICH with and without IVH showed the best results of 30-day survival in patients with Hypertensive ICH without IVH. In a comparative evaluation of survival in patients, depending on the gradation of mGS, the following results were noted: for example, with mGS <5 points, the 30-day survival averaged 0.63±0.15, and with mGS >5 points, this indicator was 0.3± 0.14 (Tab. 4 and Fig. 3).
|
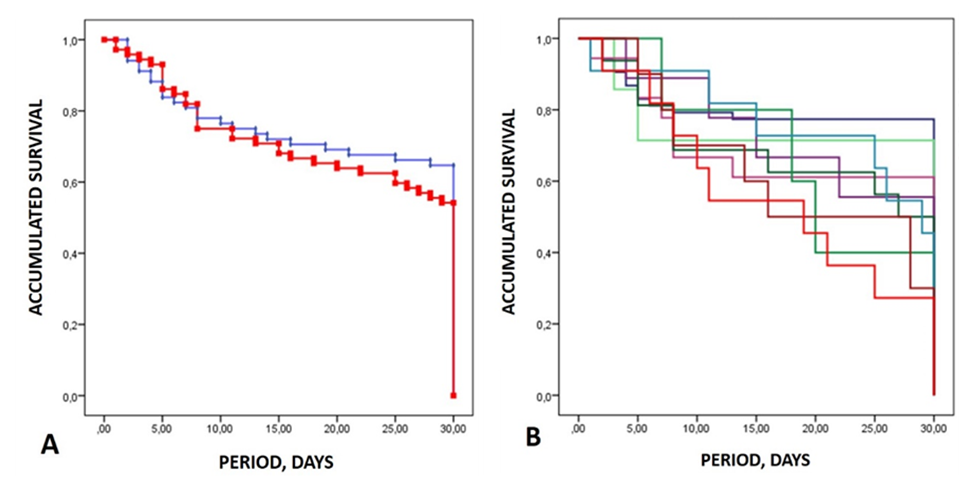 | Figure 3. А – 30-day survival rates for patients with Hypertensive ICH without and with IVH; В – indicators of 30-day survival depending on the mGS gradation |
5. Conclusions
- Thus, since patients with Hypertensive ICH, complicated by ICH have a significantly increased risk of death and unsatisfactory functional outcome, the evaluation of ICH gradation is important in predicting patient survival. The use of the mGS scale in patients with ICH allowed to differentiate the severity of the patient's condition and predict the 30-day survival and the 90-day functional outcome.The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML