Ibatova Sh. M., Mamatkulova F. Kh., Mamatkulova D. Kh., Ruzikulov N. Yo., Abdurasulov F. P.
Samarkand State Medical University, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Giardiasis is one of the most common helminthic infestations in the world. Giardiasis manifests itself both in a latent form and in the form of intestinal disorders. The aim of the study was to study the clinical features of giardiasis in children. Under supervision there were 78 children with latent form of giardiasis aged from 3 to 15 years. All patients underwent a comprehensive clinical examination, which included the collection of anamnesis, physical examination, complete blood count, feces. The classic method of laboratory diagnosis of giardiasis are protozoological studies. Giardiasis in children occurs in a latent, subclinical and clinical form. In the clinical form of giardiasis, the manifestations of duodenitis were most pronounced, which must be taken into account when individualizing the diet and treatment in children.
Keywords:
Giardiasis, Patients, Clinical forms, Diagnostics
Cite this paper: Ibatova Sh. M., Mamatkulova F. Kh., Mamatkulova D. Kh., Ruzikulov N. Yo., Abdurasulov F. P., Study of the Clinical Features of Giambliasis in Children, American Journal of Medicine and Medical Sciences, Vol. 12 No. 7, 2022, pp. 711-714. doi: 10.5923/j.ajmms.20221207.05.
1. Relevance
Giardiasis is one of the most common helminthic infestations in the world. The problem of giardiasis is also very relevant for the Republic of Uzbekistan. In Uzbekistan, among parasitic diseases, giardiasis makes up a large proportion (60-70%) among children in organized children's groups [1,3,5]. It is known that giardiasis manifests itself both in a latent form and in the form of intestinal disorders [13,15,16]. The previously described giardia lesions of the hepatobiliary system are subject to revision, since giardia are located on the surface of the mucous membrane of the duodenum, small intestine and are not found in the biliary tract [2,6,9]. However, it has been proven that with massive giardiasis invasion, enteral syndrome of varying severity occurs, manifested by abdominal pain, unstable stools with polyfecal matter. In children, especially at an early age, the increase in body weight slows down, a deficiency of vitamins and minerals develops [7,10,14].Along with severe clinical manifestations of giardiasis, latent forms of the disease are also described [8,12]. Isolation of Giardia without clinical manifestations is often used as an argument for evaluating this condition as a healthy carriage of protozoa. However, with the accumulation of data on morphological changes in the microvilli of intestinal epithelial cells during invasion, as well as immunological changes in the body with giardiasis, the possibility of their pathogenic effect even with asymptomatic carriage becomes obvious. Studies conducted in Giardia carriers revealed both functional and morphological changes.
2. Purpose of the Study
To study the clinical features of giardiasis in children.
3. Material and Research Methods
78 children with a latent form of giardiasis aged from 3 to 15 years were under observation. All patients underwent a comprehensive clinical examination, which included the collection of anamnesis, physical examination, complete blood count, feces. Particular attention was paid to determining the process of fat resorption, which was assessed by the results of an extended scatological study. The classic method of laboratory diagnosis of giardiasis are protozoological studies. Microscopic examination of native and stained with Lugol's solution smears from freshly isolated feces is carried out.
4. Research Results
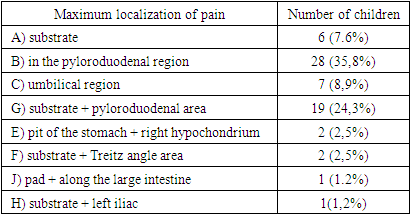
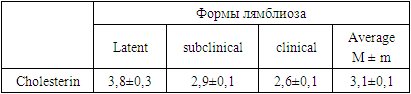
In the subclinical form of giardiasis, which included children aged 3 to 15 years, mild abdominal pain was often observed in 66 out of 78 (84.6%), "intestinal" dyspepsia syndrome in 52 (66.7%) and less frequently. "gastric" dyspepsia in 26 (33.3%) patients. Such symptoms are generally typical for giardiasis and are explained by the fact that protozoa vegetate in the duodenum and small intestine, which leads to the development of duodenitis and enteritis.In the children we observed, the pains were late, occurred on an empty stomach or appeared 1-2 hours after eating. Pains, as a rule, were pulling and dull. Only 3 children out of 78 (3.8%) had the Moinigan rhythm of pain (pain - food - relief).This is also evidenced by the peculiarities of the localization of pain in the abdomen during palpation (Table 1).Table 1. Maximum localization of abdominal pain in children with subclinical form of giardiasis
 |
| |
|
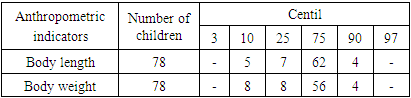
As can be seen from Table. 1. in the subclinical form of giardiasis, abdominal pain on palpation was mainly localized in the pyloroduodenal and pit + pyloroduodenal zones (24.3%), which is characteristic of duodenitis. Less commonly, pain was noted near the navel (8.9%) and in the pit of the stomach in 6 children.Along with a mildly pronounced pain syndrome, the children observed by us with a subclinical form had dyspeptic phenomena. The most frequently observed nausea in 11 children out of 78 (14.1%), which is characteristic of increased pressure in the duodenum with a simultaneous decrease in the pressure gradient between the stomach and duodenum. Belching was observed in 8 patients (10.2%), in the genesis of which a certain importance is attached to an increase in pressure in the stomach cavity due to | strengthening its tone or spasm of the pylorus. And only 2 patients had vomiting and heartburn.Based on the severity of clinical manifestations, latent, subclinical and clinical forms of giardiasis were identified. Among the various forms of giardia invasion, its asymptomatic form occupies a special place. The actual isolation of Giardia without clinical manifestations is often used as an argument for evaluating this condition as a healthy carriage of protozoa. However, with the accumulation of data on the morphology of Giardia, the epidemiology of this invasion, on morphological and functional changes in the gastrointestinal tract, as well as immunological changes in the body with giardiasis, the possibility of a certain effect of Giardia on the human body becomes obvious even with their asymptomatic carriage [4,11]. Endoscopic and morphological studies conducted during long-term giardia carriers in adults revealed focal or widespread hyperemia, edema of the duodenal mucosa [17].Along with signs of the so-called "gastric" dyspepsia, symptoms of "intestinal" dyspepsia were observed twice as often.In 38 of 78 patients (48.7%), unstable stools were observed. These children often had loose stools, the feces were homogeneous, light yellow in color without pathological impurities.Only 6 (7.6%) patients were diagnosed with flatulence, 6 (7.6%) had constipation, in 3 patients (3.8%) the lower edge of the liver protruded along the anterior axillary and midclavicular lines by 4 cm and on palpation was slightly painful. These children suffered from viral hepatitis a year ago.The physical development of children with subclinical form of giardiasis was assessed by centile tables.Table 2. Body length and weight in children with subclinical form of giardiasis
 |
| |
|
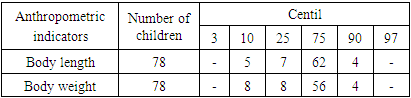
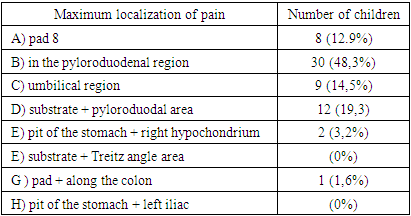
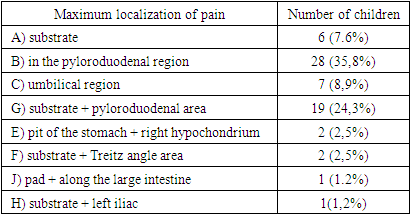
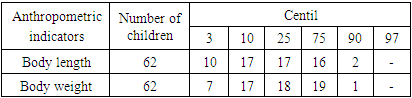
As can be seen from Table. 2, in children with a subclinical form of giardiasis, growth was more often than average in 69 of 78 (88.5%), and in 5 (6.4%) below average and only in 4 (5.1%) above average.Body weight in children with subclinical form of giardiasis was often average in 64 out of 78 (82.0%), and below average in 8 out of 78 (10.2%), above average in 4 out of 78 (5.1%) children.The skeletal system, respiratory organs, cardiovascular system in patients with subclinical form of giardiasis were not changed.Two children complained of headaches, 4 patients complained of irritability. Cyst secretion in the subclinical form ranged from 0.7 to 2.2, averaging 1.5 cysts per field of view.Under our supervision there were 62 patients with a clinically pronounced form of giardiasis aged 3 to 15 years. Compared with the subclinical form, patients in this group experienced more intense abdominal pain, manifestations of "gastric" and "intestinal" dyspepsia. In addition, some patients had relatively low body weight and growth retardation, which was indicative of malabsorption of nutrients.Of interest was the maximum localization of pain during abdominal palpation (Table 3).Table 3. Maximum localization of pain during palpation of the abdomen in children with the clinical form of giardiasis
 |
| |
|
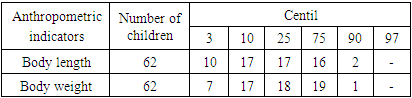
As can be seen from Table. 3. most often, the maximum localization of pain during palpation of the abdomen in children with the clinical form of giardiasis was localized in the pyloroduodenal and substratum + pyloroduodenal area in 42 out of 62 children (67.7%), which is also characteristic of duodenal lesions. Patients with the clinical form of giardiasis had late pain that appeared on an empty stomach or 1-2 hours after eating. Although the pains were dull, they were more prolonged than in the subclinical form.Moinigan's rhythm of pain was noted only in 5 of 62 (8%) patients. Significantly more often than in the subclinical form, manifestations of "gastric" dyspepsia were observed. So, nausea was in 18 out of 62 (29.0%) children, belching in 11 (17.7%), heartburn in 6 (9.6%). In 26 children there was a decrease in appetite.Enteral syndrome was more pronounced. Fifty-five of 62 (88.7%) children had loose stools, 6 (9.6%) had flatulence, and 3 (4.8%) had borborygmi. In 28 out of 55 (50.9%) children with a clinically pronounced form of giardiasis, the stool was liquid, homogeneous, often frothy, yellow. Scatological examination revealed leukocytes, epithelial cells, and fatty acid crystals in the feces. In 17 out of 62 (27.4%), the stool is liquid with an increase in muscle fibers, connective tissue, and plant fiber (duodenal syndrome).In 28 out of 62 (12.9%) patients, the stools were liquid, abundant, yellow-gray in color, ointment-like. The study determined neutral fats, starch grains, muscle fibers, which is typical for pancreatic insufficiency. Only 2 out of 62 (3.2%) had mucus in their stools.In 13 out of 62 (20.9%) children with the clinical form of giardiasis, liver enlargement was detected. From the anamnesis it is known that these children had previously had viral hepatitis.In the clinical form of giardiasis, the physical development of children suffered more (Table 4).Table 4. Body length and weight in children with clinical form of giardiasis
 |
| |
|
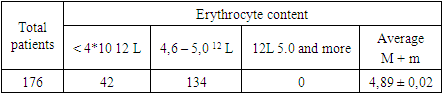
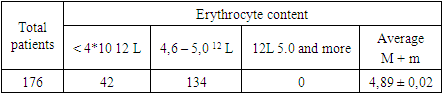
As can be seen from Table. 4, in children with the clinical form of giardiasis, growth was average only in 33 of 62 (53.2%), below average in 17 (274%), and in 10 (16.1%) growth was low.A similar picture applies to body weight. The average body weight was in 37 out of 62 children (59.7%), below the average in 17 (27.4%), and in 7 low (11.2%). Naturally, in the clinical form of giardiasis, 24 out of 62 (38.7%) more often had disharmonious development (the difference in corridors was 2 intervals).Pallor of the skin was noted in 41 of 62 (66.1%), and in 2 patients (3.2%) on the trunk, chest, abdomen, a large-spotted allergic rash (such as urticaria) was noted.In 3 out of 62 (4.8%) children, a gentle systolic murmur was heard at the apex of the heart of a functional nature. The limits of relative dullness of the heart were within the age norm.In addition, patients often complained of weakness (17.7%), irritability (29%), less often of sleep disturbances and headache.With a clinically pronounced form of giardiasis, cystic excretion ranged from 2.2 to 2.8, averaging 2.5 cysts per field of view.All 176 children with giardiasis underwent general clinical and biochemical analyzes (Table 5).Table 5. The average content of erythrocytes in children with giardiasis
 |
| |
|
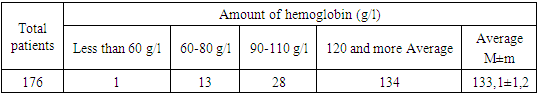
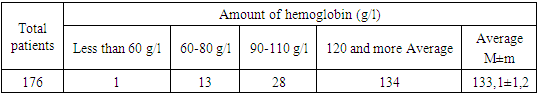
As can be seen from Table. 5, the average content of erythrocytes in giardiasis was within the normal range, but in 42 children out of 176 (23.8%) | anemia was noted. This is also confirmed by the results of the study of hemoglobin (Table 6).Table 6. Hemoglobin content in children with giardiasis
 |
| |
|
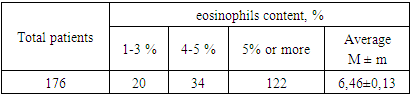
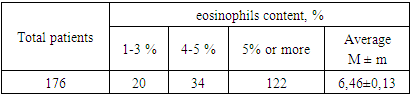
As can be seen from Table. 6, 42 of 176 (23.9%) children with giardiasis had anemia, and 28 of 176 (15.9%) had mild anemia, 13 (7.3%) had moderate anemia, and only one had severe anemia. In the latent form of giardiasis, anemia was not observed, in subclinical form in 1 out of 78 (1.3%), in clinical in 41 out of 62 (66.1%) children.The number of leukocytes in observed children with giardiasis ranged from 5.2 to 9.3 * 109 liters and averaged 7.2 + 0.1-109 liters.In children with latent form it was 6.2±0.2, in subclinical form 17.6±0.2, clinical 8.0±0.3*109l.4.5% of children with giardiasis had neutrophilia, 1.7% had neutropenia, and 1.1% had lymphocytosis.It is known that invasion by protozoa and worms is often accompanied by eosinophilia (Table 7).Table 7. The content of eosinophils in children with giardiasis
 |
| |
|
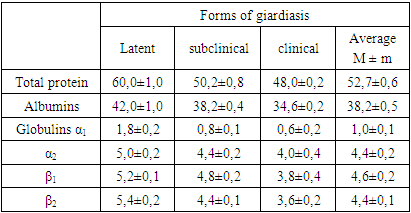
As can be seen from Table. 7, an increase in eosinophils was noted in the absolute number of patients.Since enteral syndrome, lag in weight and growth were often observed in patients with giardiasis, the results of a study of protein and their fractions are of interest (Table 8).Table 8. The average content of protein and its fractions (in g/l) in the blood serum of children with giardiasis
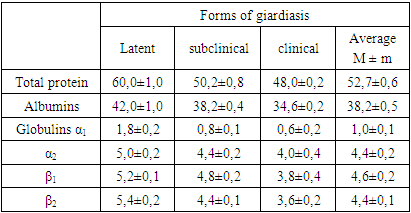 |
| |
|
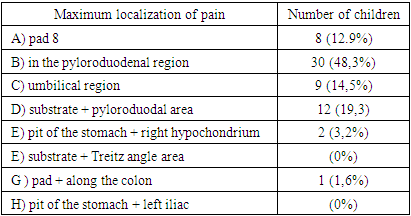
As can be seen from Table. 8, hypoproteinemia is most pronounced in the clinical form of giardiasis.Invasion by protozoa is often accompanied by steatorrhea, therefore, the results of a study of serum cholesterol were of interest (Table 9).Table 9. The content of cholesterol (in mmol / l) in the blood serum of children with giardiasis
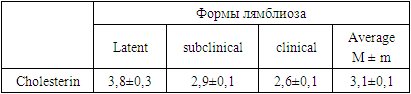 |
| |
|
As can be seen from Table. 9. there is a direct dependence of the degree of hypocholesterolemia on the clinical form of giardiasis.Сonclusion Thus, giardiasis in children occurs in a latent, subclinical and clinical form. In the latent form, no clinical manifestations were observed.In the subclinical form, an unsharply pronounced clinical picture of duodenitis was revealed. Clinical manifestations of duodenitis are most pronounced in the clinical form of giardiasis. A certain dependence of the degree of anemia, eosinophilia, hypoproteinemin, hypocholesterolemia on the clinical form of giardiasis was noted. This must be taken into account when individualizing the appointment of a diet and treatment in children.
References
| [1] | Agarkova L.D., O.M. Sokolovskaya, E.N. Maslodudova, I.N. Melnichenko. Infection with giardiasis in the population of the Kyiv region of Donetsk // Problems of ecology in the field of environmental protection of the technogenic region. Donetsk: DonNU, Volume 7. 2010 - P. 77–84. |
| [2] | Akhmetova R.A. Diagnosis, treatment and prevention of giardia infestation in children with chronic diseases of the digestive system. // Guidelines. Ufa. 2018. S.-5-14. |
| [3] | Babak O.Ya. Intestinal helminthiases: the situation and the trend towards its change // Health of Ukraine. -2016. -No. 9(1). pp. 89-110. |
| [4] | Bodnya E.I. Giardiasis in children: clinical manifestations, treatment tactics // Health of the child. - 2011. - No. 8(35), pp. 91–94. |
| [5] | Grigorieva I.N. Modern ideas about the pathogenesis, optimal therapy and prevention of giardiasis. // Medical consultation. 2010. T.12.-S. 59-62. |
| [6] | Denisov M.Yu. Modern aspects of treatment, rehabilitation and prevention of giardia infestation in children. // Bulletin of NSU Series: Biology, Clinical Medicine. 2018. V.6. S. 97-101. |
| [7] | Dudnik V.M. Diagnosis and pathogenetic aspects of helminthiases in children // Modern Pediatrics. 2011. No. 4(38). pp. 70-72. |
| [8] | Ershova I.B. Parasitic invasions in the practice of a pediatrician // Health of the child. 2017. - No. 2(5). - S. 137-140. |
| [9] | E.A. Giardiasis: Textbook for doctors. - St. Petersburg: InformMed, 2010, pp. 32–33. |
| [10] | Inoyatova F.I., Nurmatova N.F. The state of the intestinal microflora in children with chronic hepatitis B and giardiasis Republican Specialized Scientific and Practical Medical Center for Pediatrics, Ministry of Health of the Republic of Uzbekistan, Uzbekistan, Tashkent, // children's infections 2015. P.55-65. |
| [11] | Kramarev S.A. Giardiasis (clinical lecture) // Modern. Pediatrics. 2015. - No. 4. S. 161-164. |
| [12] | Krivopustov S.P. Helminthiases in clinical pediatrics: issues of diagnosis, therapy, prevention // Health of the child. - 2011. - No. 4 (31). - S. 71-75. |
| [13] | Ramazanova A.B., Ibatova Sh.M., Abdukadirova N.B. Variants of clinical manifestations of giardiasis in children. International scientific journal "Problems of Biology and Medicine". Samarkand, 2021, No. 1.1 (126), -p. 342-344. |
| [14] | Usenko D.V. Modern aspects of diagnosis and treatment of giardiasis // Questions of modern pediatrics. - M., 2015. T.14. pp.108-113. |
| [15] | Ibatova Sh.M., Abdurasulov FP, Ruzikulov NY. Features of clinical manifestations of lambliosis in children. International Journal of Research and Development. Volume: 7. Issue: 1. January 2022 P. 38-41. |
| [16] | Ibatova Sh.M., Mukhamadiev N.Q., Abdurasulov F.P. Clinical manifestations of giambliasis in children. Central Asian Journal of Medical and Natural Sciences. Volume: 03 Issue: 02. Mar-Apr 2022. P. 306-308. |
| [17] | Litleskare, S., Wensaas, K.–A., Eide, G., Hanevik, K., Kahrs, G., Langeland, N., Rortveit, G. Perceived food intolerance and irritable bowel syndrome in a population 3 years after a giardiasis– outbreak: a historical cohort study, BMC Gastroenterology, 2015, Vol. 15, pp. 164. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML