-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(5): 579-583
doi:10.5923/j.ajmms.20221205.26
Received: April 23, 2022; Accepted: May 10, 2022; Published: May 24, 2022

Evaluation of the Microbial Flora of the Genital Tract and the Morphofunctional State of the Endometrium in Antiphospholipid Syndrome
Gulnoza Akhmadzhonova, Gulnoza Turaeva
Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Gulnoza Akhmadzhonova, Andijan State Medical Institute, Andijan, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Currently, the available literature data indicate that the formation of obstetric and perinatal pathology largely depends on the presence of an infectious process in the mother. Since the main trigger mechanism in the development of inflammation is microbial invasion, we conducted a study of the bacteriological contamination of the genital tract and endometrium in women with antiphospholipid syndrome (AFS).
Keywords: Antiphospholipid syndrome, Obstetric and perinatal pathology
Cite this paper: Gulnoza Akhmadzhonova, Gulnoza Turaeva, Evaluation of the Microbial Flora of the Genital Tract and the Morphofunctional State of the Endometrium in Antiphospholipid Syndrome, American Journal of Medicine and Medical Sciences, Vol. 12 No. 5, 2022, pp. 579-583. doi: 10.5923/j.ajmms.20221205.26.
Article Outline
- According to the World Health Organization (WHO), an increased rate of loss of desired pregnancies determines not only the medical but also the social significance of the problem of miscarriage. One of the main problems of obstetrics is miscarriage, the frequency of which is 10-25%, remaining high to this day. According to a number of authors, among the multiple causes of miscarriage, about 55-62% is defects in coagulation proteins or platelets, one of the manifestations of which is antiphospholipid syndrome (APS).To improve the effectiveness of measures for the early diagnosis, treatment and prevention of APS complications, a wide range of scientific research is being carried out in the world, therefore, in our country, the optimal schemes for screening activities are being improved, the optimal tactics of the screening approach are being selected, and a system is being developed to prevent the risk of reproductive complications among women. reproductive age in women with APS.There are no definite data on the frequency of APS in women in our region in the general population. This is due to difficulties in diagnosis and inconsistency between clinical and laboratory data. But, despite this alignment, most studies have shown that APA circulation is observed in 2-4% of healthy pregnant women, as well as in healthy non-pregnant women [1,6]. The fact that habitual miscarriage, a characteristic sign of APS, occurs exclusively in women, suggests that APA are found 2-5 times more often than in men [2,5].Currently, the available literature data indicate that the formation of obstetric and perinatal pathology largely depends on the presence of an infectious process in the mother [1-3]. Since the main trigger in the development of inflammation is microbial invasion, we conducted a study of bacteriological contamination of the genital tract and endometrium in women with antiphospholipid syndrome (APS) [4,5] in order to study the interaction between the pathogenesis of APS and the inflammatory process.
1. Purpose of the Study
- Assessment of the microbial flora of the genital tract and the morphological and functional state of the endometrium in women with antiphospholipid syndrome (APS) in order to study the interaction between the pathogenesis of APS and the inflammatory process.
2. Material and Methods of Research
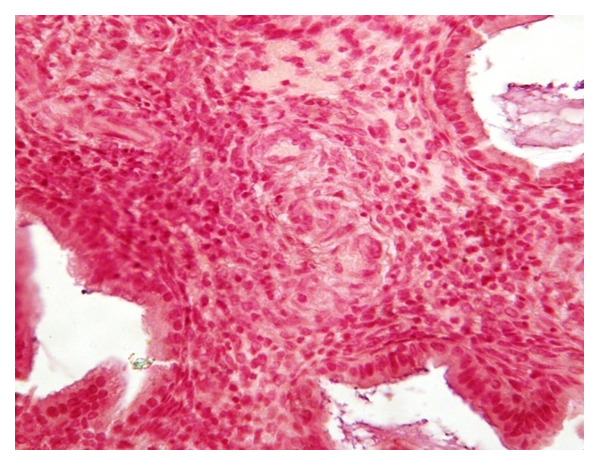
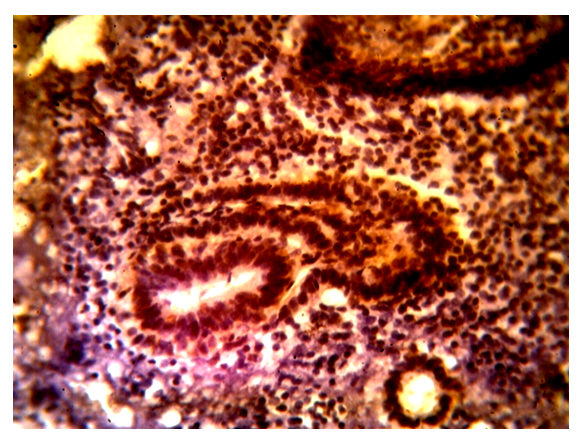
- To assess the condition of women, we studied the somatic and reproductive anamnesis, heredity, the nature of the diseases suffered, the formation of menstrual and generative functions of women, including the outcomes of pregnancies (childbirth, spontaneous abortions, ectopic pregnancy). The complex of laboratory tests included: detailed general analysis of blood, urine, determination of blood type and Rh factor, HIV, RW, carrier of the Australian antigen, biochemical blood analysis with determination of urea, bilirubin and blood content, blood coagulation system, blood test for STIs. In addition, infection screening was performed for all patients: bacteriological and bacterioscopic examination of smears from 3 points.Bacterioscopic examination of the vaginal discharge, cervical canal and scraping of the uterine mucosa. Evaluation of the microbial flora of the vagina, cervical canal and uterine cavity was carried out by bacterioscopic, bacteriological methods and polymerase chain reaction (PCR). In the bacteriological laboratory of the clinic, a survey was conducted on the microbial landscape from the cervical canal in all women, pregnant women and maternity patients with the determination of sensitivity to antibacterial and antifungal drugs. The diagnosis of vaginal candidiasis was made based on the results of microscopic and cultural examination of pathological material taken from the cervical canal. The etiological factor was considered to be the material isolated only in the III and IV degrees of massiveness. Preparations for microscopy were stained using the Gram method. Sowing was carried out on elective media, including Sabur medium to identify fungi of the genus Candida. The test material was incubated in a thermostat for 48 hours at a temperature of 22°C.Morphological and morphometric examination of the placenta. Pathomorphological examination of the placenta and histological examination of endometrial scraping were performed in the Department of Pathological anatomy of the ASMI clinic.Placenta examination was carried out according to a standardized scheme modified by A. P. Milovanov [11]. The study of the placenta began immediately from the moment of birth of the placenta, when the weight and size of the placenta, the length of the umbilical cord were determined. Attention was paid to the features of the maternal and fetal surface, the nature of the tissue on the incision, the severity of the vascular network, the location of the veins and arteries of the umbilical cord, the presence or absence of various inclusions. The mass of the placenta was determined after preliminary removal of the fruit shells and umbilical cord with scissors.For histological examination of the placenta, immediately after the birth of the placenta, pieces of placental tissue measuring lxlxl cm were taken from three zones: central, paracentral and marginal. After fixation of placental tissue in 4% neutral formalin on a phosphate buffer (pH 7.2-7.4), the material was poured into paraffin according to the Lloyd 3 method. et al. (1982). Then serial sections were made, which were stained with hematoxylin and eosin, picrofuxin according to Van Gieson.Ultrasound, Doppler examination of the examined women, cardiotocography of uterine activity and fetal cardiac activity were performed in the Department of pathology of pregnant women of the 2nd maternity complex of Andijan. Determination of hormones of the fetoplacental complex, as well as immunological studies were carried out at the Central Research Institute of ASMI (head of the laboratory of Prof. Aleynik V. A.). Polymerase chain reaction to determine the presence of STIs was carried out at the GEN-MED Medical Center in Andijan (Head of the laboratory of Ph.D. Parpieva D. A.). The morphological part of the work was carried out in the Department of Pathological anatomy of the ASMI clinic (head of the department of Assoc. Ablazimova T. B.)
3. Discussion of the Results
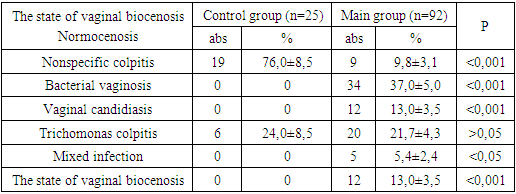
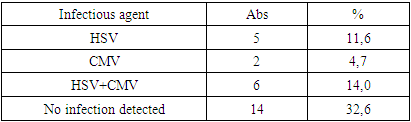
- A bacteriological study of the microbial flora of the vagina was conducted in 92 women with AFS and 25 practically healthy women. Evaluation of the microbial flora of the vagina, cervical canal and uterine cavity was carried out by bacterioscopic, bacteriological methods and polymerase chain reaction (PCR). In the control group, vaginal normocenosis was detected in 19 (76.0%) women, in the remaining 6 (24.0%), signs of candidal vaginitis without clinical manifestations of this disease were detected with bacteriological smear cultures. This can be regarded as candidiasis, which, apparently, was associated with the previously performed antimycotic treatment in 4 women and self-medication (clotrimazole) in 2 patients from this group. In the main group, during bacteriological culture of smears of the II st. vaginal purity was found in only 9 (9.8%) patients.Among inflammatory diseases of the lower genitals, the highest frequency belonged to nonspecific vaginitis, which occurred in every third woman of the main group (37.0%).Vulvovaginal candidiasis was detected in almost every fourth woman (21.7%) of the same group. Bacterial vaginosis was diagnosed somewhat less frequently (13.0%), trichomonas colpitis in 5.4% of cases in patients of the main group. Mixed infection was detected in the genital tract in women of the main group in 13.0% of cases.To determine the degree of endometrial contamination, a PCR study of scraping from the uterine cavity was performed, which was taken from 43 maternity patients of the main group (Table 2).
|
|
4. Conclusions
- Studies have shown that despite the presence of infection in women with APS, infectious agents are not pathogenetic in the complicated course of APS, which could lead to increased production of antiphospholipid antibodies. But APS itself may well be the cause of increased viral contamination, which could subsequently cause impairments in the ability of trophoblast initiation into the endometrium during pregnancy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML