-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(6): 644-646
doi:10.5923/j.ajmms.20221206.07
Received: May 11, 2022; Accepted: May 29, 2022; Published: Jun. 13, 2022

Local Immunotropic Therapy for Lichen Planus of the Oral Mucosa
Umida Shukurova, Iroda Sadikova, Feruza Navruzova, Gulnoza Kasimova
Faculty Therapeutic Dentistry Department, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Umida Shukurova, Faculty Therapeutic Dentistry Department, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Inclusion of the IRS-19 spray into the complex of therapeutic measures for patients with lichen planus (LP) of the oral mucosa (OM) helps to stop pain, disappearance of erythema and edema, quickly resolve or reduce the number of nodular rashes and prevents the appearance of new ones, promotes epithelialization of erosive and ulcerative areas accelerates the onset of remissions, prevents relapses. 139 patients with LP OM aged 20-69 years were on outpatient treatment in the clinic of therapeutic dentistry of the Tashkent State Dental Institute for the period from 2020 to 2022. The state of the oral mucosa, the nature and presence of specific elements of the lesion, the severity of inflammatory and destructive processes in the epithelium of the oral mucosa, as well as the nature and frequency of specific complaints were assessed. Iin patients with a typical clinical form of LP OM in the main group, remission was achieved in 16 (88.89±7.71) patients, in the comparison group in 10 (55.56±11.71) (P<0.05). According to the results of our studies, we recommend the use of the immunostimulating drug IRS-19 in the complex therapy of patients with LP OM.
Keywords: Lichen planus, Oral mucosa, Immunostimulant, IRS-19
Cite this paper: Umida Shukurova, Iroda Sadikova, Feruza Navruzova, Gulnoza Kasimova, Local Immunotropic Therapy for Lichen Planus of the Oral Mucosa, American Journal of Medicine and Medical Sciences, Vol. 12 No. 6, 2022, pp. 644-646. doi: 10.5923/j.ajmms.20221206.07.
Article Outline
1. Introduction
- Lichen planus is a chronic polyetiological disease with rashes of papules on the mucous membranes and skin. To date, the problem of treating lichen planus (LP) is one of the important and unresolved problems of clinical dentistry. The most significant of the primary stages of the complex therapy of LP, in addition to etiotropic and pathogenetic therapy, is local conservative treatment [1,5,8,9].The arsenal of drugs used in local therapy for LP is quite wide, these are antiseptic solutions, enzymes, corticosteroids, immunomodulators, various combined biomaterials containing solcoseryl, proteolytic enzymes, vitamin preparations, etc. [2,3,5,6]. According to various sources, the effectiveness of local therapy in this category of patients remains low. The protracted chronic course of LP OM determines the need to search for safe methods of pathogenetically substantiated treatment with drugs that have an immunotropic effect [4,7,9].An immunostimulating drug based on bacterial lysates of IRS-19 increases specific and nonspecific immunity, leads to the rapid development of a local immune response. Specific protection is due to locally formed antibodies of the class of secretory immunoglobulins type A (IgA), which prevent the fixation and reproduction of infectious agents on the mucosa. Nonspecific immunoprotection is manifested in an increase in the phagocytic activity of macrophages, an increase in the content of lysozyme.
2. Object of Research
- The material for analysis and conclusions was the results of treatment of 139 patients with LP OM aged 20-69 years who were on outpatient treatment in the clinic of therapeutic dentistry of the Tashkent State Dental Institute for the period from 2020 to 2022.
3. Material and Methods of Research
- The diagnosis of LP OM was made on the basis of the classification of E.V. Borovsky, A.L. Mashkilleyson 2001. The treatment of LP OM was interrelated with the clinical severity of its course. In patients with LP OM, representative groups of patients were formed: the main group receiving IRS-19 as a local treatment and the comparison group receiving conventional treatment. Including with a typical form (36 patients - 18 main and 18 - comparison group); exudative hyperemic 34 patients (17 main and 17 comparison group) erosive and ulcerative 42 patients (21 main and 21 comparison group) and bullous form 27 patients (14 main and 13 control group).The comparison groups were randomized by sex, age and frequency of underlying somatic pathology, which ensured the representativeness of the data obtained during treatment.The state of the oral mucosa, the nature and presence of specific elements of the lesion, the severity of inflammatory and destructive processes in the epithelium of the oral mucosa, as well as the nature and frequency of specific complaints were assessed.Patients in the control groups were treated locally with proteolytic enzymes, keratoplastic agents, physiotherapeutic procedures were prescribed, antimicrobial agents (metronidazole), regenerating agents (solcoseryl dental adhesive paste) were widely used. It should be noted that, as a rule, 2 or more local agents were used in 1 patient.In the main groups, it was recommended to use IRS-19 as a local therapy according to the scheme: with a typical form: 1 dose 2 times a day for up to 2 weeks; exudative-hyperemic: 1 dose 3 times a day for up to 2-3 weeks; erosive-ulcerative and bullous: 1 dose up to 5 times a day for a month, repeat the course every 3 months.
4. The Results of the Study
- As a result of the ongoing complex therapy, positive clinical dynamics was noted both in the main groups and in the comparison groups. An objective examination of patients showed a decrease in erythema, a decrease in the number of papular elements, a decrease in inflammation of the oral mucosa, a decrease in the area of erosions and their epithelization, and a transformation of a more severe form into a less severe one was noted.The most rapid regression of local manifestations of LP OM was noted in the main groups (P<0.05). So, in a typical form, the regression of subjective sensations was noted on days 3.81-6.11 after the start of treatment (in the comparison group - on days 5.31-8.32); with exudative-hyperemic form, respectively, on 5-8 days and 7-11 days; erosive-ulcerative form - at 7-12 and 12-22 days and with bullous form - at 8-12 and 14-20.At the same time, in patients with a typical clinical form of LP OOM in the main group, remission was achieved in 16 (88.89±7.71) patients, in the comparison group in 10 (55.56±11.71) (P<0.05); the corresponding ratios in patients with exudative-hyperemic form were 14 (82.35±9.25%) versus 8 (47.06±12.11%) (P<0.05); erosive and ulcerative 13 (61.90±10.60%) versus 6 (28.57±9.85%) (P<0.05); and bullous form 7 (50.0±13.36%) versus 2 (15.38±10.0%) (P<0.05).It should be noted that in the main groups there were no patients who had no positive dynamics of local clinical symptoms (no effect), and in the comparison groups in patients with erosive and ulcerative form, the number of such patients was 4 people (19.05±8.17%); with bullous form - 2 people (5.38±6.26%) (Fig. 1).
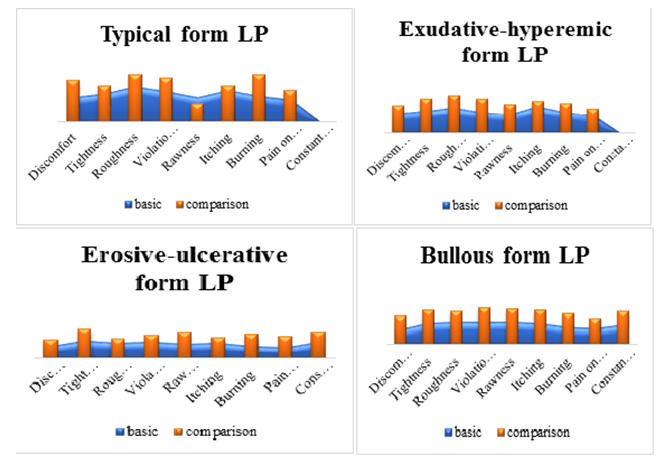 | Figure 1. Dynamics of complaints of patients with LP OM (days, M±m) in comparison groups |
5. Conclusions
- The results of measuring the concentration of cytokines in the oral fluid and blood serum before and after treatment indicate that in immunocompromised patients with LP OM, there is a distinct tendency to restore the changed indicators characterizing the activity of pro- and anti-inflammatory protection. A comparative analysis of the effectiveness of restoring the balance of cytokines in the main group and the comparison group showed that a more pronounced restoration of immune deficiency was noted in the main groups. The inclusion of IRS-19 spray in the complex of therapeutic measures for patients with LP of the oral mucosa contributes to the cessation of pain, the disappearance of erythema and edema, the rapid resolution or reduction in the number of nodular rashes and prevents the appearance of new ones, promotes the epithelization of erosive and ulcerative areas, accelerates the onset of remissions, prevents relapses. According to the results of our studies, we recommend the use of the immunostimulating drug IRS-19 in the complex therapy of patients with LP OOM.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML