Khamdamov Ilhomjon Bakhtiyorovich
Bukhara State Medical Institute Named after Abu Ali Ibn Sino, City of Bukhara, Republic of Uzbekistan
Correspondence to: Khamdamov Ilhomjon Bakhtiyorovich, Bukhara State Medical Institute Named after Abu Ali Ibn Sino, City of Bukhara, Republic of Uzbekistan.
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article presents the results of hernioplasty for ventral hernias in women of fertile age. Currently, there are no clear recommendations on the choice of the type of alloprosthesis for repair of hernias of the anterior abdominal wall. These questions remain debatable and open for women of childbearing age, and even more so during pregnancy. In our experience, we use composite mesh as described above for all hernias of the anterior abdominal wall. Of course, at present there are no specific studies to determine the individual histocompatibility of alloprostheses, however, this issue remains the subject of future research.
Keywords:
Women of fertile age, Abdominal hernias, Hernioplasty, Implant
Cite this paper: Khamdamov Ilhomjon Bakhtiyorovich, Evaluation of the Efficiency of an Improved Approach in the Treatment of Anterior Abdominal Wall Hernias in Women of Fertile Age, American Journal of Medicine and Medical Sciences, Vol. 12 No. 5, 2022, pp. 584-588. doi: 10.5923/j.ajmms.20221205.27.
1. Introduction
External abdominal hernias are one of the most common surgical diseases. The incidence increases from year to year, remaining consistently high, and is 14 patients per 1000 of the population aged 25 to 34; gradually increasing, it reaches 53 per 1000 of the population aged 55 to 64 years [1,2,5,6,8,12]. The history of herniology has more than a century of duration. The earliest mention of hernias as "... a tumor-like formation that appears on the surface of the abdomen as a result of coughing or straining" was found in the Ebers Papyrus, written around 1552 BC. The first attempt at surgical treatment of inguinal hernias was performed by C. Celsus (25 BC - 40 AD). He dissected the restraining ring and set the contents of the hernial sac into the abdominal cavity [3,4,9].The modern history of hernia surgery begins in the second half of the 19th century. and is associated with the name of E. Bassini (1844-1924), who created a unified concept for the treatment of hernias [1,7]. The success of hernia treatment consisted in the surgical restoration of the normal relationship of the anatomical structures in the area of the hernial protrusion. This was a revolutionary step not only in herniology, but also in the development of surgery in general. According to E. Bassini, the disadvantage of the proposed methods is that when the tissues are sutured, they are stretched and this contributes to the eruption of the sutures, which subsequently causes a recurrence of the hernia [10].In modern surgical practice, the issues of choosing the method of hernia repair in women of reproductive age are not particularly discussed. Pregnancy is a contraindication according to the recommendations of allomaterial manufacturers and their instructions. to their application. However, questions of the possibility of using allomaterials in women of childbearing age remain outside the interests of practical surgeons. We, analyzing the results of surgical treatment of this category of persons with external hernias, found that the frequency of complications in the early and late postoperative periods exceeds 20% [2,11]. A critical analysis of the clinical results of the traditional approach to the method of hernia repair has made it possible to outline ways to resolve this problem. Considering the foregoing, we conducted experimental studies, as a result of which we came to the conclusion that when localizing a hernia along the midline and under the xiphoid process, it is advisable to use the most absorbable prosid allomaterial, when localizing hernias in the lateral region of the abdomen and in the inguinal region, the most optimal is the use of semi-absorbable material ultrapro. The non-absorbable allomaterial in the form of prolene, which is widely used in modern surgery, is inappropriate for use in women of reproductive age.Considering the foregoing, the aim of this study was to improve the results of surgical treatment of women of childbearing age with hernias of the anterior abdominal wall by substantiating a differentiated approach to the choice of the method of allohernioplasty.
2. Material and Methods
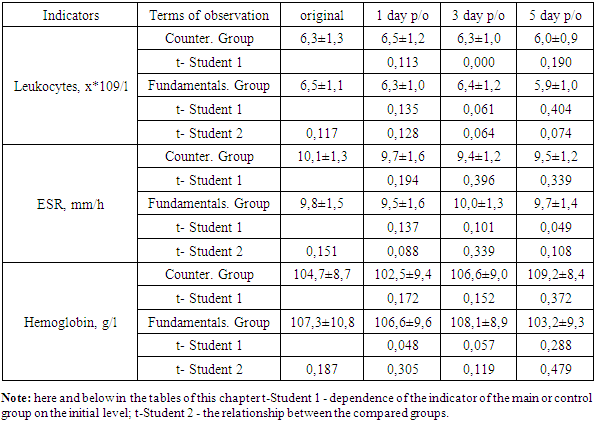
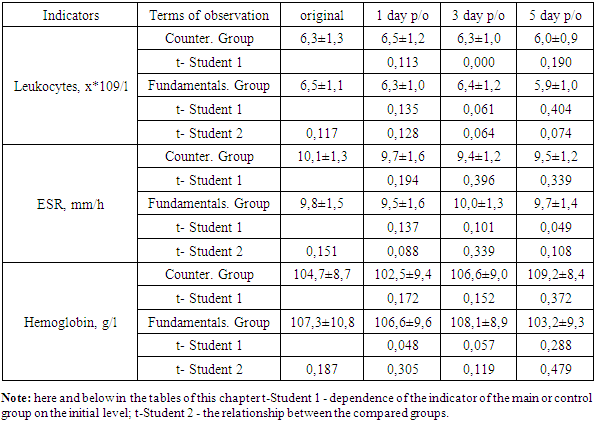
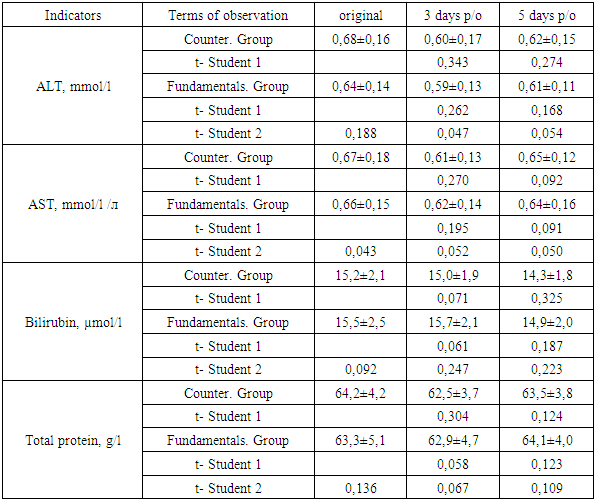
The results of surgical treatment of 64 women of childbearing age with hernias of the anterior abdominal wall, who were hospitalized for the period from 2017 to 2020, were analyzed. Of these, 35 patients were in the 1st surgical department of the Bukhara Regional Multidisciplinary Medical Center and 29 in the Department of Thoracoabdominal Surgery of the Multidisciplinary Clinic of the Tashkent Medical Academy. In a comparative aspect, the results of treatment with patients in the control group were carried out.The initial state of women in the compared groups did not differ. The clinical picture of the disease in all patients was characterized by the presence of a hernial protrusion, in 10 (15.6%) patients various dyspeptic phenomena were observed. The general condition in all cases was assessed as satisfactory, the body temperature did not exceed normal values, no hemodynamic and respiratory changes were noted. When assessing the local status, all women had a positive symptom of "cough push". The size of the hernia orifice, as in the control group, ranged from 2 to 10 cm. The average size of the hernial orifice was 4.2±1.4 cm and did not differ much from those in the comparison group (4.5±1.7 cm; t=0.136). In 61 (95.3%) patients, the hernia was single-chamber, in 3 (4.7%) patients with postoperative hernias, there were two chambers. Similar data were in the control group.Mean laboratory tests were within normal limits. The blood leukocyte counts ranged from 4.9 to 10.9*109/l (mean 6.5±1.1*109/l); ESR - from 5.0 to 12.5 mm/h (9.8±1.5 mm/h); hemoglobin - from 91 to 124 g / l (107.3 ± 10.8 g / l). In biochemical blood tests, ALT values ranged from 0.41 to 0.87 µmol/l (0.64±0.14 µmol/l), AST - from 0.43 to 0.88 µmol/l (0.66 ±0.15 µmol/l), bilirubin - from 12.1 to 20.3 mmol/l (15.5±2.5 mmol/l), total protein - from 56.6 to 72.7 g/l (63.3±5.1 g/l). In a comparative aspect, no significant differences between the main and control groups were noted for any indicator (Table 1).Table 1. Comparative evaluation of laboratory parameters in clinical groups
 |
| |
|
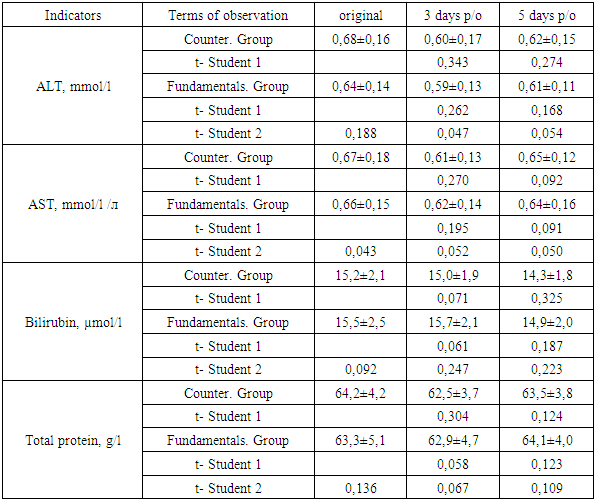
As in the control group, all patients were operated on in a planned manner. Out of 41 (64.1%) patients with inguinal hernias, in 24 (37.5%) cases, laparoscopic hernioplasty was performed (17 - transabdominal preperitoneal plasty; 7 - total extraperitoneal plasty) using ultrapro material, and in 4 (6.3 %) of which this operation was performed on both sides. In 17 (26.6%) cases, the Liechtenstein operation was performed. Moreover, the choice of the method of operation did not depend on the type of inguinal hernia. Out of 12 (18.8%) women with umbilical hernias, in 10 (15.6%) cases, hernia repair was performed with on-lay plasty using prosid. In 2 (3.2%) cases of umbilical hernia, laparoscopic hernioplasty was performed with the installation of a mesh allograft in the preperitoneal space. 5 (7.8%) patients with hernias of the white line of the abdomen underwent on-lay alloplasty of the hernia orifices using prosid. In 6 (9.4%) cases, patients with incisional hernias underwent hernia repair with on-lay alloplasty. Moreover, in 4 (6.3%) cases with the localization of the hernia along the midline, prosid was used as the allomaterial, in 2 (3.1%) cases with a hernia of the lateral region of the abdomen - ultrapro. In 2 (3.1%) cases, when performing laparoscopic hernioplasty for an inguinal hernia, laparoscopic cholecystectomy was simultaneously performed. In 2 (3.1%) cases, laparoscopic cystectomy was performed for an ovarian cyst during laparoscopic hernioplasty for an inguinal hernia in one woman and the second patient with an on-lay hernia repair for an umbilical hernia. In 3 (4.7%) cases, unilateral phlebectomy was simultaneously performed (one observation each during laparoscopic hernioplasty for an inguinal hernia; during alloplasty of the on lay type for an umbilical hernia; during alloplasty of the on lay type for a hernia of the white line of the abdomen).In the postoperative period, as well as in the control group, the parameters of the general blood test did not undergo any special changes, during the observation period there were no significant differences from the initial value. Comparative evaluation between clinical groups also did not reveal statistically significant differences (table 1).Similar dynamics was observed with the indicator of biochemical blood tests. Both individual and average indicators in the compared clinical groups were within normal limits and did not undergo any special changes in the dynamics of treatment. No significant differences were noted either in the dynamics of observations or between the compared groups (table 2).Table 2. Comparative evaluation of biochemical parameters in clinical groups
 |
| |
|
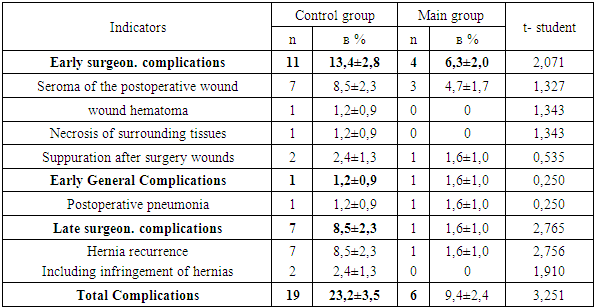
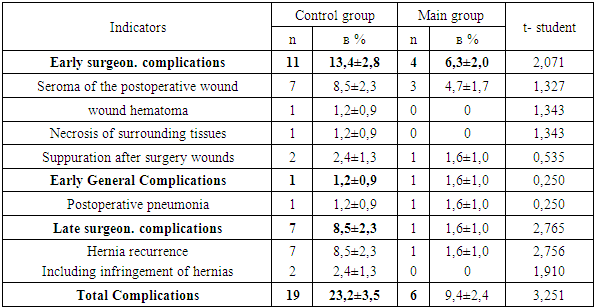
The length of stay of patients in the hospital ranged from 2 to 8 days. This indicator was lower than in the control group. The average duration of the hospital stage of treatment was 4.0±0.8 days. The decrease in bed days was associated with the inclusion of laparoscopic operations in the arsenal of surgical interventions. Despite this, there was no significant difference between the compared groups (in the control group, the average duration of inpatient treatment was 4.2±1.9 days; t=0.582).In the early postoperative period, in 6.3±2.0% (4 patients) of cases, the development of surgical complications was noted, while in the control group this figure was significantly higher (13.4±2.8%; t=2.071). In 3 (4.7%) patients, the development of seroma of the postoperative wound was noted. In all cases, conservative therapy was carried out in stationary conditions. After discharge from the hospital, these patients were treated at the outpatient stage for 4 to 11 days. In 1 (1.6%) case, after alloplasty for postoperative hernia, limited subcutaneous suppuration of the postoperative wound was noted. Conservative therapy with daily ointment dressings contributed to wound cleansing and wound healing by secondary intention.The frequency of early general complications was 1.6±1.0%, which did not differ much from those in the control group (1.2±0.9%; t=0.250). One (1.6%) patient developed pneumonia after surgery for ventral hernia. Against the background of conservative therapy, the patient's condition improved and on the 8th day she was discharged for outpatient treatment (table 3).Table 3. Clinical results in compared groups
 |
| |
|
In the remote period up to 3 years, all patients became pregnant, which ended in childbirth. Of the total number of patients, in 9 (14.1±2.9%) cases, it was necessary to resort to caesarean section, but this indicator in the main group was significantly lower than in the control group (25.6±3.6%; t=2.500 ). Only in 1 (1.6%) case, 1.5 years after alloplasty for a hernia of the white line of the abdomen, a postoperative hernia developed, which required surgical treatment in a planned manner. It should be noted that in this clinical case, a paraprosthetic hernia developed. In general, the overall frequency of complications in the main group significantly decreased from 23.2±3.5% to 9.4±2.4% (t=3.251).Clinical example. Patient U., 31 years old (IB No. 4108), was admitted to the clinic on February 14, 2017 with complaints of a hernial protrusion and discomfort in the navel. From the anamnesis considers himself ill for 3 years. The disease is associated with a pregnancy. The patient came to our clinic and was hospitalized in the thoracoabdominal surgical department of the multidisciplinary TMA clinic. When collecting an anamnesis, the patient noted that she was planning a pregnancy. Taking into account this fact, it was planned to perform an operation with alloplasty using the most absorbable prosid allomaterial.Objectively: the general condition of the patient at admission is satisfactory, consciousness is clear. Skin and visible mucous membranes of normal color. Vesicular breathing in the lungs. Heart sounds are clear, rhythmic. BP 110/70 mmHg Art. Pulse 80 beats / min. Locally: Tongue moist, clean. The abdomen is soft, participates in the act of breathing. In the umbilical region there is a hernial protrusion measuring 2.0 x 2.0 cm, retractable into the abdominal cavity (fig. 1). The symptom of "cough shock" is positive. Symptoms of peritoneal irritation are negative. Intestinal peristalsis is auscultated. Stool and diuresis regular. | Figure 1. General view of the umbilical hernia |
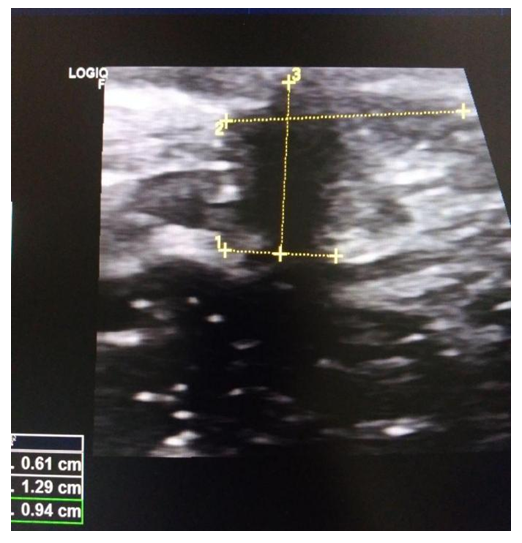
In blood tests: Complete blood count: hemoglobin - 114 g / l, erythrocytes - 4.3 x 1012 / l, color index - 0.9, platelets - 233 x 109 / l, leukocytes - 6.8 x 109 / l, ESR – 9 mm/hour. Biochemical blood tests: ALT - 0.4 mmol / l, AST - 0.5 mmol / l, bilirubin - 19.0 μmol / l, urea - 7.1 mmol / l, creatinine - 68 μmol / l, total protein - 65 g/l, fibrinogen - 220 mg%.On ultrasound: in the umbilical region, there is an expansion of the umbilical ring and the presence of a hernia. During the Valsalva test, prolapse of a part of the greater omentum is noted (fig. 2.).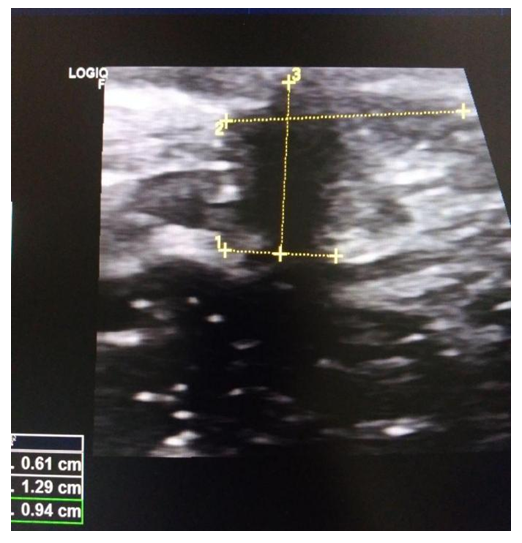 | Figure 2. Ultrasound for umbilical hernia |
The patient was diagnosed with umbilical hernia.On February 15, 2017, the patient underwent "Laparoscopic hernioplasty" under general intubation anesthesia. The contents of the hernial sac was part of the greater omentum. Intraoperatively, a preperitoneal installation of prosid allomaterial 10x10 cm in size was performed.The postoperative period proceeded smoothly. The patient was discharged on the 2nd day after surgery. She was on an outpatient basis for 5 days, the sutures were removed on the 7th day after the operation. Postoperative wound healing by primary intention.The patient became pregnant 14 months after the operation. The pregnancy proceeded uneventfully. Was under the supervision of surgeons and obstetricians. In due time, the patient had a physiological birth. The patient was examined 2.5 years after delivery. No hernia recurrence was noted.The above clinical example clearly demonstrates the advantages and possibilities of alloplasty and modern methods of surgical treatment of surgical patients. A scientifically based approach to the choice of surgical intervention, namely laparoscopic hernioplasty and the corresponding allomaterial, made it possible to achieve not only a good clinical result, but also a cosmetic effect, which is an important social factor that has a significant impact on the quality of life of people.Thus, our studies show all the advantages of our proposed approach to the choice of the method of allohernioplasty in women of childbearing age. An important fact is the widespread introduction of laparoscopic technology, which, along with numerous advantages compared to open operations, which are expressed in the reduction of postoperative pain, low incidence of wound complications, less likelihood of developing postoperative intestinal obstruction, reduced hospital stay and earlier return to baseline functions, allows for excellent visualization, wide coverage of the area outside the defect with the alloprosthesis and reliable attachment to the healthy abdominal wall fascia.Currently, there are no clear recommendations on the choice of the type of alloprosthesis for repair of hernias of the anterior abdominal wall. These questions remain debatable and open for women of childbearing age, and even more so during pregnancy. In our experience, we use composite mesh as described above for all hernias of the anterior abdominal wall. Of course, at present there are no specific studies to determine the individual histocompatibility of alloprostheses, however, this issue remains the subject of future research.
References
| [1] | Steensel S., Hil L., Bloemen A. Prevention of incisional hernia using different suture materials for closing the abdominal wall: a comparison of PDS, Vicryl and Prolene in a rat model // Hernia. – 2020. – Vol. 24, № 1. – P. 67-78. |
| [2] | Khansa I., Jefferson R., Khansa L., Janis J. E. Optimal Pain Control in Abdominal Wall Reconstruction // Plast. Reconstr. Surg. – 2018. – Vol. 142, № 3 Suppl. – P. 142–148. |
| [3] | Khamdamova M.T., Rabiev S.N. Somatometric characteristics of pregnant women with different body types // Europe's Journal of Psychology (EJOP), 2021, Vol. 17(3), Р. 215-220. |
| [4] | Kockerling F. What Do We Know About the Chevrel Technique in Ventral Incisional Hernia Repair? // Front. Surg. – 2019. – № 6. – P. 15. |
| [5] | Khamdamova M. T. Аgeechographic characteristics of the uterus and ovaries in women of the first and second period of middle age // Biology and integrative medicine. ISSN 2181-8827 2020. №2 –March- April (42). -Р. 75-86. |
| [6] | Kohler A., Lavanchy J.L., Lenoir U. Effectiveness of Prophylactic Intraperitoneal Mesh Implantation for Prevention of Incisional Hernia in Patients Undergoing Open Abdominal Surgery: A Randomized Clinical Trial // JAMA Surg. – 2019. – Vol. 154, № 2. – P. 109-115. |
| [7] | Khamdamova M. T. Age and individual variability of the shape and size of the uterus according to morphological and ultrasound studies // Problems of biology and medicine. – 2020. – №. 1. – С. 116. |
| [8] | Koscienly A., Widenmayer S., May T. Comparison of biological and alloplastic meshes in ventral incisional hernia repair // Langenbecks Arch. Surg. – 2018. – Bd. 403, № 2. – P. 255–263. |
| [9] | Khamdamova M. T., Tukhtasinovna K. M. Echographic features variability in the size and shape of the uterus and ovaries in women of the second period of adulthood using various contraceptives // Asian Journal of Multidimensional Research (AJMR). – 2020. – Т. 9. – №. 5. – С. 259-263. |
| [10] | Walming S., Angenete E., Block M. Retrospective review of risk factors for surgical wound dehiscence and incisional hernia // BMC Surg. – 2017. – Vol. 17, № 1. – P. 19. |
| [11] | Khamdamova M. T. Еchographic features of the range of variability in the size of the uterus and ovaries in women of menopausal age using oral and injectable forms of contraception // American Journal of Medicine and Medical Sciences. - 2020. - N10 (8). - P. 580-583. |
| [12] | Jucker B.E., Simillis C., Tekkis P., Kontovounisios C. Suture choice to reduce occurrence of surgical site infection, hernia, wound dehiscence and sinus/fistula: a network meta-analysis // Ann R Coll Surg Engl. – 2019. – Vol. 101, № 3. – P. 150-161. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML