-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(7): 729-732
doi:10.5923/j.ajmms.20221207.09
Received: Jun. 18, 2022; Accepted: Jul. 9, 2022; Published: Jul. 15, 2022

The Importance of Intracardiac Hemodynamics Indicators in Patients with Essential Hypertension and Rheumatoid Arthritis
Durbek Kasimov, Rustam Turakulov, Adigaffar Gadayev
Department of Internal Diseases #3, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim of the study. Comparative analysis of echocardiographic parameters of the heart in hypertensive patients with and without comorbid rheumatoid arthritis. Materials and methods. The study was conducted in 70 patients with arterial hypertension. Patients were divided into 2 groups based on the presence of rheumatoid arthritis: the main group (n=40) included patients with arterial hypertension and rheumatoid arthritis, the control group (n=30) - patients with arterial hypertension without comorbid rheumatoid arthritis. Echocardiographic investigation was performed in all patients following recommendations of the American echocardiography association. Results. In patients of the main group, left ventricular hypertrophy and diastolic dysfunction were manifested stronger compared to the control group. Statistically significant positive correlation was found between left ventricular hypertrophy and diastolic dysfunction on one hand and rheumatoid arthritis related factors.
Keywords: Essential hypertension, Rheumatoid arthritis, Echocardiography, Left ventricular mass index, Diastolic dysfunction
Cite this paper: Durbek Kasimov, Rustam Turakulov, Adigaffar Gadayev, The Importance of Intracardiac Hemodynamics Indicators in Patients with Essential Hypertension and Rheumatoid Arthritis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 7, 2022, pp. 729-732. doi: 10.5923/j.ajmms.20221207.09.
1. Introduction
- Essential hypertension remains one of the leading causes of morbidity and mortality throughout the world. It significantly affects incidence and course of serious cardiovascular complications such as stroke, coronary artery disease, heart failure, aneurism of abdominal aorta and peripheral artery diseases.Estimated number of essential hypertension cases in adults around the world reaches 1.28 billion and two thirds of it is in developing countries. Nearly half of patients with essential hypertension (46%) are unaware of their problems. Even after diagnosis, satisfactory control of arterial blood pressure is achieved only in 30-40 percent of cases [1].Essential hypertension is frequently accompanied by at least one comorbid condition. Number of studies show the presence of one comorbid disease in 80 percent of patients with essential hypertension, while in 55 percent of cases there were two or more such diseases. In such circumstances risk of cardiovascular complications will not be an arithmetical sum of two risk factors but will increase exponentially [2]. One of the conditions that aggravate the course of cardiovascular diseases, including essential hypertension, is rheumatoid arthritis (RA). Around 1 percent of the world population suffers with this autoimmune disease. According to number of studies, prevalence of essential hypertension among RA patients varies between 30 and 80 percent [3]. Moreover, in 25-35 percent of patients with essential hypertension and RA blood pressure control is unsatisfactory. The number is 1,5 to 2 times higher compared to that of the patients with high blood pressure but without comorbid RA [4].The information mentioned above confirms, that development of clinical recommendations on timely diagnosis and treatment of arterial hypertension in patients with comorbid diseases, including RA remains one of the pressing issues of today’s medicine.Heart involvement is often asymptomatic or causes mild ailments, frequently disregarded by affected persons, because RA individuals are generally not energetic and avoid to move too much. Since RA patients are often hypodynamic, clinical symptoms of heart diseases related with physical activity manifest themselves rather late. These are perhaps the reasons why at least twice as many changes in RA hearts are recognized post-mortem then during the patients’ lifetime. One of the current issues in medicine therefore is to recognize the presence, type and the extend of heart involvement in RA and to search for correlations of their intensity with clinical activity of the disease. Echocardiography appears to be of much help in this aspect.For above mentioned reasons, it is interesting to study echocardiographic changes in patients with essential hypertension with comorbid RA.The aim of the study. To study and comparatively analyse indices of intracardiac hemodynamics in patients with essential hypertension and rheumatoid arthritis.
2. Materials and Methods
- The study was conducted in multi-profile clinic of Tashkent medical academy. 70 patients with essential hypertension during 2019-2021 were selected. They were divided into two groups. The main group consisted of 40 patients (21 women (52.5%) and 19 men (47.5%); mean age 48,2±1.48 years) with essential hypertension and RA with intermediate disease activity and receiving disease modifying agents. The control group consisted of 30 patients (14 women (46.7%) and 16 men (53.3%); mean age 49.6±1.27 years) with essential hypertension but without RA. The diagnosis of essential hypertension was made based on patients complaints, history, physical examination, laboratory and instrumental investigations, according to ESC/ESH 2018 recommendations [5]. The diagnosis of RA was formulated based on ACR/EULAR 2010 diagnostic recommendations [6]. Patients with other systemic inflammatory disorders, severe internal organ diseases, acute inflammatory process, oncologic and psychiatric diseases and other serious diseases were excluded from the study.Echocardiography (EchoCG) investigation was performed with transthoracic method using Toshiba SSH-YO(60)A device (3,5 Mhzs, Japan). In order to evaluate functional status of the heart M and B modalities from different approaches were used in accordance with the recommendations of the American echocardiography association. During the evaluation following indices were measured: end diastolic and systolic diameters and volumes of the left ventricle (LV), left ventricular posterior wall thickness and intraventricular septum thickness, left ventricular ejection fraction (LVEF), systolic volume. As it is well known, LVEF, systolic volume, diameters and volumes of the heart chambers largely depend on patients’ height, weight and sex. Therefore, these indices are standardized by dividing them to body surface area. Left ventricular mass index (LVMI)was calculated using formula suggested by Devereux R.B.LVMI values greater than ≥134 g/m2 in men and ≥110 g/m2 in women was considered as a LV hypertrophy. Remodelling of LV myocardium was evaluated based on it’s relative wall thickness (LVRWT). LVRWT values form 0.31 to 0.45 were considered as adapted remodelling and values ≤0.30 as non-adapted. Diastolic dysfunction of LV was estimated by Doppler echocardiographic analysis of transmitral flow (TMF). Type of diastolic dysfunction was differentiated by dividing early diastolic filling velocity of LV (E peak) to late diastolic filling velocity (A peak), e.g. E/A. There are three types of LV diastolic dysfunction: Type I – impaired relaxation of LV (E/A≤1), Type II – pseudonormal (E/A=1-2) and Type III – restrictive (E/A>2). Erythrocytes sedimentation rate (ESR) was measured using Panchenko’s apparatus in 100 mm tube by diluting blood with 5 percent solution of sodium citrate.Activity level of RA was evaluated using DAS28 integral index.S-reactive protein (SRP) levels were measured by electro-chemiluminescence analyses and by using Humatex CRP reactives (Human Gmbh., Germaniya).For data processing IBM SPSS Statistics 21.0 computer program was used. Arithmetic mean and standard deviation (M±m) of all data in following tables were calculated. To determine significance of difference between groups Student’s paired and unpaired t-tests for quantitative indices and Chi2 criterion for qualitative indices were used. Correlation analysis was done using Pearson’s correlation coefficient and confidence tables. Differences were considered to be statistically significant when р<0.05.
3. Results
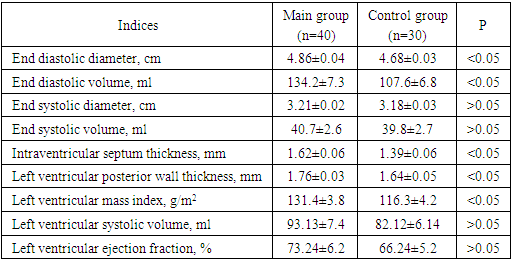
- Following central hemodynamic values were found in patients involved in our study:
|
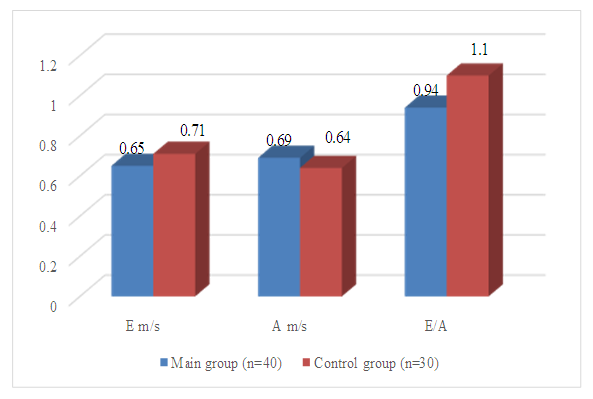 | Figure 1. Parameters of diastolic dysfunction of the patients in the study |
4. Discussion
- Involvement of heart in RA was detected in numerous studies. Kłodziński Ł et. al found left ventricular mass in RA individuals significantly greater then in the controls. The same concerned intraventricular septum end diastolic thickness, LV posterior wall end diastolic thickness. The ejection fraction was significantly lower in RA patients compared to the controls These findings are in accordance with Alpaslan, Di Franco and Levendoglu’s results, that revealed significant differences in LV diastolic function (peak E velocity, E velocity/A velocity ratio, IVRT, myocardial performance index (MPI) and transmural flow propagation velocity (TFPV)) between RA group and the control subjects [7].The results of these studies indicate to the presence of subclinical myocardial involvement in RA, which can be ascribed to nonspecific myocarditis observed in this disease. Nevertheless different other risk factors for cardiac muscle impairment are usually present in RA individuals and therefore it is uncertain, whether heart pathology in rheumatoid arthritis is due to inflammation itself or is secondary to other process or to drug use in this disease.Studies devoted to the assessment of diastolic function parameters revealed significantly longer isovolumetric relaxation time and deceleration time in RA patients.The authors noticed that RA patients, in absence of overt heart disease, show diastolic function characterized by impaired E/A and S/D ratio. They explain increased risk of cardiovascular diseases in RA patients partly by this phenomenon. Yazici et al. aimed at determining diastolic abnormalities in RA at baseline and after a 5-year follow-up, considering that cardiovascular findings are mostly subtle and diastolic function abnormalities are one of the earliest manifestations. The author concluded that RA is associated with increased risk of cardiovascular mortality [8]. In RA patients LV filling abnormalities were characterized by a reduced E/A ratio (0.98±0.22]) compared to the controls (1.09±0.11; p=0.004). Moreover, strong negative correlation between E/A ratio and the disease duration was found (r=-0.56, p= 0.001) [8]. In our study E/A ratio was also lower in patients of the main group compared to the control group (0,94±0,03 against 1,1±0,04; p<0.05).Saadati N., as well as Krasnoselski et. al studied relationship between echocardiographic changes in the heart and RA related factors (RA duration, SRO, ESR etc.). The studies found weak to moderate positive correlation between LVMI, diastolic dysfunction on one hand and RA duration, SRP and ESR levels on another (r=0,29-0,46; p<0.05) [9]. In our study, there was negative correlation between E/A ratio on one hand and SRP, ESR, RA duration and DAS28 score on another (r=-0,21, r=-0,11, r=-0,17 and r=-0,19 respectively; p<0.05). Correlation between LVMI and ESR was weak positive (r=0,27; p<0.05), while correlations between the former and with SRP, RA duration and DAS28 score were positive (respectively r=0,48, r=0,42 and r=0,43; p<0.05).The above mentioned confirms the negative effect of inflammation on myocardial function. Many of these changes do not include dilation and systolic dysfunction of the heart chambers and therefore often ignored as asymptomatic by doctors and researchers. However, pathologic changes which occur in RA patients, particularly diastolic dysfunction and LVMI, negatively affect life quality and expectancy of patient. Echocardiography enables us to detect and monitor them and should be viewed as a standard investigative method in all patients with RA.
5. Conclusions
- In arterial hypertension, the dominant type of left ventricular remodelling is concentric hypertrophy – 85%. In rheumatoid arthritis, all types of remodelling are equally present: eccentric hypertrophy – 22.3%, concentric hypertrophy – 27.2%, concentric remodelling – 36.9%. When hypertension is accompanied by rheumatoid arthritis, pathological types of remodelling occur in 96.4% of cases: eccentric hypertrophy – 13.4%, concentric hypertrophy – 78.6%, concentric remodelling – 4.4%. Furthermore, eccentric hypertrophy is associated to a greater extent with rheumatoid arthritis, and concentric hypertrophy with hypertension. In case of combination of arthritis with high blood pressure, diastolic dysfunction of left ventricle was detected in 70% of cases. Both myocardial mass index and diastolic dysfunction of left ventricle had positive correlation with activity and duration of rheumatoid arthritis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML