-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(6): 639-643
doi:10.5923/j.ajmms.20221206.06
Received: May 10, 2022; Accepted: Jun. 1, 2022; Published: Jun. 13, 2022

Use of NGAL and IL-18 as a Biomarker of Acute Kidney Injury in Sepsis
V. Kh. Sharipova, N. F. Berdiev, M. I. Jabborova, Sh. E. Khaydarov
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim of the research was to studydiagnostic andprognostic values of blood NGAL, urine IL-18 in patients with septic shock. Background. Acute kidney injury is common in critically ill patients and is associated with increased morbidity, mortality and financial costs. Clinical signs and routine laboratory parameters such as urine output and serum creatinine are late signs of kidney injury. The study and implementation of new markers with high specificity in the early stages of kidney injury is a time requirement. Neutrophil gelatinase associated lipocalin (NGAL) and Interleukin 18 (IL-18) are such markers. Materials and methods. 103 patients (65 men and 38 women, mean age 65.3±8.8 years) were examined with a diagnosis of sepsis complicated by septic shock in the Department of ICU at the Republican Research Centre of Emergency Medicine for the period from 2019 to 2021. Acute kidney injury was diagnosed according to the criteria of Kidney Disease Improving Global Outcomes (KDIGO). The level of blood NGAL and urine IL-18 in patients was determined upon admission to the hospital and 12.36 hours after admission to the intensive care unit. According to the results of the biomarker analysis, all patients were divided into two groups: group 1 - positive biomarkers (BM+) and group 2 - negative biomarkers (BM-). This test system is based on the method of quantitative sandwich enzyme immunoassay. To analyze the predictive ability of NGAL and IL-18, we used Area Under Receiver Operating Characteristic Curve (AUROC) method of binary logistic regression and calculation. Results. Acute kidney injury was developed in those patients whose concentration of biomarkers was significantly higher than in patients with a low content of biomarkers: (NGAL 556 ng/ml (341;988) in compare with 124 ng/ml (91,3:185.3) P <0.001 and IL-18 - 376 ng/ml (98,5:1280) than 23,8 ng/ml (9,7:101.7) P <0.001, respectively). A ROC analysis was performed to predict acute kidney injury. The AUROC for NGAL concentration was 0.81 (95% confidence interval (CI): 0.63–0.95) with a sensitivity of 72.7% and a specificity of 86.1%, IL-18 was 0.75 (95% CI: 0.52–0.93) with a sensitivity of 64.1% and a specificity of 87.4%. Conclusion. The level of NGAL and IL-18 is a highly specific marker of early detection of Acute kidney injury in critical patients with sepsis.
Keywords: Acute kidney injury, Biomarker, IL-18, NGAL, KDIGO, Septic shock
Cite this paper: V. Kh. Sharipova, N. F. Berdiev, M. I. Jabborova, Sh. E. Khaydarov, Use of NGAL and IL-18 as a Biomarker of Acute Kidney Injury in Sepsis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 6, 2022, pp. 639-643. doi: 10.5923/j.ajmms.20221206.06.
1. Introduction
- Acute kidney injury (AKI) is a polyetiological syndrome, which is a sudden decrease in kidney function for several days or weeks, causing the accumulation of nitrogenous compounds in the blood, with or without a decrease in diuresis. AKI is common in hospitalized patients and is associated with increased morbidity, mortality and financial costs. According to various authors, AKI occurs in 35-70% of patients in intensive care units (ICU) and is most often observed in patients with septic shock [1-2].Currently, the diagnostics of AKI is determined according to the KDIGO guidelines based on changes in serum creatinine concentration or urine output, although their shortcomings are known in clinical practice [3]. The kidneys have a significant functional reserve and creatinine concentration at AKI can remain within the normal range until 50% of nephrons are lost [4]. Oliguria is an undoubted sign of severe kidney injury [5]. On the other hand, oliguria may be associated with some clinical conditions, such as prolonged fasting, hypovolemia, after major surgery and severe trauma [6]. Late diagnosis and treatment of AKI can lead to irreversible kidney injury.Currently, researches are underway to find more accurate markers of early diagnosis of AKI worldwide. The search for new AKI biomarkers would allow to diagnose pathology, the level of damage at the earliest possible time, and timely apply therapeutic and rehabilitation measures to prevent the development of chronic kidney disease (CKD) [7]. NGAL and IL-18 are highly specific biomarkers for early detection of AKI in patients in critical conditions.Several studies have shown that NGAL is formed in the kidneys after ischemic or nephrotoxic injury [8]. NGAL is elevated in the blood of patients with AKI within 2 hours and reaches a peak approximately 6 hours after AKI [9]. Maximum concentrations can be sustained within 5 days [10]. IL-18 is produced in urine by the epithelium of the proximal tubules under the influence of damaging factors [11]. Urinary IL-18 is an early predictive biomarker for AKI in the ICU [12]. The concentration of IL-18 is increased 24-48 hours before AKI and its concentration is kept for 96 hours.Aim of the research was to study diagnostic and prognostic values of blood NGAL, urine IL-18 in patients with septic shock.
2. Material and Methods
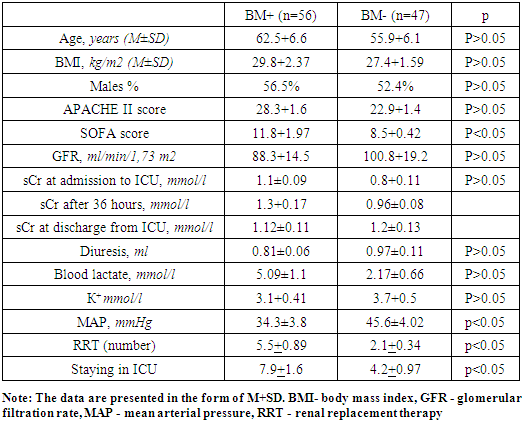
- 121 patients were admitted with a diagnosis of sepsis to the Intensive Care Unit of the Republican Research Center of Emergency Medicine for the period from 2019 to 2021. 103 patients (65 males and 38 females) were included in this study. The mean age of the patients was 65.3±8.8 years. All patients were divided into two groups. Group I included 56 patients with high levels of NGAL and IL-18 (BM+) biomarkers. Group II included 47 patients without biomarkers (BM-). The inclusion criteria for the study were as follows: the presence of diagnosed sepsis in the patient, as well as the availability of informed consent to participate in the study. The exclusion criteria were: age over 75 and under 18 years of age, presence of chronic renal failure, condition after kidney transplantation, pregnancy, the patient’s stay in the ICU for less than 24 hours (Fig. 1).
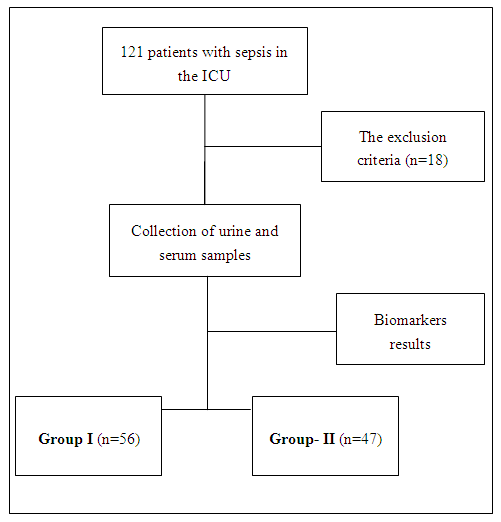 | Figure 1. Distribution of patients by groups |
3. Results
- Demographic and clinical characteristics of patients are presented in table 1.
|
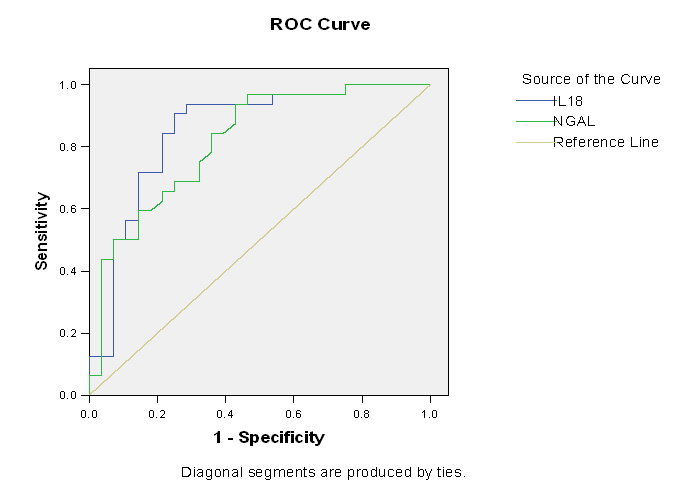 | Figure 2. ROC Curve for sNGAL and uIL-18 after 12 hours |
4. Discussion
- Biomarkers are one of the most informative indicators for the early diagnostics of AKI in patients with sepsis. An increase in its concentration in the urine indicates a high risk of developing AKI. Our study showed that AKI patients with such urinary biomarker level had a longer ICU stay than patients without AKI. Zdziechowska and other researchers found that high levels of uNGAL and uIL-18 were observed in patients with AKI (234-438 ng/mL at various points) [15].Recently, some studies have confirmed that uNGAL and uIL-18 are good prognostic and diagnostic biomarkers of AKI [16]. Kashani et al found that more severe renal complications, chronic renal dysfunction, higher risk of needing RRT, and higher mortality were seen in patients with high biomarkers than those with low levels. According to our data, severe renal complications and the need for RRT were observed in patients with high levels of biomarkers.According to some studies, a high concentration of BM is associated with an increase in the duration of stay in the intensive care unit [17]. Duration of stay in the intensive care unit was 3 times higher in patients with high levels of the biomarkers. ROC analysis was performed to predict AKI. AUROC for uNGAL concentration after 36 hours was 0.81 (95% CI:0.63–0.95) with sensitivity of 72.7% and specificity of 86.1%, IL-18 after 36 hours was 0.77 (95% CI:0.52–0.93) with sensitivity of 69.5% and specificity of 87.4%.According to our data, statistically significant correlations between urea (r=-0.342), creatinine (r=-0.342), age and volume of diuresis (r=-0.37 p>0.05) were found in patients with a high level of biomarkers. According to some studies, there were significant correlations between the concentration of uNGAL in the blood, the duration of stay in the ICU (r=0.86; p<0.05) and urine volume (r=-0.52; p>0.05) in septic patients [18-19].
5. Conclusions
- Based on our observations, it can be concluded that the determination of uNGAL and uIL-18 has prognostic and diagnostic significance in the early detection of AKI in septic patients. An increase in the concentration of NGAL and uIL- at normal creatinine levels indicates a subclinical AKI. High values of biomarkers in urine have a direct relationship in the development of AKI. The level of uNGAL and ul- in urine can be used as an early biomarker of AKI to make a decision on timely targeted therapy before the development of irreversible kidney injury.The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is being published for the first time and is a part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML