B. F. Mukhamedova, M. Kh. Nazarova, Sh. N. Salakhitdinov, B. O. Kazakov
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Aim of the study is to evaluate the organization and quality of emergency medicine for patients with acute coronary syndrome in the Republican Research Centre of Emergency Medicine for the period from 2019 to 2021.Introduction. Diseases of the circulatory system are the leading cause of death in the population and make up 63.2% of all death causes in Uzbekistan. The main diseases that form high mortality are coronary heart disease, myocardial infarction. Material and methods. Our study has been conducted at the Republican Research Center of Emergency Medicine. A retrospective analysis of the annual statistical reports of the Department of Emergency Cardiology and Therapy of the Republican Research Center of Emergency Medicine for 2019-2021 has been carried out to assess the immediate results of acute coronary syndrome and acute myocardial infarction treatment. Results. 3,302 men and 1,690 women with a diagnosis of acute coronary syndrome have been registered at the Republican Research Center of Emergency Medicine for three years (2019-2021). During the reporting period, percutaneous coronary interventions in the form of balloon angioplasty and stenting of the infarct-related artery were performed in 1,076 and 1,574, respectively. Regardless of the timing of primary percutaneous coronary interventions, stenting was performed in all cases. The mortality rate of patients diagnosed with acute myocardial infarction, including acute myocardial infarction with a Q wave, without a Q wave and repeated acute myocardial infarction decreased in the Republican Research Center of Emergency Medicine and made up 16.3% in 2021 (19.1% in 2019, 18.4% in 2020, respectively). Conclusion. The development and implementation of regional medical and economic standards with the priority application of X-ray endovascular technology in medical organizations in the city of Tashkent has improved the quality of care for patients with cardiovascular diseases and, first of all, to patients with acute myocardial infarction, including the high frequency of percutaneous coronary interventions in acute coronary syndrome.
Keywords:
Acute coronary syndrome, Thrombolysis, Percutaneous coronary intervention
Cite this paper: B. F. Mukhamedova, M. Kh. Nazarova, Sh. N. Salakhitdinov, B. O. Kazakov, Organization of Emergency Medicine for Patients with Acute Coronary Syndrome in the Republican Research Centre of Emergency Medicine from 2019 to 2021, American Journal of Medicine and Medical Sciences, Vol. 12 No. 6, 2022, pp. 609-615. doi: 10.5923/j.ajmms.20221206.04.
1. Introduction
Diseases of the circulatory system are the leading causes of high morbidity and mortality in many countries of the world, including the Republic of Uzbekistan, and largely determine the state of public health and healthcare system. Mortality from the circulatory system diseases is dominant in the structure of total mortality in all developed countries and tends to increase [1-2]. There is a negative trend towards an increase in the incidence of the circulatory system diseases and high mortality from cardiovascular diseases (CVDs) in many regions of the country, including in the economically developed, densely populated subject of the Republic of Uzbekistan - the city of Tashkent [3-4].The issue of continuous improvement of diagnostics, treatment and prevention of the cardiovascular system various diseases, including surgical methods of correction of these disorders, remains relevant in our country [5-6]. In particular, the Action Strategy for the five priority areas of development of the Republic of Uzbekistan for 2017-2021 provides for the following tasks: "... improving the availability and quality of specialized medical care to the population, as well as reforming the system of emergency medicine, disability prevention [7-8]. Based on mentioned above, one of the relevant directions is to determine the optimal tactics for the treatment of patients with acute coronary syndrome (ACS) [9-10]. To solve the problem of ultra-high mortality from ACS in the Republic of Uzbekistan, the Government Decree adopted Order No. 341 dated by December 18, 2020 "On improving the organization of emergency medical care for patients with acute coronary syndrome in Tashkent" to provide the most effective care to patients with coronary heart disease, in terms of reducing mortality and disability, significant investments were made in the development of cardiology services of Tashkent. The main strategic direction of this document is to provide the population with high-tech medical care at urgent cardiac conditions. Aim of the study is to evaluate the organization and quality of emergency medicine for patients with acute coronary syndrome in the Republican Research Centre of Emergency Medicine for the period from 2019 to 2021.
2. Material and Methods
Our study was conducted at the Republican Research Center of Emergency Medicine (RRCEM). RRCEM is a multidisciplinary hospital providing free emergency specialized medical care in all major areas of emergency medicine - surgical, therapeutic, burn and toxicological profiles for adults and children around the clock. The center is designed for 680 beds. Besides, there are 80 beds in the intensive care units.A retrospective analysis of the annual statistical reports of the Department of Emergency Cardiology and Therapy of the RRCEM for 2019-2021 has been carried out to assess the immediate results of acute coronary syndrome (ACS) and acute myocardial infarction (AMI) treatment.
3. Results
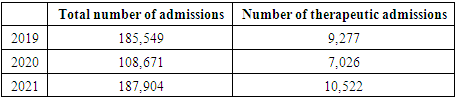
187,904 patients admitted to the Center for emergency medical care: among them the number of patients with a therapeutic profile made up 10,522 people (Tab. 1) in 2021.Table 1. Number of patients admitted to RRCEM (2019-2021)
 |
| |
|
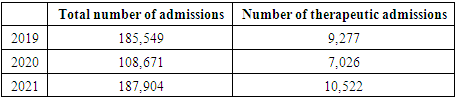
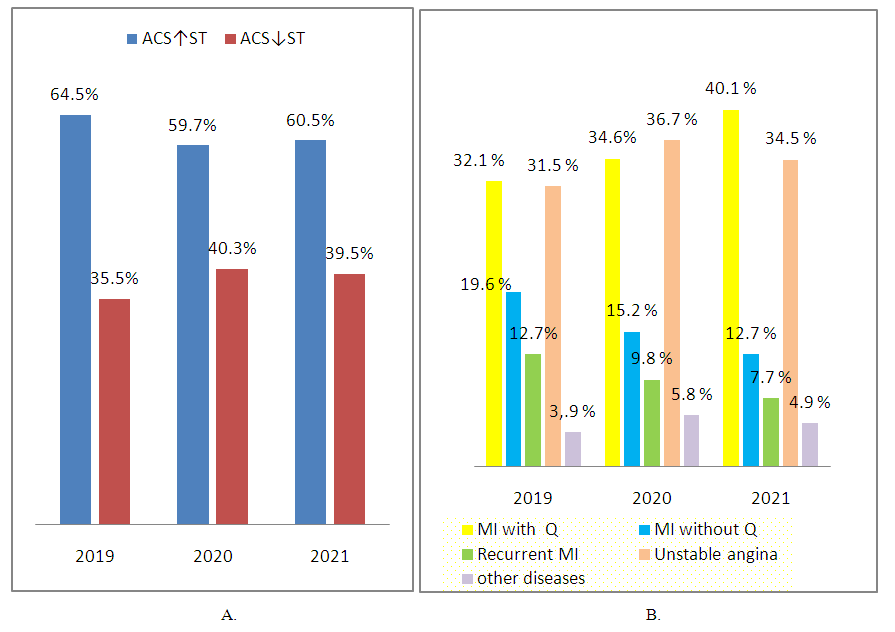
Basically, they were patients with acute coronary syndrome (2074): the number of ACS cases with ST segment elevation (ACS↑ST) was 60.5% (1256); patients with ACS without ST elevation (ACS↓ST) made up 39.5% (818). MI with Q-wave was developed in 40.1% (831) cases of ACS↑ST outcomes; MI without Q- wave – in 12.7% (265) patients; recurrent MI – in 7.7% (160) cases; unstable angina (UA) – in 34.5% (715) patients; other diseases – in 4.9% (103) cases.108,671 patients admitted to the RRCEM for emergency medical care in 2020 and 7,026 people among them were patients of a therapeutic profile. As it has been shown in the table, the total number of admissions at the RRCEM in 2021 increased by 1.73 times in compare with 2020 and the number of patients of the therapeutic profile increased by 1.49 times [11-12].10,522 admissions with ACS were registered at the RRCEMP in 2020: The number of cases of ACS with ST segment elevation (ACS↑ST) made up 627 (59.7%) patients; ACS without ST elevation (ACS↓ST) was detected in 423 (40.3%) cases. MI with Q-wave was developed in 364 (34.6%) cases; MI without Q-wave – in 160 (15.2%) patients; recurrent MI – in 103 (9.8%) cases; UA – in 385 (36.7%); other diseases – in 61 (5.8%) cases.Due to the declared COVID-19 pandemic, many multi-specialty hospitals, including RRCEM, were re-designated into a coronavirus center. 185,549 people admitted to the RRCEM for emergency medical care in 2019. The number of patients of a therapeutic profile made up 9,277 people. Table 1 shows that the total admission to the RRCEM in 2020 was decreased by 1.7 times in compare with 2019, and the admissions of the therapeutic profile were reduced by 1-3 times. 1,888 cases with ACS were registered in the RRCEM in 2019: the number of patients with ACS↑ST made up 1,218 (64.5%), ACS↓ST was detected in 670 (35.5%) patients (Fig.1, A). MI with Q-wave was developed in 607 (32.1%) cases; MI without Q-wave – in 371 (19.6%) patients; recurrent MI – in 240 (12.7%) cases; UA – in 596 (31.5%) patients; other diseases – 74 (3.9%) (Fig.1, B).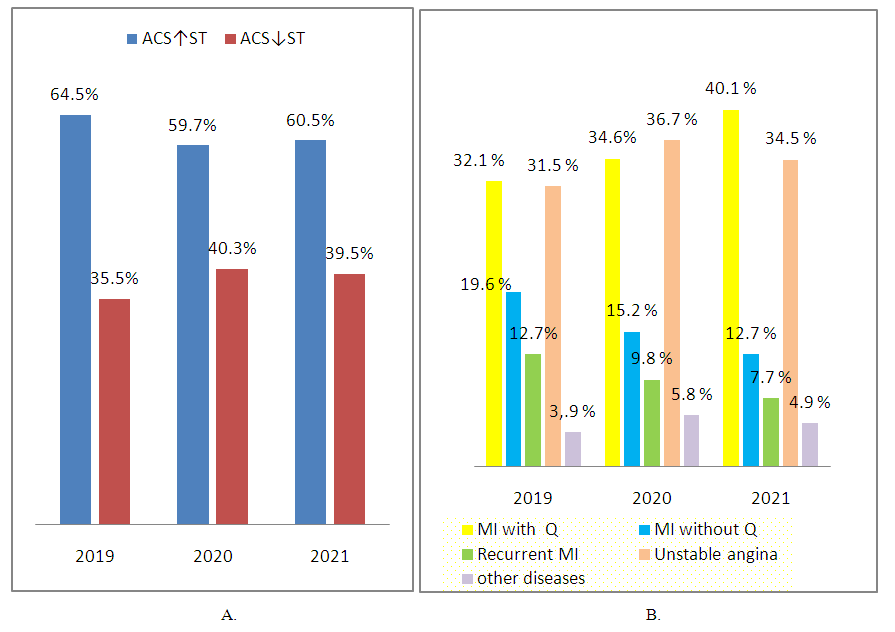 | Figure 1. ACS occurrence frequency |
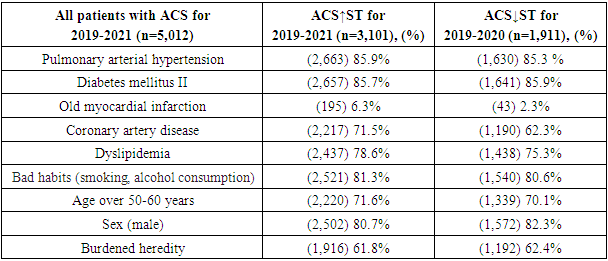
ACS is a polyethological disease, in the occurrence and progression of which many external and internal factors, called risk factors (RFs), are important [13-15]. Currently, more than 30 factors are known. The most significant of them are the following ones [16-17]:1. Non-modifiable (immutable) RFs;• Age over 50-60 years• Sex (male)• Burdened heredity2. Modifiable (changeable) RFs;• Dyslipidemia• Pulmonary arterial hypertension (PAH)• Smoking• Obesity• Carbohydrate metabolism disorders• Hypodynamia• Irrational nutritionHyperhomocysteinemia, etc.The study revealed that 85.7% of patients with ACS had a history of PAH, diabetes mellitus (DM). 78.6% of patients had obesity of II, III. 81.3% of patients had bad habits (smoking, alcohol consumption). A high incidence of coronary heart disease, myocardial infarction occurred in patients with ACS↓ST [18-21] (Tab. 2). Table 2. Anamnestic data on diseases preceding ACS
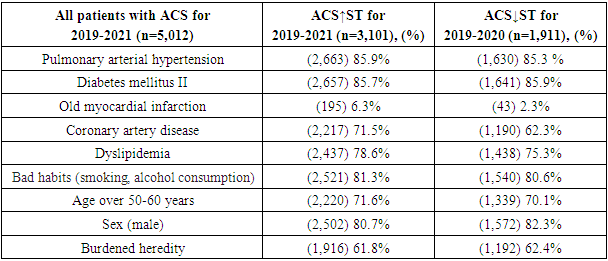 |
| |
|
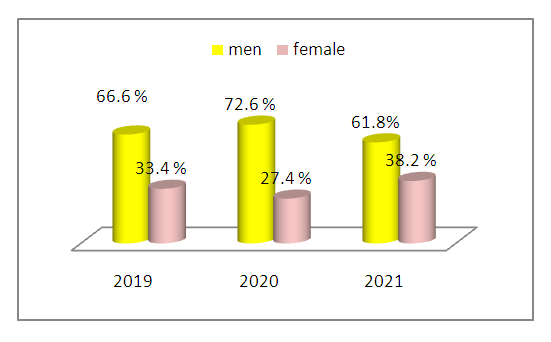
3,302 males and 1,690 females with a diagnosis of ACS were registered in the RRCEM for the period from 2019 to 2021 (in 2019 – 1,257 males (66.6%), 631 females (33.4%); in 2020 - 763 males (72.6%), 267 females (27.4%); in 2021 -1,282 males (61,8%), 792 females (38,2%)) (Fig. 2).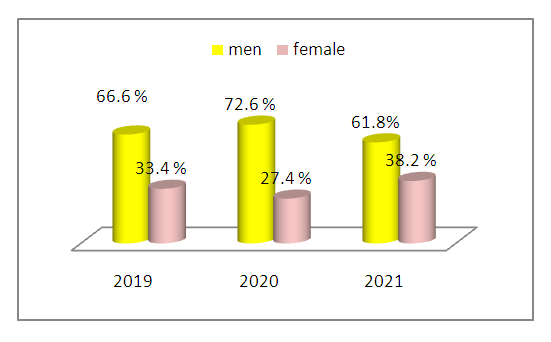 | Figure 2. Distribution of patients by sex |
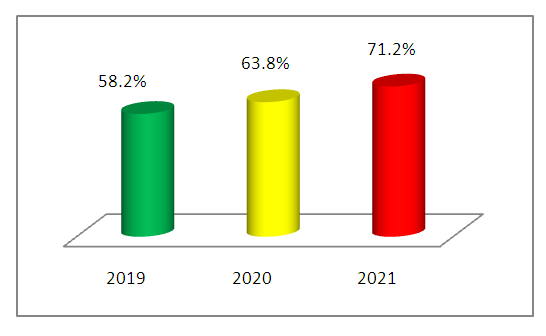
An analysis of the patients' admission to RRCEM with ACS by regions in 2019 showed that 1,100 (58.2%) of patients were residents of Tashkent city. This value made up 669 (63.8%) cases in 2020. The number of Tashkent residents admitted to the RRCEM with ACS diagnosis was 1,476 (71.2%) people in 2021 (Fig. 3). 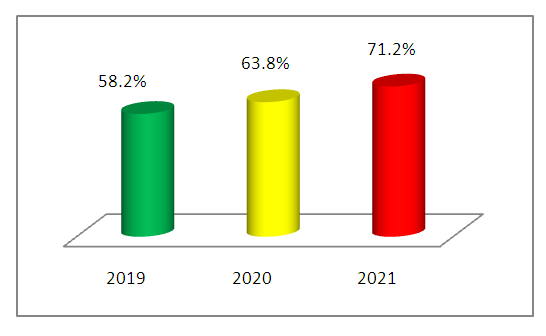 | Figure 3. The number of Tashkent residents admitted to the RRCEM with ACS |
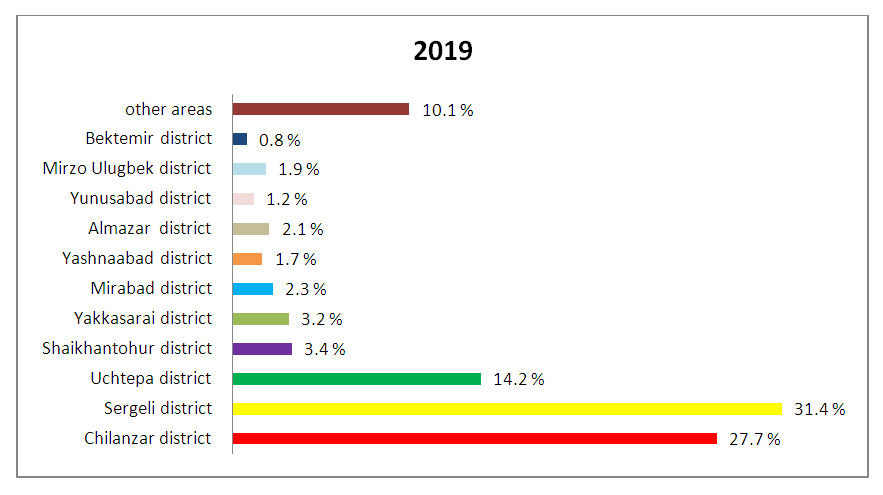
There were 11 districts in the capital of Uzbekistan until May, 2020. The largest proportion of residents of Tashkent city admitted to the RRCEM with ACS in 2019 were residents of the following districts: Chilanzar district (27.7%), Sergeli district (31.4%), Uchtepa district-14.2%. The number of residents from other regions of the Republic of Uzbekistan made up 10.1%. (Fig. 4).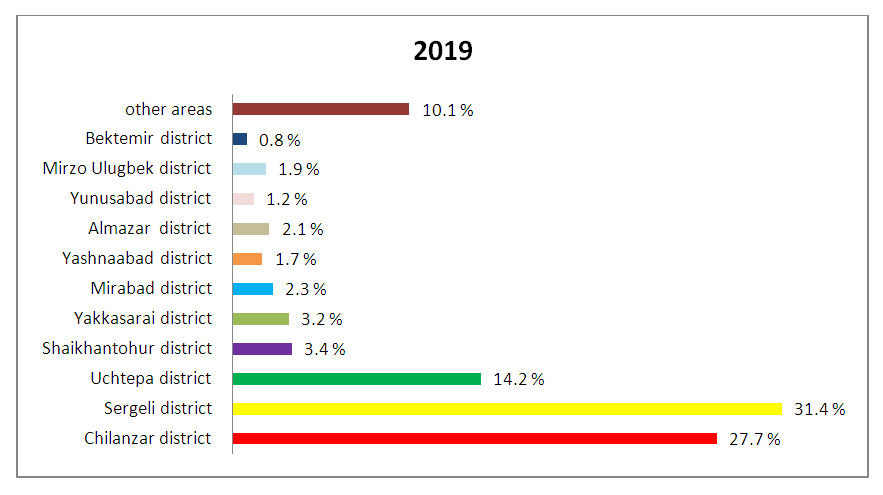 | Figure 4. The proportion of Tashkent city residents admitted to the RRCEM in 2019 |
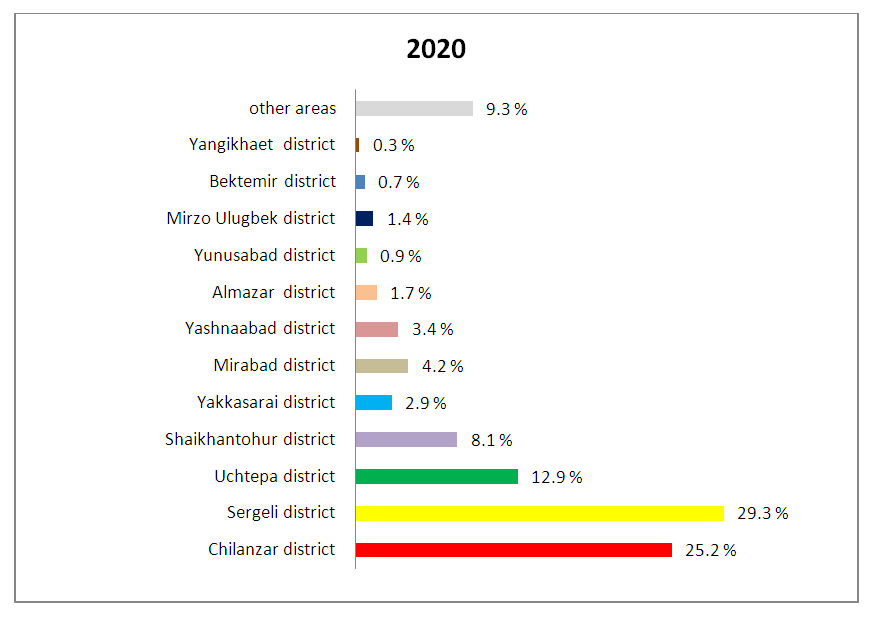
In May 2020, a new Yangikhayot district was created in Tashkent. In 2020, the proportion of residents of Tashkent admitted to the RRCEM was distributed as follows: Chilanzar district-25.2%, Sergeli district-29.3%, Uchtepa district-12.9%, from other regions of the country - 9.3% (Fig. 5).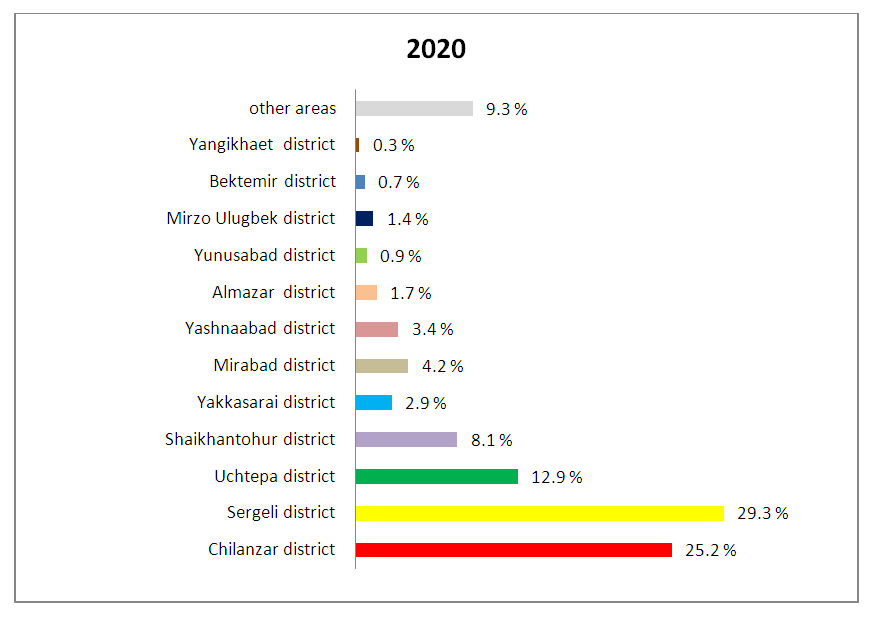 | Figure 5. The proportion of Tashkent city residents admitted to the RRCEM in 2020 |
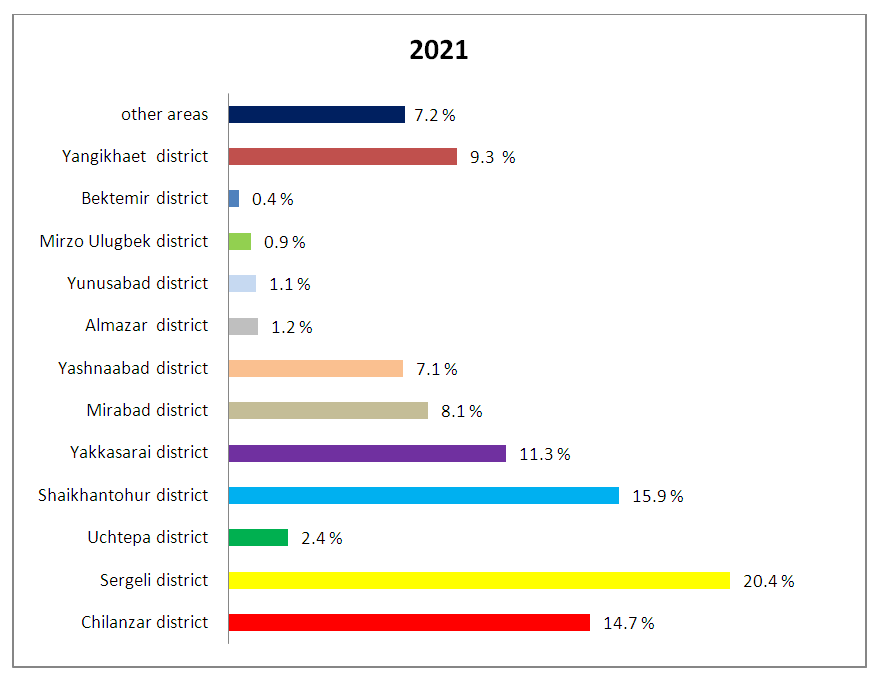
For the period from 2019 to 2020, the largest number of cases with a diagnosis of ACS was recorded among residents of two districts of Tashkent city - Chilanzar and Sergeli. The fact is that until 2020, only residents of these two districts with ACS admitted to RRCEM, they underwent emergency percutaneous coronary intervention (PCI) only until 14.00 on a working day. Residents of other districts with a diagnosis of ACS admitted to other hospitals. The main method of reperfusion treatment used was thrombolytic therapy.As part of the implementation of the Government Decree dated by December 18, 2020 No. 341 “On improving the organization of emergency medical care for patients with acute coronary syndrome in Tashkent”, in order to provide the most effective, in terms of reducing mortality and disability of patients with coronary artery disease, significant investments have been made in the development of craniological services in Tashkent. According to Order No. 341, effective emergency medical care is provided to patients diagnosed with ACS and ST segment elevation in the following medical institutions:- at the Republican Scientific Center of Emergency Medicine (RNCEMP) (24\7); - at the Republican Specialized Scientific and Practical Medical Center of Cardiology (RSSPMCC) and at the Republican Specialized Scientific and Practical Medical Center of Surgery (RSSPMCS) from 9.00. service posts function until 17.00 to provide patients with primary percutaneous coronary intervention. The highest rates of admissions with a diagnosis of ACS in 2021 were fixed in the following districts of Tashkent: Sergeli (20.4%), Shaikhontokhur (15.9%) and Chilanzar (14.7%) districts (Fig. 6).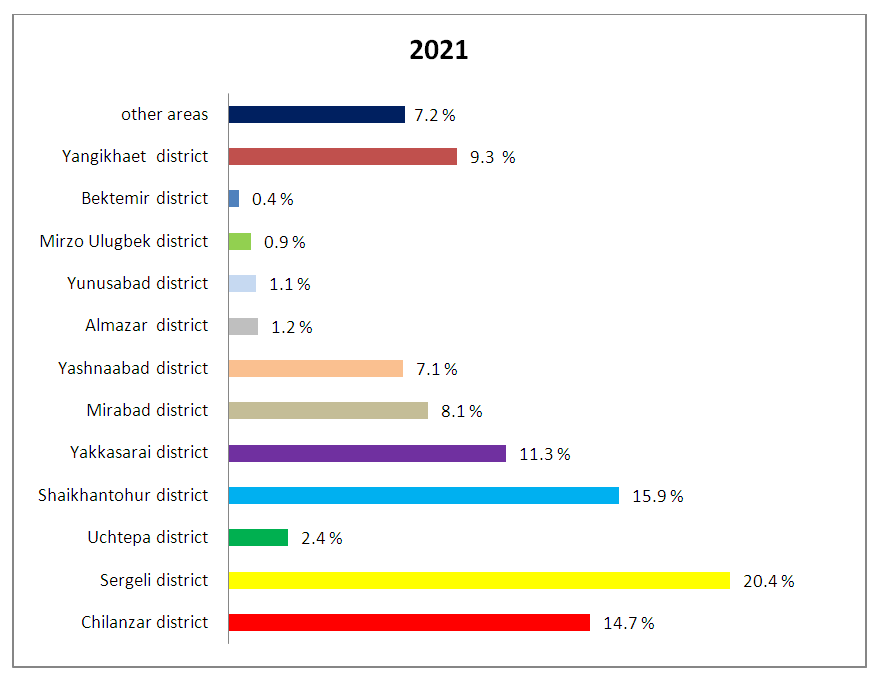 | Figure 6. The proportion of Tashkent city residents admitted to the RRCEM in 2021 |
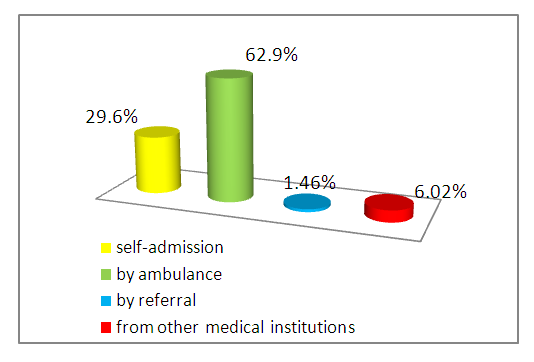
5,012 patients with a diagnosis of ACS admitted to the RRCEM in 2019-2021: self-admission – 1,483 (29,6%), by ambulance -3,152 (62,9%), by referral - 73 (1,46%), from other hospitals - 301 (6,02%) (Fig. 7). 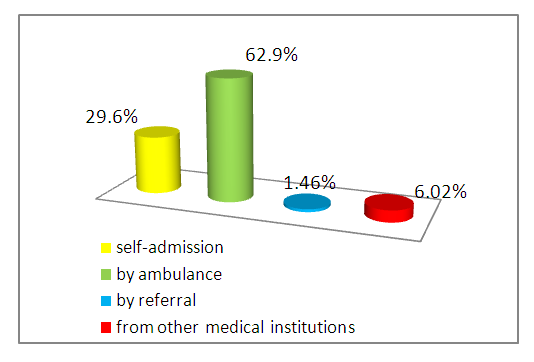 | Figure 7. Ways of patients’ admissions to the RRCEM |
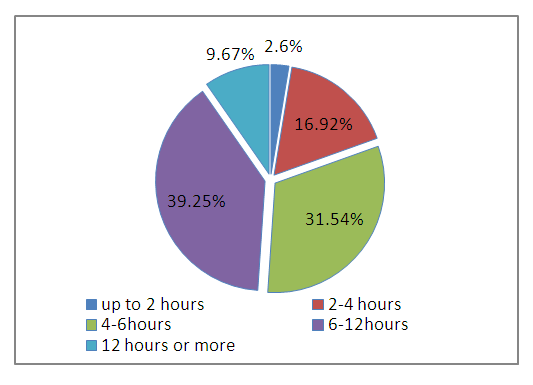
The study revealed that 130 (2.6%) patients with ACS were admitted up to 2 hours from the onset of the disease, within 2-4 hours - 847 (16.9%), 4-6 hours - 1,578 (31.5%), 6-12 hours – 1,964 (39.2%), 12 hours or more - 488 (9.66%) patients with ACS (Fig. 8).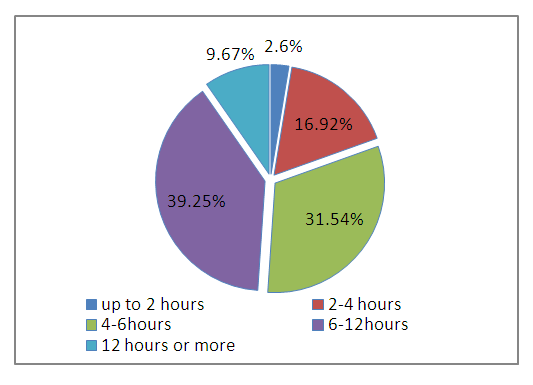 | Figure 8. Time of ACS patients’ admission to the RNCEMP |
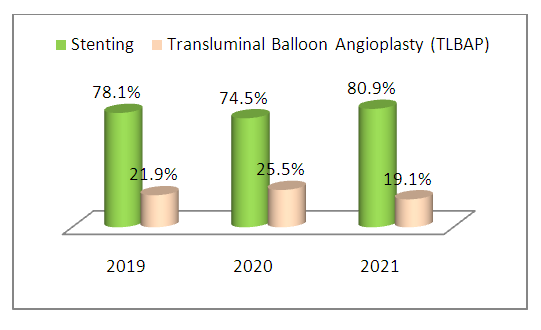
Percutaneous coronary interventions in the form of balloon angioplasty and stenting of a connected artery infarction have been performed for three years in 1,076 and 1,574 patients, respectively. Regardless of the timing of primary percutaneous coronary interventions, stenting was performed in all cases (Fig. 9).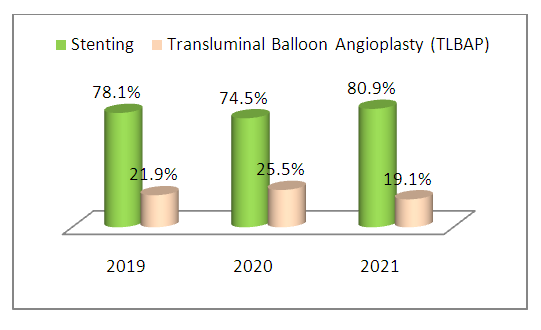 | Figure 9. Primary PCI depending on the strategy of their use |
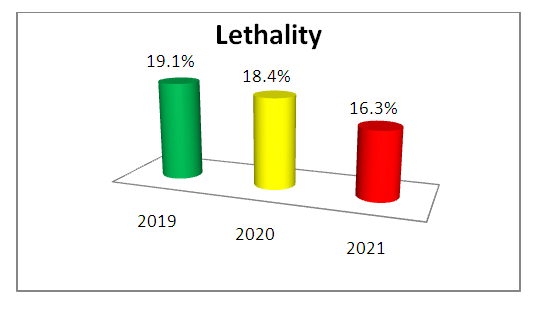
In the RNCEMP, the mortality rate of patients diagnosed with AMI, including AMI with a Q wave, without a Q wave and recurrent AMI decreased and reached 16.3% in 2021 (19.1% - in 2019, 18.4% - in 2020, respectively) (Fig. 10).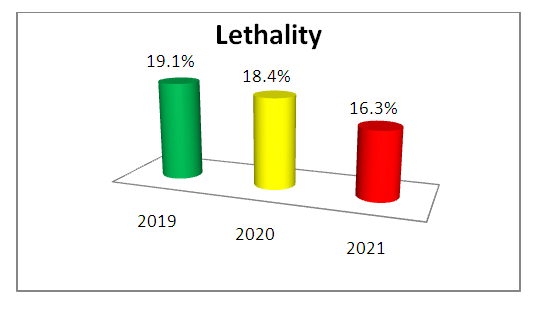 | Figure 10. The frequency of hospital mortality in patients with ACS |
4. Discussion
Analysis of the organizing and quality of medical care in dynamics at the RRCEM for patients with ACS for 2019-2021 showed that the number of patients with ACS↑ST was 1.5 times higher than the number of patients with ACS↓ST. MI with Q-wave was developed in 40.1% (831) cases of ACS↑ST outcomes, MI without Q-wave - in 12.7% (265) and recurrent MI – in 7,7% (160) cases. 85.7% of patients with ACS had a history of PAH, diabetes mellitus (DM). There was obesity of II, III in 78.6% of patients. Smoking, alcohol consumption was registered in 81.3% of patients.A larger proportion of patients with ACS were men (66.6%).When analyzing the admission of patients with ACS from the regions of Uzbekistan, it was revealed that 71.2% were residents of Tashkent. The number of PCI performed in the RRCEM increased by 12.9% for 2019-2021 (stenting – 15.7%, transluminal balloon angioplasty (TLBAP) - 9.8%).The mortality rate of patients diagnosed with AMI (with a Q wave, without a Q wave and recurrent AMI) decreased from 19.1% in 2019 to 16.3% in 2021.
5. Conclusions
The development and implementation of regional medical and economic standards with the priority use of X-ray endovascular technology in medical organizations of Tashkent city has improved the quality of care for patients with cardiovascular diseases and, first of all, to patients with acute myocardial infarction, including a high frequency of percutaneous coronary interventions at acute coronary syndrome [22,11].The efficiency of the introduction of percutaneous coronary interventions in regional medical organizations is confirmed by the improvement of the quality of life of patients with acute myocardial infarction, both social and public health indicators [23,13].The development of the X-ray endovascular care system contributed to the improvement of the structural and functional foundations of healthcare in Tashkent in accordance with the objectives of the National Programs of the Republic of Uzbekistan in the field of health and healthcare.The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
References
| [1] | Abdujamalova N.M. et al. Mechanisms of development of restenosis in the stent of the coronary arteries in patients with coronary heart disease. In Russian // Cardiol. vestn. – 2016. – V. 11, № 2. – P. 100-103. |
| [2] | Barbarash O.L. et al. Approaches to the diagnosis and treatment of patients with non-ST elevation acute coronary syndrome in Russian hospitals. Results of the RECORD-3 register. In Russian // Sib. med. J – 2017. – V. 32, №3. – P. 88-94. |
| [3] | Ibragimov R.U. The results of stenting the trunk of the left coronary artery in patients with stable coronary heart disease using stents with biodegradable and permanent polymers. In Russian // Patol. circulation and cardiac surgery. – 2018. – V. 22, №3. – P. 49-55. |
| [4] | Karimov A.M., Abdullaev T.A., Tsoi I.A., Fozilov Kh.G. Features of coronary vascular lesions in patients with coronary artery disease with reduced LV EF and type 2 diabetes mellitus. In Russian // Cardiology of Uzbekistan. – 2018. – №4. – P. 40-44. |
| [5] | Stoyko O.A. Clinical and prognostic value of residual platelet activity in patients with acute coronary syndrome without ST segment elevations: Dis. … Dr. med. Sciences. In Russian – Tyumen, 2018. |
| [6] | Urinov O., Mamutov R.Sh. Compliance to therapy of patients with acute coronary pathology during a 6-month follow-up. In Russian // Cardiology of Uzbekistan. – 2018. – №2. – P. 99. |
| [7] | Martsevich S.Yu. mRegister of acute coronary syndrome LIS-3: what has changed over the past years in the "Portrait" of the patient and the immediate outcomes of the disease in comparison with the register LIS-1. In Russian// Rational pharmacotherapy in cardiology. – 2017. – V. 13, №1. – P. 63-68. |
| [8] | Osipova E.S., Veselovskaya N.G., Chumakova G.A. Risk factors for coronary artery restenosis after stenting in women with obesity during menopause. In Russian // Russian cardiologic journal - 2018. - V. 23, No. 5. - P. 34-39. |
| [9] | Vershinina E.O. Long-term outcomes of planned endovascular interventions on the coronary arteries. In Russian // Cardiology. – 2018. – V. 58, №7. – P. 5-13. |
| [10] | Dorokhova O. V. et al. Risk factors for adverse coronary events in patients with non-ST elevation acute coronary syndrome and type 2 diabetes. In Russian // Vestn. of Ivanovo med. acad. – 2014. – V. 19, №1. – P. 30-33. |
| [11] | Shames D.V., Galyavich A.S., Galeeva Z.M. Restenoses after stenting of the coronary arteries: risk factors for occurrence, potential for prevention, methods of elimination. In Russian // Urgent Cardiol. – 2017. – Т. 3. – P. 38-46. |
| [12] | Erlikh A.D. Relationship between the degree of coronary lesion and stenting characteristics with short-term and long-term outcomes in patients with acute coronary syndrome (data from the RECORD-3 registry). In Russian // Kardiologiya. – 2018. – V. 58, №5. – P. 5-12. |
| [13] | Paramasivam G. et al. In-stent restenosis of drug-eluting stents in patients with diabetes mellitus: Clinical presentation, angiographic features, and outcomes // Anatolian J. Cardiol. – 2020. –Vol. 23, №1. – P. 28-34. |
| [14] | Reynolds K. Trends in incidence of hospitalized acute myocardial infarction in the Cardiovascular Research Network (CVRN) // Amer. J. Med. – 2017. – Vol. 130, №3. – P. 317-327. |
| [15] | Riegger R.A. et al. Histopathological evaluation of thrombus in patients presenting with stent thrombosis. A multicenter European study: a report of the prevention of late stent thrombosis by an interdisciplinary global European effort consortium // Europ. Heart J. – 2015. – Vol. 37, №19. – P. 1538-1549. |
| [16] | Ahrens I. et al. Invasive and antiplatelet treatment of patients with non-ST-segment elevation myocardial infarction: Understanding and addressing the global risk‐treatment paradox // Clin. Cardiol. – 2019. – Vol. 42, №10. – Р. 1028-1040. |
| [17] | Berwanger O. Effect of loading dose of atorvastatin prior to planned percutaneous coronary intervention on major adverse cardiovascular events in acute coronary syndrome: the SECURE-PCI randomized clinical trial // J.A.M.A. – 2018. – Vol. 319, №13. – P. 1331-1340. |
| [18] | Candela E. Conservatively managed patients with non-ST-segment elevation acute coronary syndrome are undertreated with indicated medicines // PloS One. – 2018. – Vol. 13, №11. – P. e0208069. |
| [19] | Canpolat U. et al. Impact of free thyroxine levels and other clinical factors on bare metal stent restenosis // Arch. Endocrinol. Metab. – 2017. – Vol. 61, №2. – P. 130-136. |
| [20] | Gallo G. et al. Role of oxidative stress in the process of vascular remodeling following coronary revascularization // Int. J. Cardiol. – 2018. – Vol. 268. – P. 27-33. |
| [21] | Gori T. et al. Predictors of stent thrombosis and their implications for clinical practice // Nat. Rev. Cardiol. – 2018. – Vol. 16, №4. – P. 243-256. |
| [22] | Staroverov I.I. Eurasian Clinical Guidelines for the Diagnosis and Treatment of ST-Elevation Acute Coronary Syndrome (ST elevation ACS). In Russian // Evraziyskiy Kardiol. J – 2020. – №1. – P. 4-77. |
| [23] | Beyer C. et al. Effects of hyperthyroidism on coronary artery disease: a computed tomography angiography study // Canad. J. Cardiol. – 2017. – Vol. 33, №10. – P. 1327-1334. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML