-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(5): 491-494
doi:10.5923/j.ajmms.20221205.08
Received: April 23, 2022; Accepted: May 7, 2022; Published: May 10, 2022

Pathological Alterations in Cholestasis of the Liver in Maternal Mortality
Erkin A. Eshbaev
Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Erkin A. Eshbaev, Tashkent Medical Academy, Tashkent, Uzbekistan.
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Bile production is one of the vital functions of the body, including the liver. The concept of cholestasis is a disorder of bile production, stagnation in the bile ducts, a disruption of synthesis by hepatocytes, a violation of primary bile capillaries, intrahepatic bile ducts, extrahepatic bile ducts, and duodenal infiltration. Clinically and pathogenetically, bile is manifested by the retention and accumulation in the blood of bile components, i.e. bilirubin, bile acids, and alkaline phosphatase.
Keywords: Pathomophology, Cholestasis, Cholelithiasis, Morphology, Pregnancy, Bile pigments
Cite this paper: Erkin A. Eshbaev, Pathological Alterations in Cholestasis of the Liver in Maternal Mortality, American Journal of Medicine and Medical Sciences, Vol. 12 No. 5, 2022, pp. 491-494. doi: 10.5923/j.ajmms.20221205.08.
1. Introduction
- Cholestasis syndrome is divided into 2 groups: 1) disorders of bile formation; 2) difficulty in bile flow. Pregnancy cholestasis syndrome belongs to the first group of diseases because women develop diseases of the hepatobiliary system at the reproductive age and during pregnancy. During pregnancy, the hormone progesterone affects the tone and motility of the bile duct wall, causing the process of cholestasis. This syndrome is little studied in the scientific literature but is important in obstetric and therapeutic practice.Pregnancy Intrahepatic cholestasis syndrome was first reported in 1883 and detected by F. Alfeld. But in 1954, Swedish scientists A. Svanborg and L. Torling studied the etiology, pathogenesis, and clinical signs of this syndrome as a pregnancy pathology. However, the causes of pregnancy cholestasis remain unknown (24). Nowadays, hormonal theory plays a major role. After all, inadequate inactivation of enzymes and conjugation of steroid hormones carried out by glucuronic and sulfuric acids reduces the ability of liver cells and bile ducts to produce bile. Estrogen conjugates reduce the retention of bile acids from the blood by liver cells. It has been found that in pregnancy cholestasis, the number of progesterone metabolites, which reduce bile acid metabolism and production, increases. Therefore, the peak period of pregnancy cholestasis estrogen levels is observed in the third trimester.
2. Materials and Methods
- Enrichment of information on specific morphological features that characterize the morphogenesis and pathological anatomy of liver disease associated with and associated with pregnancy, which plays an important role in maternal mortality. Clinical-anamnestic, morphological, and histological methods were used in the study to solve the research tasks and achieve the goal. The object of the study - a total of 131 maternal mortality autopsies, of which pregnancy-related - 67, and clinical and anamnestic data and liver of 64 associated liver diseases were obtained.
3. Results and Discussion
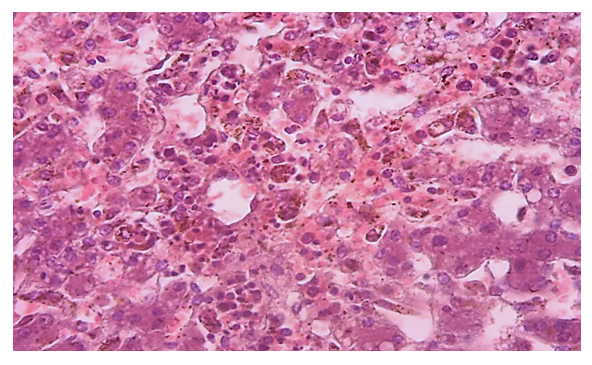
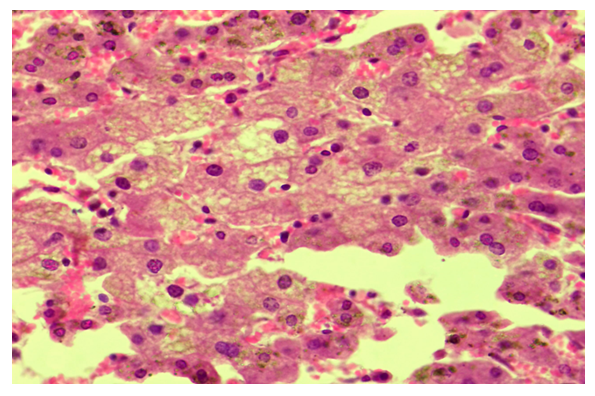
- The results of the morphological examination showed that in hepatic cholestasis in the central part of the liver fragments in the cytoplasm of almost all hepatocytes were found to accumulate dark brown bile pigments of various sizes (Fig. 1). It is observed that in some hepatocytes there are clusters that completely occupy the relatively large cytoplasm. In this case, it is determined that the nuclei of hepatocytes are pushed to the edge of the cell and destroyed to varying degrees. It is found that the disc space between the hepatic columns is enlarged due to edema and plasmorrhagia, hypertrophied Kupfer cells, in which also phagocytosed brown bile pigments appear. It is found that erythrocytes within sinusoids are destroyed to varying degrees and some are hemolyzed.
 | Figure 1. Pregnancy cholestasis, 27-year-old woman. Dark brown bile pigments accumulate in the cytoplasm of hepatocytes Stain: H-E. Size: 10x40 |
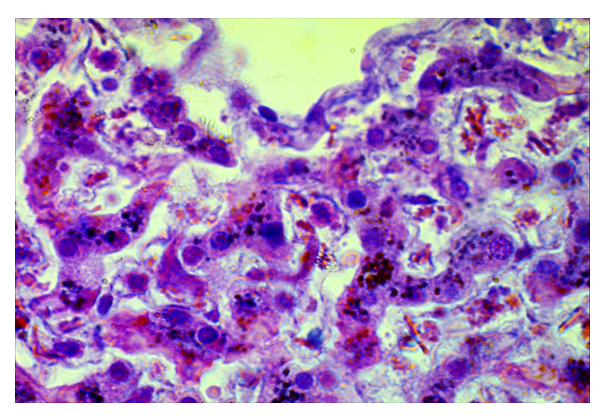
 | Figure 3. Pregnancy cholestasis. A 36-year-old woman. Liver parenchyma 2-morphofunctional area Cholestasis of the cytoplasm of hepatocytes. Stain: H-E. Size: 10x40 |
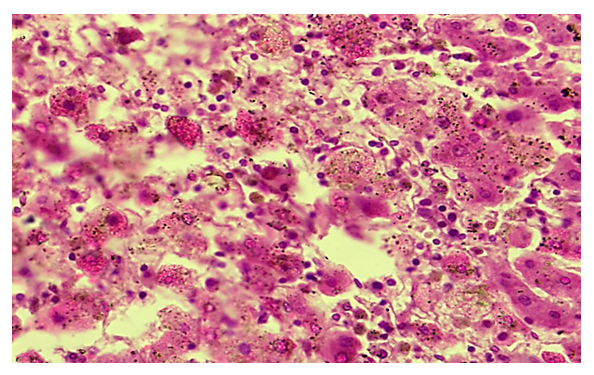
 | Figure 4. Pregnancy cholestasis, 32-year-old woman. The cytoplasm of hepatocytes is enlarged, in which the bile pigments are scattered. Stain: H-E. Size: 10x100 |
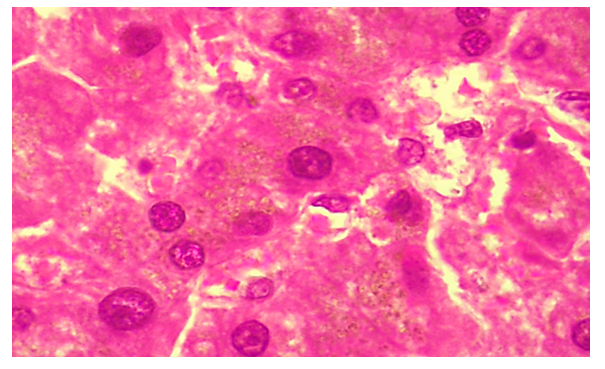
 | Figure 5. Pregnancy cholestasis, 28-year-old woman. Hepatocytes with intracellular cholestasis developed hydropic dystrophy and necrobiosis. Stain: H-E. Size: 10x40 |
4. Conclusions
- Bile production is one of the vital functions of the body, including the liver. The concept of cholestasis is a disruption of the synthesis of bile bile by hepatocytes, primary bile capillaries, intrahepatic bile ducts, extrahepatic bile ducts, and duodenal infiltration. Clinically and pathogenetically, bile is manifested by the retention and accumulation in the blood of a component of bile, namely bilirubin, bile acids and alkaline phosphatase. During pregnancy, the hormone progesterone affects the tone and motility of the bile duct wall, causing the process of cholestasis. This syndrome is little studied in the scientific literature, but is important in obstetric and therapeutic practice. The following specific changes in the liver are observed in patients with gestational cholestasis. Accumulation of bile pigments in the cytoplasm of hepatocytes, dilation of bile capillaries and pathways, stagnation of bile in them, the formation of bile clots, manifested by varying degrees of destruction, necrobiosis and necrosis of hepatocytes. Hypertrophy of Kupfer cells in the sinusoidal wall and interstitial tissue, accumulation of free macrophages, phagocytosis of bile pigments in the cytoplasm are observed.According to the literature, pathomorphological changes in the liver characteristic of gestational cholestasis are the accumulation of bile pigment in the cytoplasm of hepatocytes, stagnation in the bile capillaries and pathways, necrobiosis and necrosis of hepatocytes, proliferation of macrophages. In our material, this type of pathomorphological changes did not always occur, and their incidence was as follows: the accumulation of bile pigment in the cytoplasm of hepatocytes is constant, stagnation in the bile capillaries and pathways - 75.0%, necrobiosis and necrosis of hepatocytes - 54.2%, proliferation of macrophages was constantly observed.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML