Sh. I. Giyasov1, 2, A. R. Ruzibaev1, A. A. Rakhimbaev2, A. A. Kayumov2, F. R. Nasirov2, F. A. Akilov1, 2, I. B. Ziyaev2
1Tashkent Medical Academy, Tashkent, Uzbekistan
2Republican Specialized Scientific-Practical Medical Center of Urology, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Aim of the study was to evaluate the effectiveness of the preventive measures taken to reduce the frequency and severity of intra- and postoperative complications and determinate other causative factors in the development of acute complicated pyelonephritis after treatment of urolithiasis by endoscopic surgery. Introduction. Despite to the improvement of endoscopic instruments and intervention techniques, compliance with preventive measures of intra-and postoperative complications, the problem of the management of complicated urinary tract infections after interventions still remains as a very urgent problem. Materials and methods. A prospective analysis of the results of 220 X-ray endoscopic operations performed for kidney and upper urinary tract stones in the Republican Specialized Scientific-Practical Medical Center of Urology (RSSPMCU, Tashkent, Uzbekistan) during the period of 2019-2020 was carried out. The mean age of the patients was 44.3±14.8 (8-78 years) years. simple stones were in 112 (51%) patients, with 14.1±0.57 mm in size, complex - in 108 (49%), with 41.6±1.76 mm in size. During the examination, the initial infection of the urinary tract was found only in 194 patients (88.2%). From these, leukocyturia without bacteriuria was found in 59 (26.8%) patients, leukocyturia with bacteriuria in 135 (61.4%) patients, while only in 46 (20.9%) patients were revealed growth of microflora. Results. An analysis of the frequency of intraoperative complications showed that 23 (10.5%) had moderate bleeding during the intervention, which did not required additional interventions and blood transfusion, the «stone-free rate» (SFR) was 87.7%. The number of postoperative complications were 30 (13.6%), according to Clavien: I - 1 (0.5%), II - 19 (8.7%), IIIa - 5 (2.3%), IIIb - 3 (1.4%), IVa - 2 (0.9%), V-0. The most common complication was acute complicated pyelonephritis, which revealed in 19 (8.7%) patients. All complication was eliminated conservatively. Conclusion. Compliance with preventive measures to reduce the frequency and severity of intra- and postoperative complications led to the reducing the frequency and severity of complicated pyelonephritis from 18.6% to 8.6%. The frequency of complicated pyelonephritis depended on the initial infection of the urinary tract, as well as on the type of access to the stone and the duration of the intervention. The last two factors, in turn, depended on the complexity of the kidney stone.
Keywords:
Kidney stone, Urolithiasis, X-ray endoscopic operation, Leukocyturia
Cite this paper: Sh. I. Giyasov, A. R. Ruzibaev, A. A. Rakhimbaev, A. A. Kayumov, F. R. Nasirov, F. A. Akilov, I. B. Ziyaev, Infectious-Inflammatory Complications of Endoscopic Surgery of Urolithiasis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 5, 2022, pp. 531-537. doi: 10.5923/j.ajmms.20221205.16.
1. Introduction
The prevalence of urolithiasis depends on many factors, including geographical, climatic, ethnic, genetic and dietary factors. For this reason, prevalence of urolithiasis rates varies from 1 to 20% in different regions [1]. The incidence of urolithiasis is less than 10% in countries with a high standard of living. According to the literature, in some regions there has been an increase in indicators by more than 37% over the past 20 years [2–4]. In a number of regions of Uzbekistan, and especially in the Aral Sea region, the prevalence of this disease is endemic [5].Surgical interventions for urolithiasis in 22-28% lead to various complications and in 11% end with nephrectomy, in 3% - with mortality [6]. Given the widespread introduction of non-invasive and minimally invasive technology in the treatment of patients with urolithiasis, an important role belongs to the revealing causes of complications and development of their preventive measures.Endoscopic operations performed by transurethral and percutaneous approaches, which allow effective removal of both simple and complex stones, have become the "gold standard" for the surgical treatment of urolithiasis. Endoscopic surgical interventions are the method of choice in patients with high anesthetic risk, as well as with recurrent stone formation [7,8].Despite to the improvement of endoscopic instruments and intervention techniques, compliance with preventive measures of intra- and postoperative complications, the problem of the management of complicated urinary tract infections after interventions is still relevant [9,10]. The reason for this is that the development of postoperative complicated pyelonephritis depends not only on the presence of infection, but also on a number of factors and other previously developed complications, which in turn contribute to the development of a pathological infectious process.Particularly, iatrogenic damage of kidneys and urinary tract during intervention, massive bleeding, the size and location of stones, the category of their complexity, access to the stone and the duration of the intervention, impaired function of the drainage systems installed in the urinary tract undoubtedly are important in the development of complicated urinary tract infections. Because of this, the frequency of postoperative acute complicated pyelonephritis continues to be high and occupies a leading position among other complications. Consequently, the need to find solutions to issues related to their prevention does not lose relevance, despite of numerous studies [9-14].The aim of our study was to evaluate the effectiveness of the preventive measures taken to reduce the frequency and severity of intra- and postoperative complications and other causative factors in the development of acute complicated pyelonephritis after endoscopic surgery for urolithiasis.
2. Materials and Methods
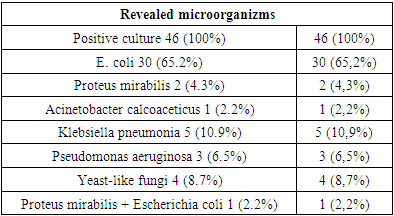
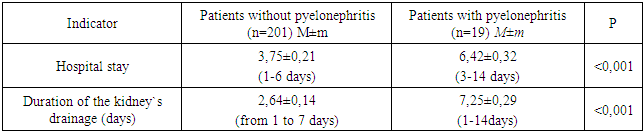
A prospective analysis of the results of 220 X-ray endoscopic operations performed for kidney and upper urinary tract stones at the Republican Specialized Scientific-Practical Medical Center of Urology (RSPMCU, Tashkent, Uzbekistan) in the period 2019-2020 was carried out. The average age of patients was 44.3±14.8 (8-78 years) years, among them 144 (65.5%) were men and 76 (34.5%) were women.111 (50.5%) stone removal interventions were performed on the right kidney, 106 (48.2%) on the left, 3 (1.3%) on both sides. In 4 (1.8%) patients, surgeries were performed on a single kidney.Stones were located in the pelvicalyceal system (PCS) in 130 (59%) patients, in both - in the PCS and in the ureter - in 19 (8.6%), only in the ureter - in 71 (32.4%) patients. The average size of stones localized in the PCS was 34.4±1.83 mm (9-87 mm), in the ureter - 12.7±0.52 mm (5-32 mm)."Simple" stones were in 112 (51%) patients, "complex" - in 108 (49%). Simple stones included single stones located in the calyx, pelvis or ureter, regardless of its size. Among patients with complex stones, two or more stones were found in 47 (21.3%) patients, staghorn stones - in 28 (12.7%), staghorn stones in combination with single or multiple stones - in 33 (15%). The average size of simple stones was 14.1±0.57 mm (5-36 mm), complex - 41.6±1.76 mm (12-105 mm).Before the intervention, the dilation of the pelvicalyceal system was in the form of calicoectasia in 55 (25%), hydronephrosis - in 41 (18.6%), ureterohydronephrosis - in 78 (35.4%). At the same time, due to complicated pyelonephritis and / or decreasing of kidney function, nephrostomy drainage was previously installed in 27 (12.3%) patients, and JJ stent was installed in 3 (1.4%) patients. Against the background of stones in 16 (7.3%) patients, there was no dilation of the PCS. Stones were removed by percutaneous access in 179 (81.4%) patients, from them in 149 (67.7%) patients was performed percutaneous nephrolithotripsy (PNL) and in 30 (13.6%) patients - percutaneous antegrade nephroureterolithotripsy (or extraction). At the same time, 161 (73.1%) patients were operated through one percutaneous access and 18 (8.1%) patients - through two accesses. Stones were removed by transurethral access in 41 (18.7%) patients, who were underwent ureterolithotripsy (or extraction). In patients with single stones predominantly was performed Holmium laser lithotripsy, for staghorn and multiple stones were performed pneumatic and ultrasonic lithotripsy, while the size of the nephroscope was 24 Ch-26 Ch, Amplatz - 30 Ch. Our analysis revealed that the body temperature during the initial visit to the clinic was normal in 205 (93.1%) patients, subfebrile - in 4 (1.9%), febrile - in 10 (4.5%), hectic - in 1 (0.5%). During the examination, the initial infection of the urinary tract was found in 194 (88.2%). Of these, leukocyturia without bacteriuria was found in 59 (26.8%), leukocyturia with bacteriuria in 135 (61.4%). All 194 patients underwent bacteriological examination of urine, while only 46 (20.9%) showed growth of microflora and 148 (67.3%) showed absence of growth of bacteria. Among identified microorganizms, the vast majority accounts for E. coli, which revealed in 30 (65.2%) cases, Table 1. Table 1. Revealed microrganizms from patient`s urine
 |
| |
|
Patients with revealed flora were treated according to the antibiogram and other patients, without growth of microorganizms - with broad-spectrum antibiotics, and due to controlled infection of the urinary tract, the main operation (removing stones) was performed.The anesthetic risk of surgical interventions was assessed according to the system for assessing the objective status of the patient, adopted by the American Society of Anesthesiologists (ASA) [15].The duration of the surgical intervention was determined from the moment of access to the stone until the final installation of drainage into the urinary tract.The criteria for postoperative pyelonephritis were the following indicators: increase of patient's body temperature to 38°C and above for 2 or more days, flank pain, changes in the patient's urine and peripheral blood characteristic of the inflammatory process.Statistical processing of the material was carried out using MS Office Excel 2007, StatSoft Statistica 8.0 using the Student-Fisher criteria.
3. Results
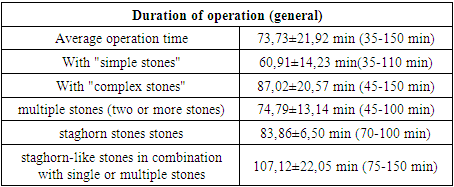
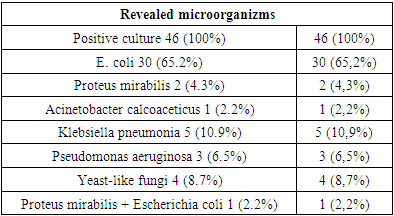
The analysis of the duration of the operation, depending on the category of complexity of the stones, showed the following results, Table 2.Table 2. Duration of operation depending on the category of complexity of stones
 |
| |
|
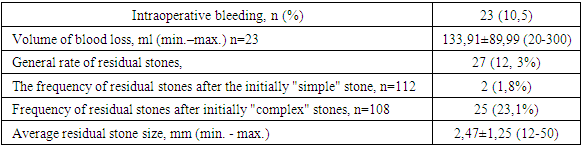
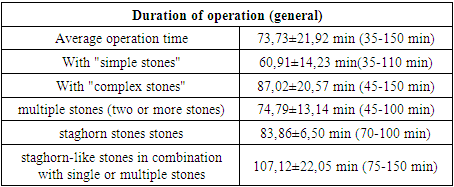
An analysis of the frequency of intraoperative complications revealed that 23 (10.5%) patients had moderate bleeding during the intervention, which did not require additional interventions and blood transfusion, the stone free rate was 87.7%. We did not find other complications, Table 3.Table 3. The frequency of intraoperative complications of endoscopic surgery for urolithiasis
 |
| |
|
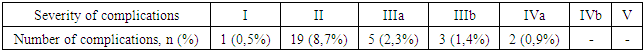
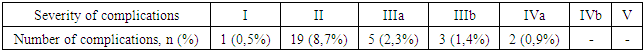
An analysis of the postoperative period showed that there were 30 cases of deviations from the standard, which were regarded as a complication and we systematized them according to the Clavien-Dindo classification [16], which we adapted in 2012 for an objective assessment of postoperative complications of endoscopic surgery for urolithiasis [17], Table 4.Table 4. Systematization of postoperative complications in endoscopic (percutaneous and transurethral) removal of upper urinary tract stones according to the adapted Clavien-Dindo classification. Number of complications 30 (13.6%)
 |
| |
|
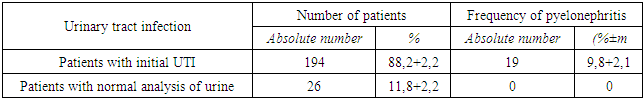
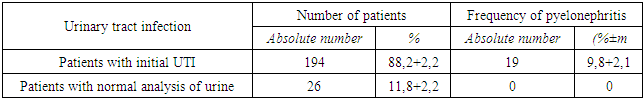
We observed a patient with one case of a small hematoma in the perirenal space without additional interventions and included him in the I degree of severity.An infectious-inflammatory complication developed in 19 (8.7%) patients in the form of acute complicated pyelonephritis, none of them developed urosepsis. In all cases, the complication was eliminated conservatively and we included them as a complication of the II degree of severity.In 3 (1.4%) patients, ureteral edema was detected in the postoperative period, from them ureteral stenting was performed in 2 patients, catheterization - in 1 with local anesthesia, all them were included in IIIa.In 3 (1.4%) patients, under general anesthesia, additional interventions were performed - renephrostomy in 2 (for a prolapsed nephrostomy in one and a non-functioning nephrostomy in another) and in 1 - nephroscopy and aspiration of blood clots were performed for tamponade PCS cavities, which we included in IIIb.Due to a life-threatening situation because of angina pectoris, 2 (0.9%) patients in the postoperative period were transferred to the intensive care ward and received drug therapy, which considered as a complication IVa.From the 27 (12.3%) residual stones, 2 (0.9%) were after an initially "simple" stone, which were eliminated by ESWL and regarded as a complication IIIa (intervention without general anesthesia). Another 25 (11.4%) residual stones after the initially “complex” stone were eliminated by repeated percutaneous intervention, and in some patients, ESWL was performed and regarded as a stage of treatment according to the accepted standard of the postoperative period [17].The most common complication of the postoperative period is still complicated pyelonephritis 19 (8.7%), which again requires an analysis of its causes and the development of preventive measures.To determine the impact of initial urinary tract infection (UTI) on the development of postoperative pyelonephritis, patients were divided into two groups, with initial UTI and without UTI. The analysis showed that even with the sanitation of the urinary tract before the intervention and perioperative preparation of patients, the initial UTI significantly affected the incidence of pyelonephritis, Table 5.Table 5. The frequency of pyelonephritis depending on the presence of initial urinary tract infection
 |
| |
|
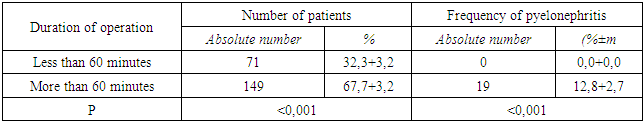
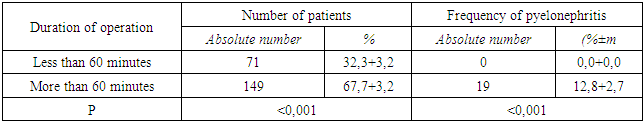
To analyze the causes of infectious and inflammatory complications, according to the duration of the operative time, the patients were divided into two groups: patients with an intervention of less than 60 minutes or more, Table 6.Table 6. The frequency of pyelonephritis depending on the duration of surgical intervention
 |
| |
|
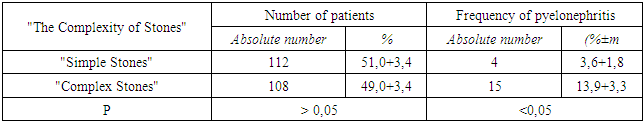
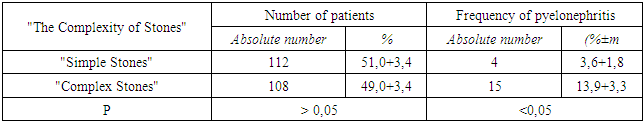
The effect of the initial complexity of stones on the frequency of pyelonephritis showed that complicated pyelonephritis developed significantly more often with complex stones, Table 7.Table 7. The incidence of pyelonephritis, depending on the initial complexity of stones
 |
| |
|
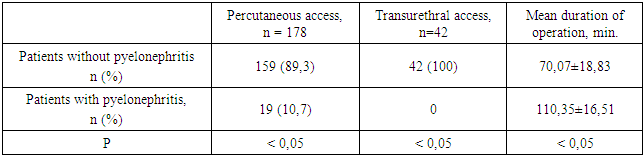
Causes of pyelonephritis, depending on the performed accesses, showed that in all 19 patients the stones were removed by percutaneous access, while in 18 patients were perfomed percutaneous nephrolithotripsy, and in 1 patient was performed percutaneous antegrade nephroureterolithotripsy, Table 8.Table 8. Comparative assessment of the type of access and duration of surgery in patients without pyelonephritis and with developed pyelonephritis
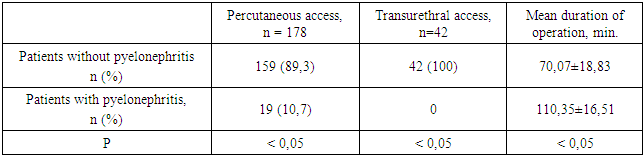 |
| |
|
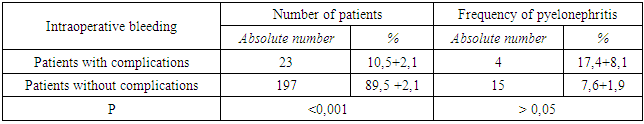
Thus, in all 19 patients, stone removal was carried out by percutaneous transrenal access. Among patients in whom the stone was removed by transurethral access in the postoperative period, none of the patients developed pyelonephritis.After that we analyzed the effect of the frequency of intraoperative bleeding and other postoperative complications on the incidence of postoperative pyelonephritis, Tables 9, 10.Table 9. The frequency of pyelonephritis depending on the presence of intraoperative complications
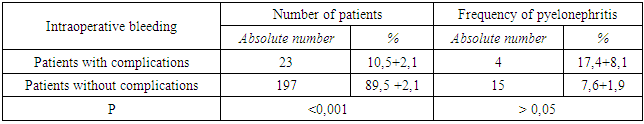 |
| |
|
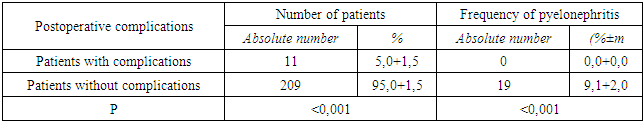
Table 10. The frequency of pyelonephritis depending on the presence of other postoperative complications
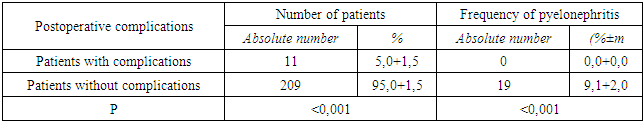 |
| |
|
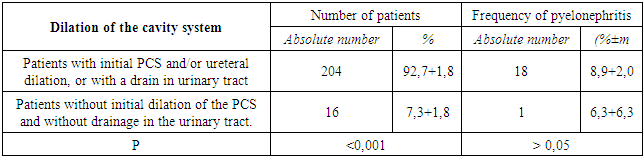
As we found out, intraoperative bleeding and other postoperative complications did not have a significant impact on the incidence of pyelonephritis.The frequency of pyelonephritis also did not differ among patients with the initial dilation of the PCS and installed drains, as well as without the dilation of the PCS, Table 11.Table 11. The frequency of pyelonephritis depending on the presence of the initial expansion of the cavities of the kidneys
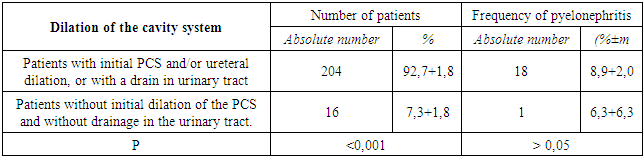 |
| |
|
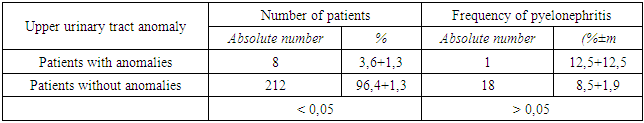
We also analyzed the impact of the presence of urinary tract anomalies on the development of pyelonephritis and the study showed no relationship, Table 12.Table 12. The incidence of pyelonephritis depending on the presence of urinary tract anomalies
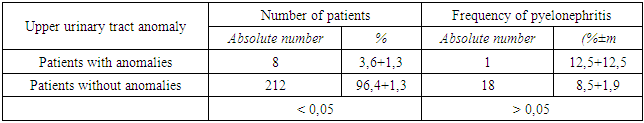 |
| |
|
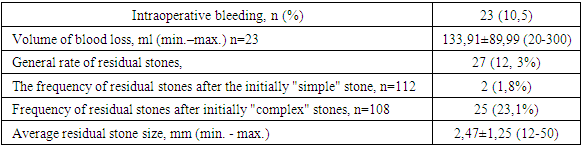
The analysis of the postoperative period showed that in patients with the development of acute pyelonephritis, the drainage in the cavities of the urinary tract was significantly longer and the hospital stay was significantly more than in patients without any complications in postoperative period, Table 13. Table 13. Duration of the patients stay in the hospital depending on the development of postoperative pyelonephritis
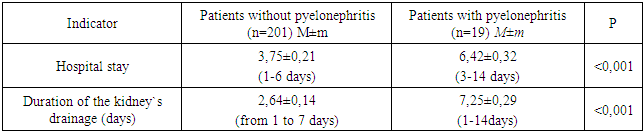 |
| |
|
Thus, among all complications, 20 (66.7%) were relatively mild - I-II severity and were eliminated conservatively. 10 (33.3%) complications were classified as grade III-IV, the elimination of which required additional invasive interventions, and in 2 patients the patients were in the intensive care unit.
4. Discussion
Despite to the constant improvement of technical characteristics and quality of equipment for endoscopic access and disintegration of stones, as well as methods of anesthesia, during performing percutaneous nephrolithotripsy, a personal approach is required from highly qualified surgeon, who must be prepared for non-standard situations [18]. Thus, according to the literature, the frequency of postoperative complications is directly dependent on the size and number of removed stones [19], on the increase in the duration of the operation [20], as well as on the number of performed percutaneous accesses [14]. In our study, we also confirmed the significance of these factors in the development of complicated urinary tract infection. At the same time, the authors most often associate the development of pyelonephritis both with the features of the intervention technology and with other predisposing factors [17,21].According to the literature, the frequency of complications after ureteroscopy accounts for about 9-25% [22-24]. At the same time, they are mild and do not require additional intervention. Ureteral avulsion and stricture are extremely rare (<1%), prior perforations are considered as the most important risk factor for complications. In our study, mild complications were also detected in the form of edema of the ureteral wall in 3 (1.4%) patients in the postoperative period, for which stenting or catheterization of the ureter was performed. No stricture or avulsion of the ureter was observed.With percutaneous access for the treatment of urolithiasis, the frequency of febrile temperature accounts for 10.8%, blood transfusions - 7%, thoracic complications in the form of damage to the pleura or lung - 1.5%, sepsis - 0.5%, damage to visceral organs - 0.4%, embolism - 0.4%, urinoma formation - 0.2% and death - 0.05% [25]. According to our study, among with percutaneous access, the rate of pyelonephritis was 10.7%, perirenal hematoma - 0,5%, 1 nephroscopy due to tamponade of the PCS with bundles - 0,5%. Our previous analysis of the causes of complicated pyelonephritis after endoscopic surgery for urolithiasis in our Center, revealed its significant relationship with the presence of an initial urinary tract infection, the frequency of developed intraoperative and various postoperative complications. From 280 patients, in 52 (18.6%) developed complicated pyelonephritis, while 3 of them (1.07%) had life-threatening sepsis. Consequently, we have developed preventive measures for the leading to the development of pyelonephritis causes in our patients, as well as a number of generally accepted preventive measures, including the implementation of standard infection control measures in the hospital, such as reducing the duration of hospitalization, early removal of indwelling urethral catheters, avoiding unnecessary catheterizations, adequate using of closed drainage systems, and daily compliance with asepsis rules to prevent cross-infection [21].As a result of the measures taken to prevent intraoperative complications, the incidence of patients with a blood loss of more than 150 ml decreased from 4.1% to 1.4%, due to which the need for blood transfusion decreased from 0.6% to 0. In the previous study If we proved the significant role of this complication in the development of postoperative pyelonephritis [26], now, due to the preventive measures taken, the frequency of intraoperative complications did not affect the development of pyelonephritis.Previously in our study, a significant role of other postoperative complications in the development of pyelonephritis was proved and the complication rate was 5.1%, from them 1.5% accounts for hematuria, 0.7% required blood transfusion, to correct 4.5% of developed complications was required additional interventions, due to late complications too [26]. Although the overall frequency of other postoperative complications have not changed (5.0%), according to the preventive measures taken, was observed relatively mild course of complications, hematuria was only in 0.4% cases and there was not blood transfusion, to correct the developed complications 2.7% cases required additional interventions only in the early postoperative period, there are no late complications. As a result, we have achieved that postoperative complications, as well as intraoperative ones, did not affect to the incidence of pyelonephritis, and also prevented the development of urosepsis, which is a life-threatening condition for the patient.In our study, we have proved that nowadays, in the cases of the implementation and compliance of preventive measures for the development of infectious and inflammatory complications, a significant role in the development of pyelonephritis belongs to the initial infection of the urinary tract, as well as the duration of the intervention, type of access and the complexity of the stone. The last three factors are interrelated, because of the access and duration of the intervention depend on the complexity of the stone.
5. Conclusions
Compliance with preventive measures to the reduce the frequency and severity of intra- and postoperative complications played an important role in the reducing of the rate frequency and severity of complicated pyelonephritis from 18.6% to 8.6%.The frequency of complicated pyelonephritis depended on the initial infection of the urinary tract, as well as on the type of access to the stone and the duration of the intervention. The last two factors, in turn, depended on the complexity of the kidney stone.
References
| [1] | Trinchieri A. et al. Epidemiology, in Stone Disease, K.S. C.P. Segura JW, Pak CY, Preminger GM, Tolley D., Editors. 2003, Health Publications: Paris. |
| [2] | Stamatelou, K.K., et al. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int, 2003. 63: 1817. https://pubmed.ncbi.nlm.nih.gov/12675858. |
| [3] | Hesse, A., et al. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur Urol, 2003. 44: 709. https://pubmed.ncbi.nlm.nih.gov/14644124. |
| [4] | Sanchez-Martin, F.M., et al. [Incidence and prevalence of published studies about urolithiasis in Spain. A review]. Actas Urol Esp, 2007. 31: 511. https://pubmed.ncbi.nlm.nih.gov/17711170. |
| [5] | Khudaybergenov U.A., Akilov F.A., Makhmudov A.T. et al. Studying of prevalence of the most significant urological diseases in the Aral Sea Area. European Science Review. 2017, 1(2): 140-144. DOI:10.20534/ESR-17-1.2-140-144. |
| [6] | Taguchi, K., Yasui, T., Milliner, D.S., Hoppe,B., Chi, T. Genetic Risk Factors for idiopathic Urolithiasis: A systematic review of the literature and causal network analysis. // European Urology Focus. https://doi.org/10:1016/j.euf.2017.04.010. |
| [7] | Skolarikos A., Alivizatos G.,de la Rosette J.J. Percutaneous Nephrolithotomy and its legasy. European Urology. 2005; 47(1): 22-28. DOI: 10.1016/j.eururo.2004.08.009. |
| [8] | Nouralizadeh A, Lashay A, Ziaee SA, Ahanian A, Sharifi SH, et al. Percutaneous nephrolithotomy in high-risk patients: a single-center experience with more than 350 cases. Urologia Internationalis. 2013. 90(4): 394-8. doi: 10.1159/000347032. |
| [9] | Dogan H.S., Guliyev F., Cetinkaya Y.S. et al. Importance of microbiological evaluation in management of infectious complications following percutaneous nephrolithotomy. Int. Urol. Nephrol. 2007. 38(3): 737-742. DOI:10.1007/s11255-006-9147-9. |
| [10] | Mariappan P., Smith G., Bariol. S.V. et al. Stone and pelvic urine culture and sensitive are better then bladder urine as predictors of urosepsis following percutaneous nephrolithotomy: a prospective clinical study. Journal of Urology (Baltimore). 2005. 173(5): 1610-1614. DOI:10.1097/01.ju.0000154350.78826.96. |
| [11] | Manuel Ritter, Patrick Krombach, Maurice S. Michel. Percutaneous Stone Removal. European Urology Supplements. 10. 2011; 433-439. |
| [12] | Xue W, Pacik D, Boellaard W, Breda A, Botoca M. et al.; CROES PCNL Study Group. Management of single large nonstaghorn renal stones in the CROES PCNL global study. Journal of Urology. 2012 Apr; 187(4): 1293-7. DOI: 10.1016/j.juro.2011.11.113. |
| [13] | Labate G, Modi P, Timoney A, Cormio L, Zhang X et al. On Behalf Of The Croes Pcnl Study Group. The percutaneous nephrolithotomy global study: classification of complications. Journal of Endourology. 2011 Aug; 25(8): 1275-80. DOI: 10.1089/end.2011.0067. |
| [14] | Kadlec A.O, Greco K.A, Fridirici Z.C, Hart S.T, Vellos T.G et al. Comparison of complication rates for unilateral and bilateral percutaneous nephrolithotomy (PCNL) using a modified Clavien grading system. BJU International. 2013 Apr; 111(4 Pt B): E243-8. DOI: 10.1111/j.1464-410X.2012.11589.x. |
| [15] | De Cassai A, Boscolo A, Tonetti T, Ban I, Ori C. Assignment of ASA-physical status relates to anesthesiologists' experience: a survey-based national-study. Korean J Anesthesiol. 2019 Feb; 72(1):53-59. |
| [16] | Dindo D., Demartines N., Clavien P.A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery. 2004; 240:205-13. DOI: 10.1097/01.sla.0000133083.54934.ae. |
| [17] | Akilov F.A., Giyasov Sh.I., Mukhtarov Sh.T., Nasirov F.R. Alidjanov J.F. Applicability of the Clavien-Dindo grading system for assessing the postoperative complications of endoscopic surgery for nephrolithiasis: a critical review. Turkish Journal of Urology. 2013. 39(3): 153-60. DOI: 10.5152/tud.2013.032. |
| [18] | Manuel Ritter, Patrick Krombach, Maurice S. Michel. Percutaneous Stone Removal European Urology Supplements. 10. 2011; 433-439. |
| [19] | Xue W, Pacik D, Boellaard W, Breda A, Botoca M. et al.; CROES PCNL Study Group. Management of single large nonstaghorn renal stones in the CROES PCNL global study. Journal of Urology. 2012 Apr; 187(4): 1293-7. DOI: 10.1016/j.juro.2011.11.113. |
| [20] | Labate G, Modi P, Timoney A, Cormio L, Zhang X et al. On Behalf Of The Croes Pcnl Study Group. The percutaneous nephrolithotomy global study: classification of complications. Journal of Endourology. 2011 Aug; 25(8): 1275-80. DOI: 10.1089/end.2011.0067. |
| [21] | Guideline EAU 2021. |
| [22] | Preminger, G.M., et al. 2007 Guideline for the management of ureteral calculi. Eur Urol, 2007. 52: 1610. https://pubmed.ncbi.nlm.nih.gov/18074433. |
| [23] | Geavlete, P., et al. Complications of 2735 retrograde semirigid ureteroscopy procedures: a single-center experience. J Endourol, 2006. 20: 179. https://pubmed.ncbi.nlm.nih.gov/16548724. |
| [24] | Perez Castro, E., et al. Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol, 2014. 66: 102. https://pubmed.ncbi.nlm.nih.gov/24507782. |
| [25] | Seitz, C., et al. Incidence, prevention, and management of complications following percutaneous nephrolitholapaxy. Eur Urol, 2012. 61: 146. https://pubmed.ncbi.nlm.nih.gov/21978422. |
| [26] | Akilov F.A., Giyasov S.I. Analysis of causes, frequency and severity of acute complicated pyelonephritis in endoscopic interventions for urolithiasis. Urology Herald. 2017; 5(4): 5-12. (In Russ.) https://doi.org/10.21886/2308-6424-2017-5-4-5-12. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML