-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(5): 512-518
doi:10.5923/j.ajmms.20221205.13
Received: April 13, 2022; Accepted: May 2, 2022; Published: May 12, 2022

Comprehensive Surgical Approach for Patients with Ventral Hernia and Morbid Obesity
Abdurakhmanov Diyor Shukurullaevich
Samarkand State Medical University, Uzbekistan
Correspondence to: Abdurakhmanov Diyor Shukurullaevich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. There is an increasing trend in the number of people with overweight and obesity in almost all developed countries at the present time. The number of patients with co-morbidities associated with obesity, including ventral hernias, is increasing. The aim of the study is to improve the quality of ventral hernia treatment in morbidly obese patients by improving the tactical and technical aspects and optimizing the choice of hernioplasty technique. Materials and methods of investigation. The study is based on clinical and laboratory examination of 121 patients with ventral hernias, who were operated on at the surgical department of the 1st clinic of Samarkand State Medical Institute during the period from 2012 to 2021. Results of the study. The use of the improved pneumobandage has significantly improved the quality of preoperative preparation of patients with ventral hernia and morbid obesity, reduced the risk of intra-abdominal hypertension after hernioplasty, improved the patient's condition earlier and reduced the incidence of postoperative extraabdominal complications from 7.4% to 4.5% accordingly. Conclusions. Application of the suggested algorithm taking into account the improved tactical and technical aspects of surgical treatment of ventral hernias in morbidly obese patients permitted to decrease significantly the total rate of postoperative complications from 15% to 9% (p=0,045), including wound complications from 11% to 5%, and also to decrease significantly the duration of surgical treatment and rehabilitation periods after various variants of hernio- and abdominoplasty.
Keywords: Postoperative ventral hernia, Complication, Compartment syndrome, Prevention
Cite this paper: Abdurakhmanov Diyor Shukurullaevich, Comprehensive Surgical Approach for Patients with Ventral Hernia and Morbid Obesity, American Journal of Medicine and Medical Sciences, Vol. 12 No. 5, 2022, pp. 512-518. doi: 10.5923/j.ajmms.20221205.13.
Article Outline
1. Introduction
- There is an increasing trend in the number of people with overweight and obesity in almost all developed countries at the current time. The number of patients with co-morbidities associated with obesity, including ventral hernias, is increasing as well. One of the causes of ventral hernias is obesity. Patients with varying degrees of obesity constitute 50 to 70% of all ventral hernia patients, with 34% having morbid obesity. Obesity is one of the major contributing factors for Hernia occurrence as well as its recurrence post surgeries, i.e. obesity as an etiologic factor in the occurrence or recurrent ventral hernia is recognized undeniably. The recurrence rate after hernioplasty is 3-13%, and with morbid obesity it reaches up to 28%.One of the significant problems of large and giant ventral hernia treatment, besides technical aspects, is an increase in intra-abdominal pressure (IAP), which leads to the development of intra-abdominal hypertension, respiratory and cardiac failure, which significantly worsens the early postoperative period, with a high mortality rate.The significant percentage of unsatisfactory outcomes and the lack of choice of the optimal method of treatment prompt further research in this field. The above dictates the necessity to develop and implement in practice optimal approaches to surgical treatment of ventral hernias in morbidly obese patients, especially in terms of the preparatory phase with an assessment of the human reserve capacity.
2. The Aim of the Study
- The aim of the study is to improve the quality of ventral hernia treatment in morbidly obese patients by improving the tactical and technical aspects and optimizing the choice of hernioplasty technique.
3. Materials and Methods of Investigation
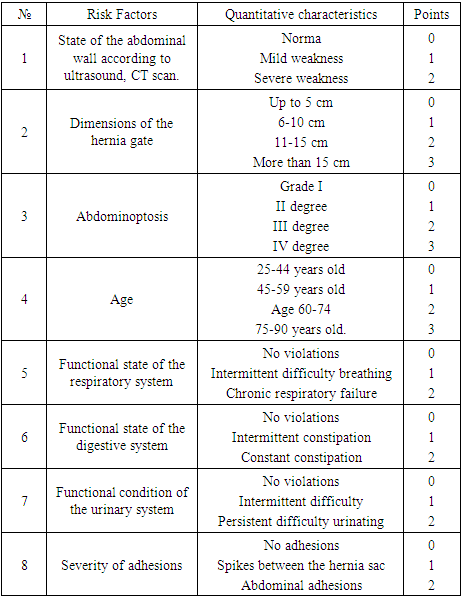
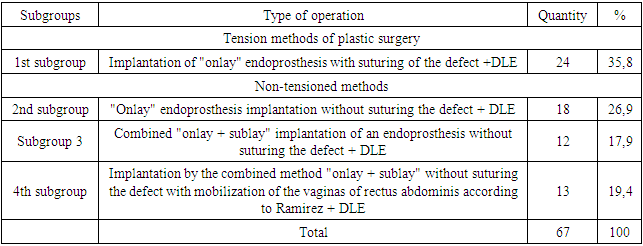
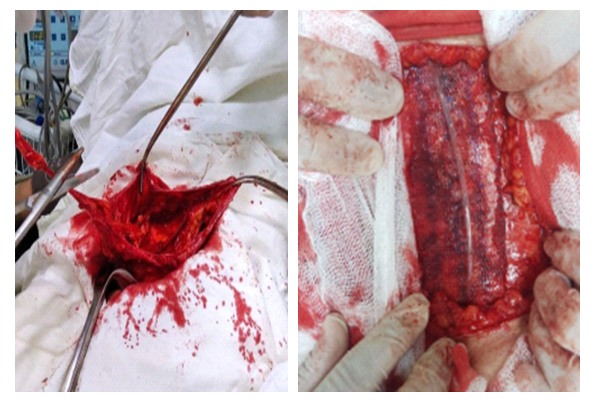
- The study is based on clinical and laboratory examination of 121 patients with ventral hernias, who were operated on at the surgical department of the 1st clinic of Samarkand State Medical Institute during the period from 2012 to 2021. All patients were operated on routinely. The patients were divided into two groups depending on the choice of treatment strategies. The first group, a comparison group, consisted of 54 patients in whom hernioplasty was performed using polypropylene prosthesis. The second group, the main group, consisted of 67 patients in whom hernioplasty was performed using a polypropylene prosthesis in combination with DLE.All patients underwent anthropometry with the detection of body weight. At the time of measurement, it was noted that patients had pathological obesity, BMI ranged from 30 to 36. - alimentary obesity caused by peculiarities of eating behavior in combination with low physical activity. Obesity was assessed according to the classification proposed by WHO. Patients were classified according to the degrees of ptosis of the anterior abdominal wall according to the classification of A. Matarasso (1989). Minimal and medium ptosis (I-II degree) was observed in 34 and 42 patients with III-IV degree obesity respectively. Moderate and severe ptosis (III-IV degree) was observed in 20 and 25 patients with III-IV degree obesity.Out of 121 patients, 90 (74.4%) patients had comorbidities. Among them 49 patients had 1 concomitant pathology, 29 patients had 2 and 12 patients had 3 concomitant diseases. Among the comorbidities there were often cardiovascular diseases in 83.4% of patients, respiratory system pathology in 22 (10.1%) patients, varicose veins of the lower extremities in 29 (13.4%) patients, and diabetes mellitus in 12 (5.5%) patients. The frequency of concomitant pathology in the study groups is presented in Fig. 2.4.Preoperative preparation for surgery was performed with the participation of cardiologist and pulmonologist. We studied the following Lung Indices by common methods: such as Stange's test, respiratory rate, respiratory volume, minute respiratory volume, vital capacity, maximal lung ventilation.In 46 (68.6%) patients of the main group with ventral hernias at the preoperative stage we performed training adaptation to increase intra-abdominal pressure using an improved pneumatic bandage belt.Before the operation, the patients underwent hygienic treatment of the anterior abdominal wall, and an area on the skin was marked. Patients in the first comparison group underwent hernioplasty with local tissues and hernioplasty with a polypropylene prosthesis (Fig. 1).
 | Figure 1. Distribution of patients in the comparison group by type of hernioplasty |
|
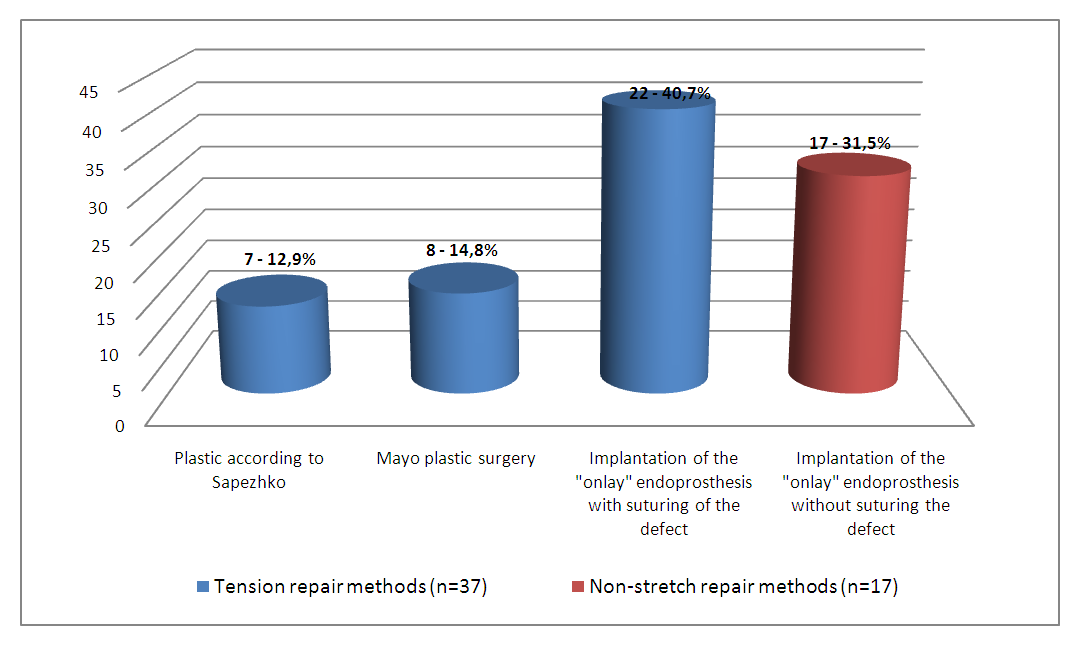
 | Figure 2. CTGA of patient P. 59 years old, No. IB 3754/296 |
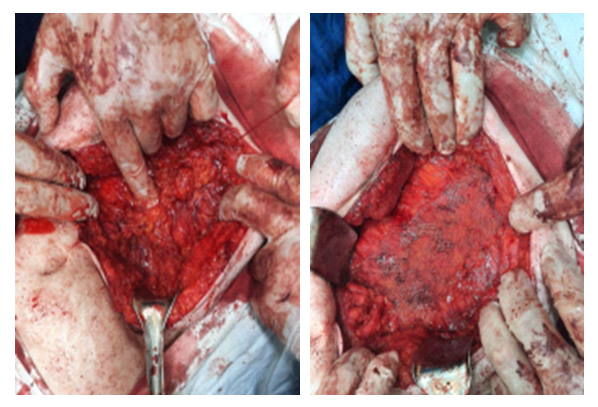 | Figure 3. Onlay implantation with suturing of the defect |
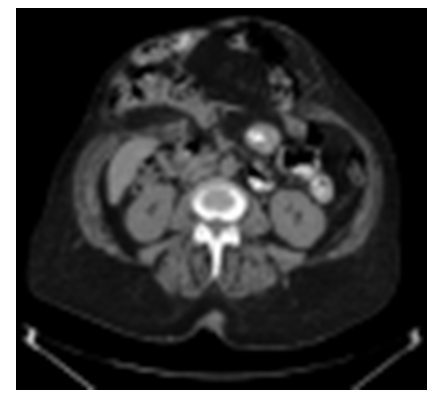
 | Figure 4. CTGA of patient R. 49 years old, No. IB 2965/268 |
 | Figure 5. Onlay implantation without suturing the defect |
|
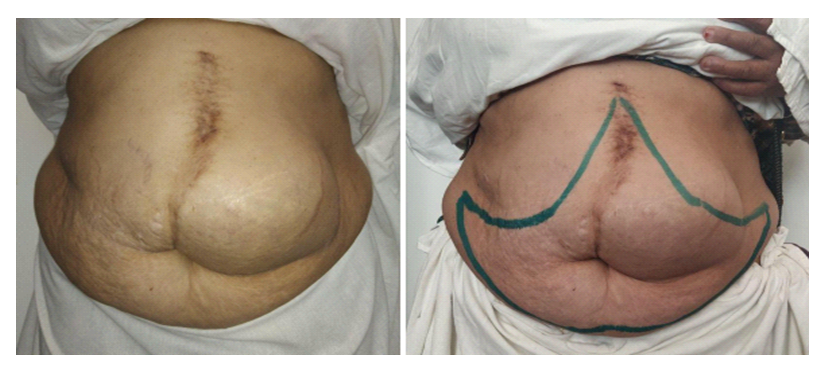 | Figure 6. Anchor-type skin marking (Castanares cut) |
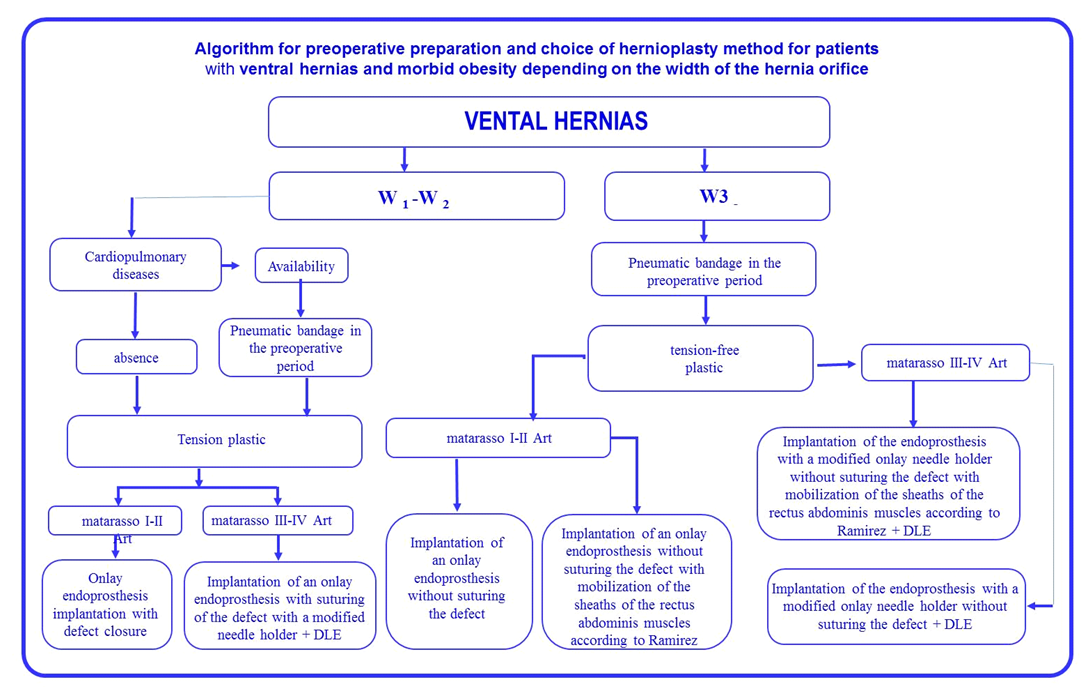 | Figure 7. Algorithm of hernialloplasty method selection |
4. Results of the Study
- Improved choice of surgical treatment tactics for ventral hernia, surgical techniques and other innovations developed and introduced in this study could not but have an impact on the immediate results of management of this category of patients. Normal gastrointestinal function was preserved in 119 (98,4%) patients after surgery, only 2 (1,6%) patients (one patient per each study group) had intestinal paresis and 1 (0,8%) patient from the comparison group had urinary retention treated with medication.Bronchopulmonary complications were noted in 3 (2.5%) cases. The development of CAD (compartment) occurred in 1 (1.8%) patient of the comparison group, the patient required prolonged EVI with breathing training, which was successfully treated conservatively. Cardiovascular complications occurred in 2 (1.6%) patients. Both respiratory and cardiovascular complications were also associated with abdominal compression due to hernioplasty of large ventral hernias. Among wound complications, postoperative hematomas were noted in 2 (3.7%) and 1 (1.2%) cases, respectively, seromas in 2 (3.7%) and 1 (1.5%) patients, lymphoria in 3 (2.5%) patients, in 2 and 1 cases in comparison and main groups respectively, wound suppuration in 1 (1.8%) patient in comparison group and skin flap edge necrosis in 2 (3.7%) and 1 (1.5%) cases.It should be noted that, on average, there were 2-3 complications per patient in the comparison group in the form of a combination of bronchopulmonary and/or cardiovascular complications with wound complications. Overall, there were 8 (14.8% of 54) patients in the comparison group with different complications, of which 6 (11.1%) had wound complications and 4 (7.4%) had general extra-abdominal complications (Fig. 8).
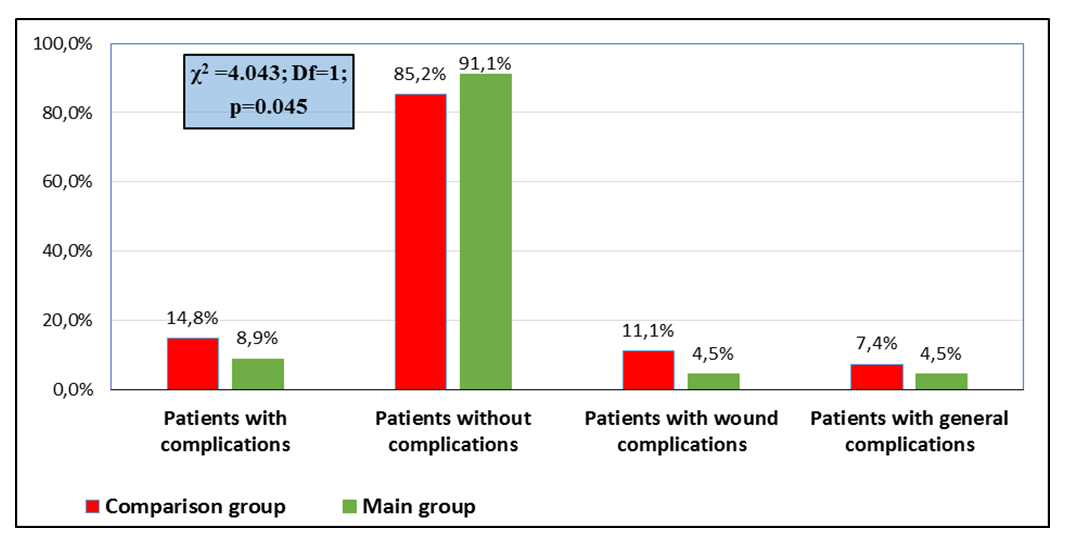 | Figure 8. Distribution of patients according to the frequency of complications after hernioplasty |
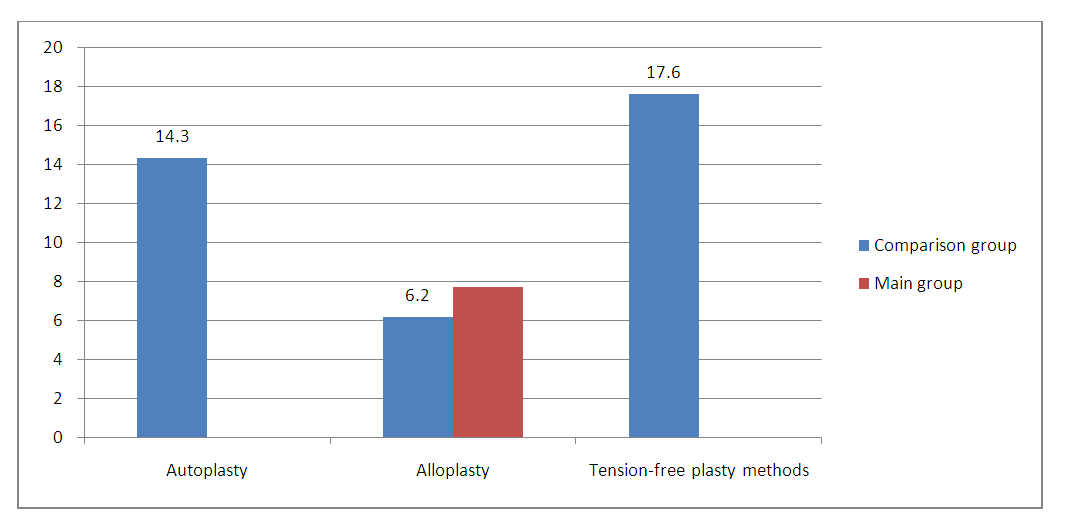 | Figure 9. Recurrence rate in ventral hernia after hernioplasty |
5. Conclusions
- • The use of the improved pneumobandage has significantly improved the quality of preoperative preparation of patients with ventral hernia and morbid obesity, reduced the risk of intra-abdominal hypertension after hernioplasty, improved the patient's condition earlier and reduced the incidence of postoperative extra abdominal complications from 7.4% to 4.5% accordingly.• Improvement of technical aspects made it possible: due to stitching the implant in advance with U-shaped sutures, the surgical technique was simplified; and due to combined implant fixation in the distant postoperative period, the cases of recurrence were reduced to zero;• Application of the suggested algorithm taking into account the improved tactical and technical aspects of surgical treatment of ventral hernias in morbidly obese patients allowed reducing the total rate of postoperative complications from 15% to 9% (p=0,045), including wound complications from 11% to 5%, as well as significantly reducing the duration of surgical treatment and rehabilitation periods after various variants of hernio- and abdominoplasty.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML