-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(5): 538-540
doi:10.5923/j.ajmms.20221205.17
Received: April 13, 2022; Accepted: May 12, 2022; Published: May 14, 2022

The Role of Nephrine as a Marker of Kidney Damage in COVID-19 in Combination with Arterial Hypertension
Amonov Mukhammad Komil Ogli
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Amonov Mukhammad Komil Ogli, Bukhara State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

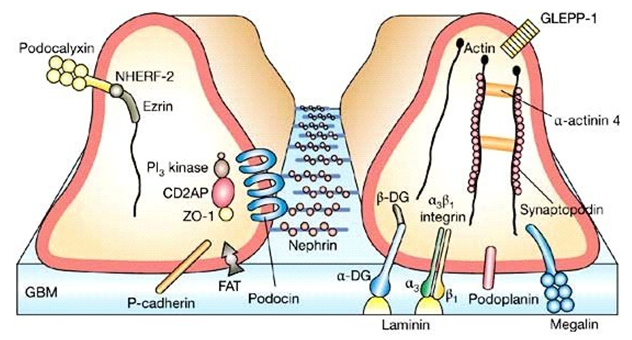
Nephrin is a podocyte-specific transmembrane protein that is predominantly localized in the slit diaphragm of the glomeruli of podocytes. Podocytes are glomerular epithelial cells located in the outermost layer of the glomerular basement membrane (GBM) and their peduncles form tight interdigital networks and regulate the filtration of circulating plasma proteins from the capillary lumen into Bowman's space. Thus, podocytes, together with BMC, determine the permeability of plasma proteins, and podocytopathies lead to proteinuria and an increase in the number of podocytes in the urine (podocyturia). An increase in podocyturia has been confirmed in patients with COVID-19. The concentration of nephrin in the urine during the period of COVID-19 disease has not been tested, the behavior of urinary nephrin during the disease has not been studied enough. The present study was performed to determine changes in nephrinuria in normotensive COVID-19 patients.
Keywords: Nephrine, Kidneys, COVID-19, Proteinuria, Creatinine
Cite this paper: Amonov Mukhammad Komil Ogli, The Role of Nephrine as a Marker of Kidney Damage in COVID-19 in Combination with Arterial Hypertension, American Journal of Medicine and Medical Sciences, Vol. 12 No. 5, 2022, pp. 538-540. doi: 10.5923/j.ajmms.20221205.17.
1. Materials and Methods
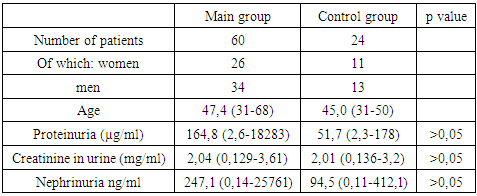
- In total, the study involved 84 patients with COVID-19 in the age range of 30-60 years, who were treated for the disease in the Bukhara Regional Infectious Diseases Hospital from November 2020 to March 2021. The patients were divided into two groups - the main group consisted of 60 patients with COVID-19 with a confirmed diagnosis of hypertension (AH) stages I-II, the control group included 24 patients with COVID-19 with normotension.This study was conducted in accordance with the principles of the Declaration of Helsinki, at the Bukhara Regional Infectious Diseases Hospital, which treats patients with COVID-19.Clinically significant proteinuria was defined as a protein/creatinine ratio (BCR, mg/mg) >0.27 (corresponding to 30 mg/mmol) in single urine samples. All single urine samples were coded and processed within 2 hours of collection. Urine samples were transferred into test tubes and centrifuged for 5 min. The urine supernatant was stored at -20°C. until protein, creatinine and nephrine levels were measured. Urinary protein and nephrin concentrations were corrected for urinary creatinine concentration and expressed as protein/creatinine ratio SBR (mg/mg) and nephrin / creatinine ratio (SNR, ng/mg).
2. Results
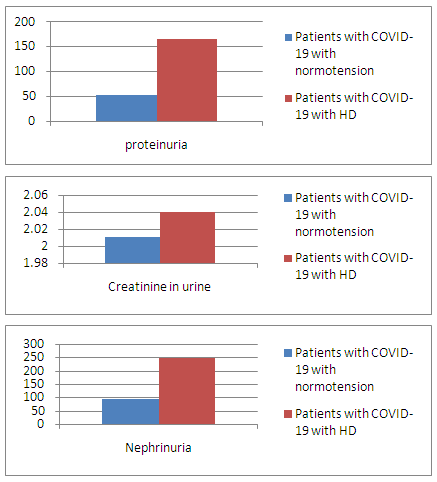
- 105 and 41 urine samples, respectively, were taken from 60 patients with COVID-19 with HD and 24 without HD. Of the 60 HD patients, 13 provided three urine samples, 19 provided two urine samples, and the remaining 28 provided only one urine sample. 17 normotensive COVID-19 patients provided two urine samples, the remaining 7 provided one sample.Proteinuria, nephrinuria and urinary creatinine in COVID-19 patients with normotensionThe concentration of nephrin in the urine is from 0.11 to 412.1 ng/ml, the concentration of protein is from 2.3 to 178 µg/ml, the concentration of creatinine is from 0.136 to 3.32 mg/ml in samples of 24 normotensive patients of the control group.Proteinuria, nephrinuria and urinary creatinine in COVID-19 patients with HDThe concentration of nephrin in the urine is from 0.14 to 25761 ng / ml, the concentration of protein is from 2.6 to 18283 μg / ml, the concentration of creatinine is from 0.129 to 3.61 mg / ml in urine samples of 60 patients of the main group.
3. Research Results
4. Findings
- Correlation of proteinuria and nephrinuria in patients of the main group and the possibility of a screening tool for predicting CKD.Proteinuria is positively correlated with nephrinuria, while urinary creatinine is inconclusive and weakly associated with kidney damage in COVID-19. At the same time, nephrinuria often occurred before the development of clinically significant proteinuria (albuminuria). This indicates that nephrin is the most sensitive indicator and the predictive value of nephrinuria as a marker of kidney damage in COVID-19 is higher.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML