-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(7): 739-742
doi:10.5923/j.ajmms.20221207.11
Received: Jun. 25, 2022; Accepted: Jul. 9, 2022; Published: Jul. 15, 2022

Biliary Peritonitis in Cholelithiasis: Observational Study
Arziyev Ismoil Aliyevich, Zafar Babajanovich Kurbaniyazov, Mannon Baxronovich Baratov
Department General Surgery, Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: Mannon Baxronovich Baratov, Department General Surgery, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

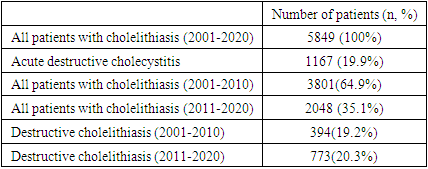
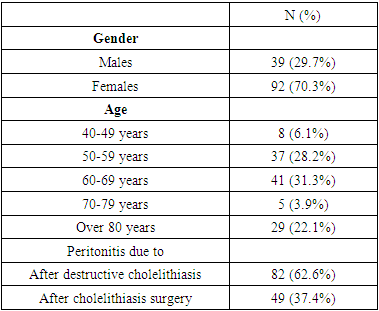
Over the last two decades, significant growth in the number of patients with cholelithiasis and its complications such as destructive cholecystitis and biliary peritonitis has been registered. This study aimed to study the causes of bile peritonitis in patients with cholelithiasis treated in 1st clinic of Samarkand State Medical University. We performed a clinic-based, observational study of patients with the diagnosis of acute destructive cholecystitis in the 1st Clinic of Samarkand State Medical University. All patients treated with the diagnosis between January 1, 2001, and January 1, 2020, were included in this study. Patient demographic characteristics such as age, sex and body mass index were taken from the registry of the hospital. In the surgical departments of the 1st clinic of Samarkand State Medical University, 5849 patients with cholelithiasis have been operated on during the last 20 years from 2001 to 2020. Of these, 1167 (19,9%) with acute destructive cholecystitis. We have observed a significant increase (1.9 times) in the number of operated patients with cholelithiasis in the period 2011-2020 (number of surgeries was 3801) compared to the decade preceded (table 1) (p<0.01). We studied 131 patients with bile peritonitis, which made up 2,2% of all operated patients with cholelithiasis. Among them 82 (7,1%) with peritonitis as a complication of acute destructive cholecystitis and 49 (0,8%) with peritonitis as a complication after cholelithiasis surgery. Among the patients with peritonitis, there were 39 (29.7%) male and 92 (70.3%) female patients with a gender ratio of 1:2.5. The same gender ratio among all operated patients with cholelithiasis was 1:6, which confirms the literature data about the complicated course of cholelithiasis in male individuals. Patients aged 60-69 years old - 41 (31,3%) and 50-59 years old - 37 (28,2%) prevailed. 11 (8.4%) patients were aged 70-79 years, 5 (3.9%) over 80 years, 29 (22.1%) 40-49 years and 8 (6.1%) 30-39 years. We have observed a significant increase in the number of surgeries on patients with cholelithiasis in the last 2 decades. However, the incidence of operated patients with peritonitis as the result of acute destructive cholecystitis and postoperative complications decreased significantly. The female gender has over two-fold higher risk of developing biliary peritonitis compared to males and older age was associated with more severe complications. Our results confirm the necessity of timely planned surgical intervention in patients with cholelithiasis using modern endo-video surgical techniques.
Keywords: Cholelithiasis, Complications, Peritonitis, Old age, Sex, Surgery, Observational study
Cite this paper: Arziyev Ismoil Aliyevich, Zafar Babajanovich Kurbaniyazov, Mannon Baxronovich Baratov, Biliary Peritonitis in Cholelithiasis: Observational Study, American Journal of Medicine and Medical Sciences, Vol. 12 No. 7, 2022, pp. 739-742. doi: 10.5923/j.ajmms.20221207.11.
Article Outline
1. Introduction
- Over the last two decades, significant growth in the number of patients with cholelithiasis and its complications as destructive cholecystitis and biliary peritonitis has been registered [3,5,11]. A peculiarity of biliary peritonitis is its hidden clinical manifestations, which lead to late diagnosis, increased frequency of postoperative complications and high mortality. Moreover, biliary peritonitis occurs more often in elderly and senile patients, which is caused by the prevalence of destructive forms of acute cholecystitis and sterile symptoms of the disease. Biliary peritonitis occurring in the postoperative period, as a complication of cholecystectomy, is also diagnosed late due to both clinical sterility and hesitancy of surgeons to perform repeated interventions [1,8,10]. This study aimed to study the causes of bile peritonitis in patients with cholelithiasis treated in 1st clinic of Samarkand State Medical University.
2. Materials and Methods
- We performed a clinic-based, observational study of patients with the diagnosis of acute destructive cholecystitis in the 1st Clinic of Samarkand State Medical University. All patients treated with the diagnosis between January 1, 2001, and January 1, 2020, were included in this study. All the data was extracted from the central patients' registry of the clinic. Personal data were anonymized and ethical approval from the Samarkand State Medical University review board was obtained. Patient demographic characteristics such as age, sex, and body mass index (BMI) were taken from the registry of the hospital. Data on clinical characteristics included concomitant diseases: diabetes mellitus, COPD, hypertension etc.; drug use: previous corticosteroid use, chemotherapy, anticoagulant use or coagulopathies. We used R studio 3.6.2 for all statistical analyses. We used Kolmogorov–Smirnov criteria to test the distribution of continuous variables. Mean values with corresponding standard deviations (SDs) were presented for continuous variables and absolute numbers with corresponding percentages were presented for categorical variables. We used the Mann-Whitney U test for continuous variables and the chi-square test for categorical data to compare risk factors. Fisher exact test was utilized in case of a small number of groups.
3. Results
- In the surgical departments of the 1st clinic of Samarkand State Medical University, a total of 5849 patients with cholelithiasis have been operated on during the last 20 years from 2001 to 2020. Of these, 1167 (19,9%) patients were operated on with acute destructive cholecystitis. We have observed a significant increase (1.9 times) in the number of operated patients with cholelithiasis in the period 2011-2020 (number of surgeries was 3801) compared to the decade preceded (table 1) (p<0.01). We also observed a significant increase (1.9 times) in the number of patients with cholelithiasis from 2011 to 2020 (number of operations was 3801), compared to the period from 2001 to 2010 (number of operations was 2048) (p<0.01).
|
|
4. Discussion
- The fundamental factors in the development of biliary peritonitis, according to academician F.G. Nazirov et al. (2019) include the nature, amount and rate of bile effusion [2]. The reactions of the peritoneum and the body differ in a massive one-step bile outpouring, a slow outpouring of its sweating. In the first case, abdominal shock will develop, but in the case of bile effusion, it is clinically unnoticeable (in our observations 3 of 27 patients with bile peritonitis were admitted to the clinic in a state of shock). The quality of the bile also influenced the development of the bile-induced pathological process. In gallbladder empyema, the perforation of the wall is not accompanied by shock (there were 10 such patients in our observations).The place of bile effusion is a free or separated abdominal cavity. Bile spreading throughout the abdominal cavity is accompanied by a severe shock reaction. If the bile is infiltrated and accumulates in a confined space, there is no clear pattern of peritonitis. The patient's condition, age, and the presence of concomitant pathology are of great importance in the outcome of the complications. In old age the disease in its initial stages is not clear, manifesting itself in the final stages when complications join and concomitant pathology is exacerbated. An analysis of 49 cases of bile peritonitis, occurred after surgical interventions for cholelithiasis, which made up 0.84% of the total number of patients (5849), operated on in the clinic from 2001 to 2020 years. We determined the following causes of peritonitis: - bile leak from Luschk's ducts in 17 patients after cholecystectomy; - undetected injury and cutting of common hepatic duct in 12 cases; - loss of clips and ligatures from bladder duct stump after cholecystectomy in 13 cases; - bile leak from choledochotomy in presence of cholelithiasis drainage and after drainage removal in 7 cases. Bile spreading all over the abdominal cavity was registered in 20 out of 49 patients with postoperative biliary peritonitis, in 29 patients the excessive bile was localized and retained only in the subhepatic space. The analysis of our observations testifies to the fact that there are certain difficulties in early diagnostics of postoperative bile peritonitis, caused by the course of peritonitis without clear clinical signs. According to our clinic over the last decade, there has been a significant (almost two-fold) increase in the number of patients with cholelithiasis and the number of operations. At the same time 19,9% of patients with cholelithiasis, i.e. nearly every 5th patient is operated on for acute destructive cholecystitis. Biliary peritonitis was observed in 82 (7.1%) out of 1167 patients with destructive cholecystitis, which coincides with the data of G.N. Gumerov et al. (2020) and E.E. Vrabie (2017). At the same time, only 37.8% of patients applied on the first day from the beginning of the disease [1,7]. Our researches and observations allow us to note, that biliary peritonitis, arises as a complication of acute destructive calculous cholecystitis and after operations for cholelithiasis. Also, it is difficult to diagnose in the early stages of bile leakage due to the erased clinical symptoms, which significantly aggravates the condition of patients by the time of manifestation of a clear clinical picture. These features of a clinical course of biliary peritonitis are pointed out in the publications of R. Hamura et al. (2016) and V.F. Zubritsky et al. (2017). J.F. Lock et al. (2016), and V.S. Budipranama (2020) and others noted a significant number of patients with proptotic biliary peritonitis when the clinic of abdominal catastrophe is rather late in presentation [8,9,10]. The incidence of biliary peritonitis after bile duct surgery according to V.F. Zubritsky et al. (2017), S.V. Chernokozinka (2021), and A.J. Staatz (2020) is most often associated with iatrogenic damage to the bile ducts and is 0.6-1.5% [3,9,11].
5. Conclusions
- We have observed a significant increase in the number of surgeries on patients with cholelithiasis in the last 2 decades. However, the incidence of operated patients with peritonitis as the result of acute destructive cholecystitis and postoperative complications decreased significantly. The female gender has over two-fold higher risk of developing biliary peritonitis compared to males and older age was associated with more severe complications. Our results confirm the necessity of timely planned surgical intervention in patients with cholelithiasis using modern endo-video surgical techniques.
ACKNOWLEDGEMENTS
- The authors express gratitude to Khasan Ibragimov for the help in manuscript preparation and translation into English.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML