-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(6): 647-652
doi:10.5923/j.ajmms.20221206.08
Received: May 15, 2022; Accepted: Jun. 1, 2022; Published: Jun. 13, 2022

Clinical Efficiency of Hemoben Wound Coating for Liver and Spleen Injuries
Sadykov R. A., Ismailov S. I., Babadjanov A. Kh., Orazaliev G. B., Sultanov S. A., Bazarbayev A. G.
Republican Specialized Scientific and Practical Medical Center for Surgery Named After Acad. V. Vakhidov, Beruni District Medical Association, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

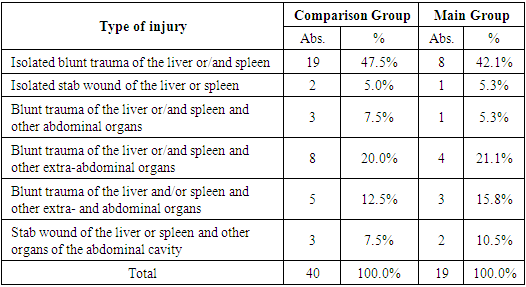
Aim of the study wasto determine the hemostatic efficacy of the drug “HEMOBEN” in patients with parenchymal organ injuries. Background. The small intestine, liver and spleen are most often injured at combined trauma of the abdominal organs. The liver is second only to the intestine in terms of the frequency of injuries. The study included only patients who were admitted with liver or spleen injury on the background of blunt trauma or stab wound, in whom combined injuries of other organs and systems did not threaten their lives (without fatal outcomes on the background of critical condition). Material and methods. The patients were divided into two groups: Main Group (n=19) where Hemoben was used for hemostasis; Comparison Group (n=40) where mechanical and physical methods of hemostasis had been used. The cause of parenchymal organs injury (liver and/or spleen) both in isolation and in combination with other organs and tissues in 67.5% of the Comparison Group and in 63.2% of the Main Group were blunt trauma, while stab wounds made up only from 7.5% to 10.5%. Results. Comparative analysis showed that hemostasis with the use of Hemoben was significantly more effective (χ2=1,052; (df=1); p=0,306, р<0.05) than the use of suturing and /or coagulation of the wound. A similar trend can be traced with the spleen injury: the proportion of splenectomy using Hemoben was significantly lower (36.4%), and hemostasis was higher and made up 63.6%, which was statistically significant (χ2=4.082; (df=1); p=0.044, р<0.05). Discussion. A feature of the HEMOBEN composition is the presence of easily decomposable calcium ions in it, which further accelerates the stopping of bleeding in the affected area upon contact with blood. According to our data, a new domestic wound coating made of cellulose derivatives with prolonged action has a good hemostatic effect when modeling parenchymal bleeding from a spleen wound, providing the formation of a film with tight adhesion to the wound surface. Conclusion. If we consider isolated liver injury, the efficiency of hemostasis did not significantly differ both in the main and in the comparison groups.
Keywords: Hemostasis, Liver, Spleen, Combined injury
Cite this paper: Sadykov R. A., Ismailov S. I., Babadjanov A. Kh., Orazaliev G. B., Sultanov S. A., Bazarbayev A. G., Clinical Efficiency of Hemoben Wound Coating for Liver and Spleen Injuries, American Journal of Medicine and Medical Sciences, Vol. 12 No. 6, 2022, pp. 647-652. doi: 10.5923/j.ajmms.20221206.08.
1. Introduction
- The small intestine, liver and spleen are most often injured at combined trauma of the abdominal organs. The liver is second only to the intestine in terms of the frequency of injuries [1]. Liver injuries due to special diagnostic difficulties, the severity of the course and the high frequency of complications are the most dangerous among the abdominal cavity closed injuries [2]. Postoperative mortality in liver injury remains high and reaches 12-34%, and various intra-abdominal complications are noted in 17-35% of patients [1,3-5]. The spleen is also often injured in case of a closed injury of the abdomen, and its traumatic defects are more bleeding. The main cause of an unfavorable outcome of liver and spleen injuries is intra-abdominal bleeding, so the timeliness of surgical intervention and the choice of an adequate method of hemostasis are of particular importance. Tactical and technical errors during the surgery expressed in an unjustified expansion of the intervention volume, lead to an increase of mortality [6-8]. Currently, the main method of treating liver wounds is suturing, which is used according to various authors in 60-80% of surgeries. Its hemostatic effect is due to the fact that the tied thread cuts through the liver parenchyma and vascular formations gather in a bundle. However, suturing the liver has a number of disadvantages: 1) the formation of a necrosis band distal to the suture, respectively, the possibility of abscessing in this area; 2) the likelihood of bleeding with insufficient tightening of the sutures; 3) technical difficulties and the duration of the application; 4) the threat of secondary bleeding [2,3,5,8].Another commonly used method of hemostasis is electrocoagulation. After its use, a scab is formed with a necrosis zone of 3-5 mm, which serves as a substrate for the development of infectious complications, secondary bleeding [4,6,9]. At the same time, alternative methods of hemostasis are being searched for in case of bleeding from parenchymal organs. Thus, studies were conducted at the Belarusian State Medical University on the use of inorganic salts to stop bleeding from the liver.
2. Material and Methods
- The study included only patients who were admitted with liver or spleen injury on the background of blunt trauma or stab wound, in whom combined injuries of other organs and systems did not threaten their lives (without fatal outcomes on the background of critical condition). Only cases with intraoperative attempt of local hemostasis among patients with spleen damage (that is, splenectomy was not initially used) were analyzed to form comparable study groups. All this allowed to objectively evaluate the hemostatic efficiency of the proposed method.Aim of the study was to determine the hemostatic efficacy of the drug “HEMOBEN” in patients with parenchymal organ injuries.
3. Results
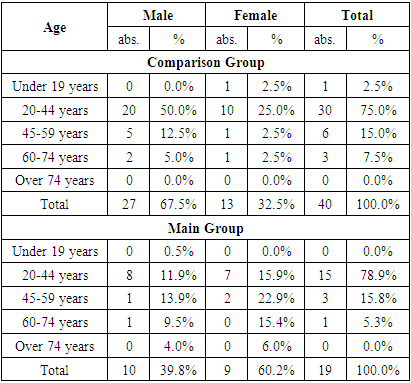
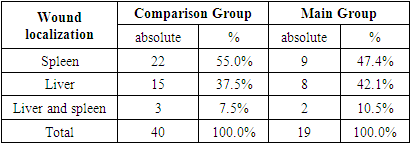
- The predominance of the female sex (67.5%) was noted in the comparison group, while the main one was dominated by males (60.2%). The mean age was 37.3±13.1 years in the comparison group and 35.0±12.8 years in the main group and in both groups ranged from 20-44 years in 78.9% of patients (Tab. 1).
|
|
|
|
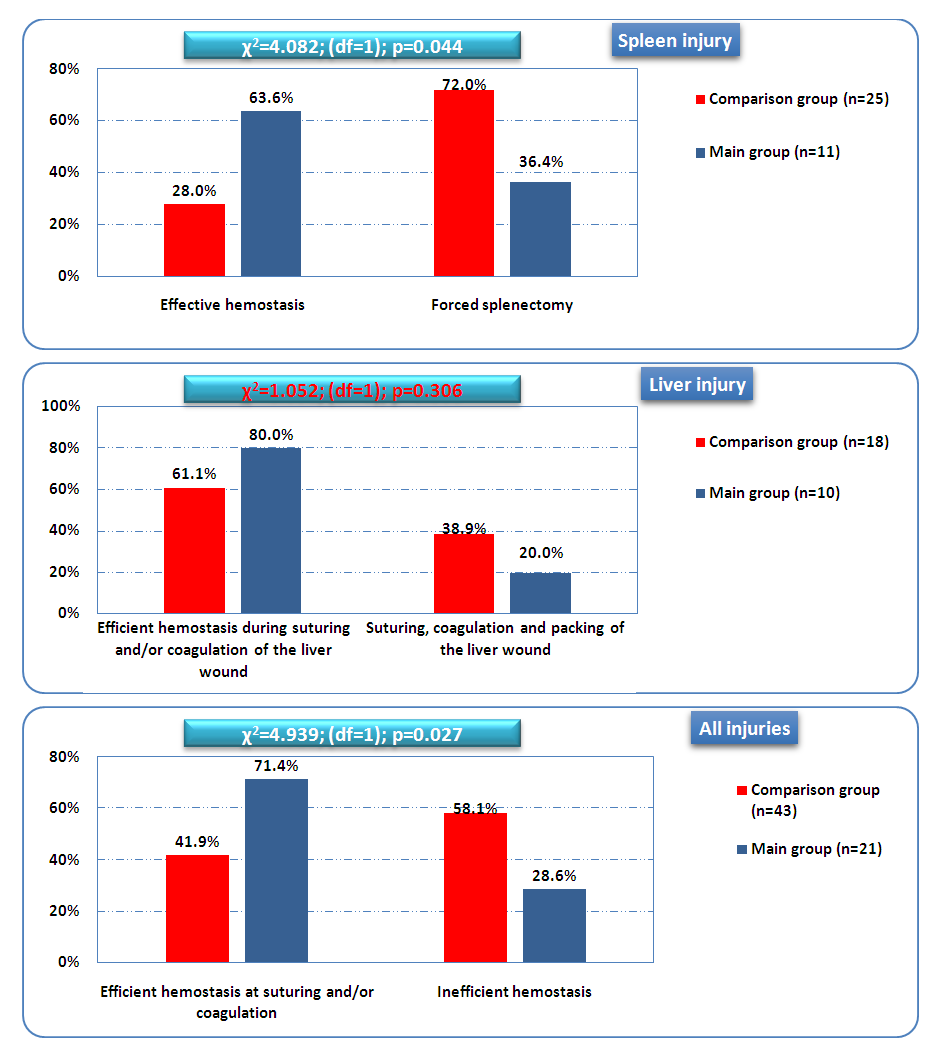 | Figure 1. The efficiency of local hemostasis attempts at injury of the liver parenchyma and (or) spleen |
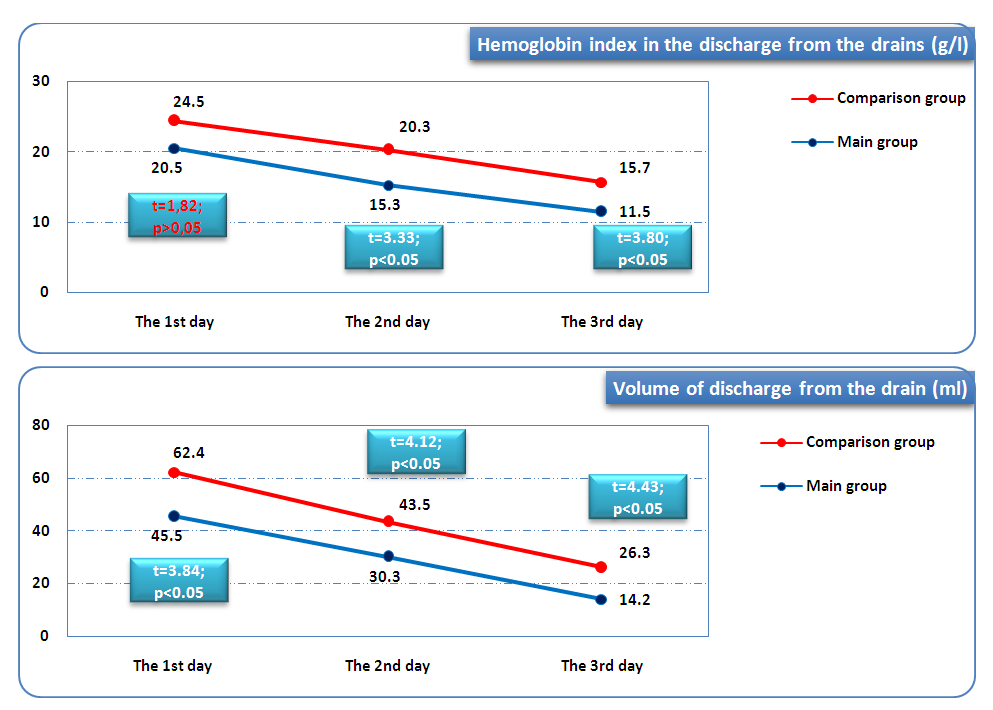 | Figure 2. The volume and index of hemoglobin in the discharge from the drains |
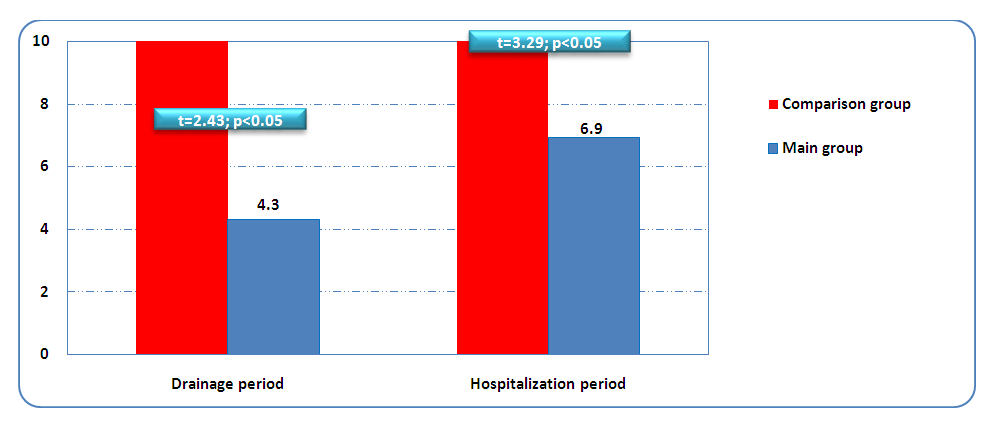 | Figure 3. Average drainage period and duration of the hospital stay (days) |
4. Discussion
- From the biomechanism of blood coagulation, it is known that the formation of fibrin protein, which enhances its adhesion and the framework of a thrombus during the formation of platelets, depends in parallel on the concentration of calcium ions. For this reason, a feature of the "HEMOBEN" composition is the presence of easily decomposable calcium ions in it, which further accelerates the stopping of bleeding in the affected area upon contact with blood. This has been shown by the above studies. According to our data, a new domestic wound coating made of cellulose derivatives with prolonged action has a good hemostatic effect when modeling parenchymal bleeding from a spleen wound, providing the formation of a film with tight adhesion to the wound surface. At the same time, the initial application completely stops capillary bleeding, and additional application of the powder to a limited surface ensures complete hemostasis, eliminating the possibility of blood leakage with the formation of hematomas in the area of interest and blood congestion, as well as infection and inflammatory reaction from surrounding tissues.Unlike collagen protein hemostatic sponges, a fine powder formed by absorbable Na-carboxymethylcellulose (Na-CMC), viscose and calcium ions "HEMOBEN" attached to them when applied to parenchymal organ injuries provides full-fledged long-term hemostasis.
5. Conclusions
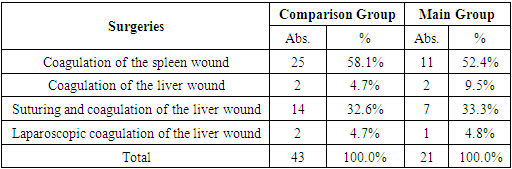
- Clinical evaluation of the use of the new domestic biocoating Hemoben showed an improvement in the local hemostatic effect in traumatic injuries of the liver or spleen parenchyma from 41.9% (18/43) of patients in the Comparison group to 71.4% (15/21) in the Main group.In the remaining 58.1% of cases of the Comparison group versus 28.6% of cases of the Main group (χ2=4,939; df=1; p=0.027), forced splenectomy (for the spleen injuries) and packing (areas of liver injury) were performed. There was a more pronounced decrease in the level of hemoglobin in the discharge from the drainage in dynamics (on the 3rd day up to 15.7±6.2 g/l in the Comparison group and up to 11.5±2.2 g/l in the Main group; t=3.80; p<0.05), as well as its volume (on the 3rd day up to 26.3±15.5 ml in the Comparison group and up to 15.5±5.1 ml in the Main group; t=4.43; p<0.05). It allowed to reduce the drainage duration from 5.8±2.2 days in the Comparison group to 4.3±2.1 days in the Main group (t=2.43; p<0.05), and, accordingly, to reduce the duration of the hospital stay from 8.3±1.6 days in the Comparison group to 6.9±1.4 days in the Main group (t=3.29; p<0.05).The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML