Ibodullaev Bekhzod Bakhromovich
Assistant of Department of Neurology and Psychiatry, Urgench Branch of the Tashkent Medical Academy, Uzbekistan
Correspondence to: Ibodullaev Bekhzod Bakhromovich, Assistant of Department of Neurology and Psychiatry, Urgench Branch of the Tashkent Medical Academy, Uzbekistan.
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article discusses the study of the structure of adaptation disorders using effective psycho-diagnostic methods in the diagnosis of adaptation disorders in patients with type 2 diabetes mellitus and the use of effective medical and psychological methods in therapeutic processes and treatment effectiveness.
Keywords:
Adaption, Anxiety, Diabetes, Frustration, Psychotherapy
Cite this paper: Ibodullaev Bekhzod Bakhromovich, Medical-Psychological Approach to the Correction of Adaptation Disorders Developed in Patients with Second Type of Diabetes, American Journal of Medicine and Medical Sciences, Vol. 12 No. 5, 2022, pp. 481-486. doi: 10.5923/j.ajmms.20221205.06.
1. Introduction
According to the World Health Organization (WHO), there is a growing number of medical, social and demographic diseases in our region, one of which is type 2 diabetes. According to the seventh edition of the 2015 Atlas of the International Association of Diabetologists (IDF Atlas diabetes 7 st publication), the number of patients with type 2 diabetes was 415 million, and by 2040 this figure will reach 642 million. It has become a global problem in the health care system, with experts predicting that the disease will become the seventh leading cause of death by 2030. [2]. Analysis of diabetes mellitus in Uzbekistan until 2019 showed that the total number of patients diagnosed with diabetes was 230,610, of which 18,349 were type 1 QD, and the remaining 212,261 were type 2 [3]. Type 2 diabetes is not only a medical and social problem today, but also one of the highest medical and psychological problems. Studies show that 80% of patients with type 2 diabetes suffer from some form of psychopathological disorder [4,5]. These conditions, in turn, are manifested in patients with psycho-emotional conditions such as adaptive disorders, anxiety, depression [6]. Patients with type 2 diabetes have mainly chronic adaptive stress disorders, the rate of which is 7-10%. An increase in the rate of adaptive disorders in approximately 30–50% of patients diagnosed with a serious complication associated with the disease has been reported in scientific sources [7]. These cases require timely detection and correction of disorders of adaptive processes in patients.Objective: To use psycho-diagnostic methods and effective medical and psychological correction in the screening of adaptation disorders in patients with type 2 diabetes treated in the endocrinology department of the clinic of the Urgench branch of the Tashkent Medical Academy.
2. Materials and Methods
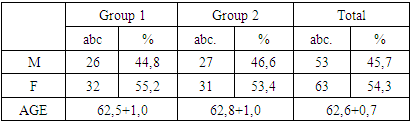
The TTA was conducted in the endocrinology department of the Urgench branch in 116 patients being treated for type 2 diabetes. Of these, 53 were men and 63 were women. The patient group consisted of individuals aged 39–75 years, with an average age of 62.8 + 0.7. The somatic condition of our patients is studied on the basis of complaints, anamnesis, objective and subjective, paraclinical data when they come to the clinic for treatment. A special medical-psychological questionnaire was used to assess the mental status of our patients. In assessing the degree of adaptive disorders in patients, the following psychometric tests were used in our study:● Statistical analysis of pre- and post-treatment parameters was performed using the Eysenck (assessment of patients ’own mental state) questionnaire. In our study, psycho-correction of psycho-adaptation disorders was performed by dividing patients into two groups:Group 1: A psychotherapeutic algorithm based on basic treatment and rational emotional psychotherapy was applied to patients in this group: n - 58.Group 2: Basic treatment and rational psychotherapy were used in patients in this group: n - 58.Rational psychotherapy and rational-emotional psychotherapy were selected from the psychotherapeutic methods performed on patient the distribution of our patients was as follows:Table 1
 |
| |
|
According to the table, 26 (44.8%) of our patients in group 1 were men, 32 (55.2%) were women, their average age was 62.5 + 1.0, 2 - 27 (44.6%) patients in the group were men, 31 (53.4%) were women, their average age was 62.8 + 0.7.
3. Results
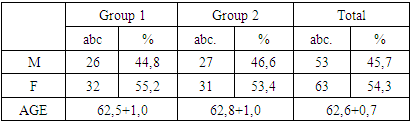
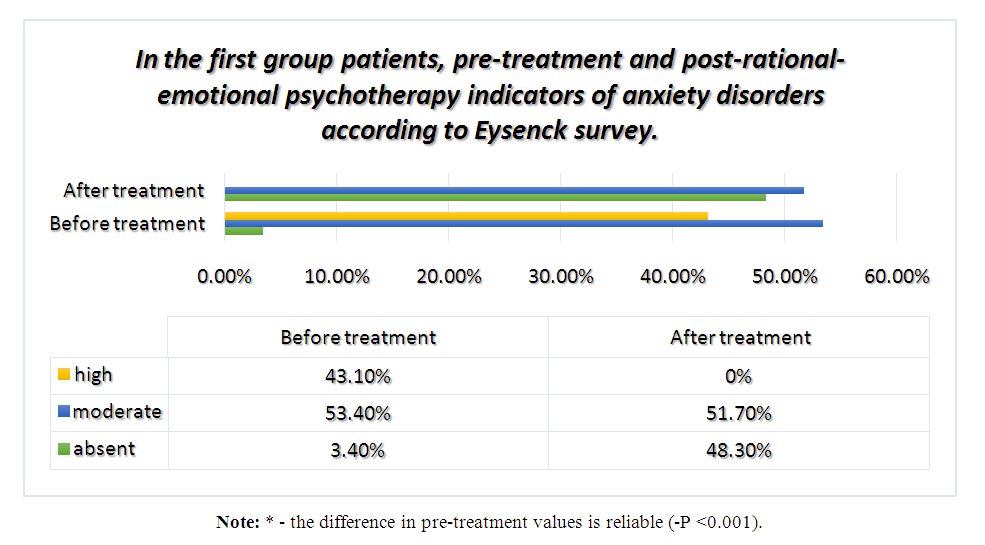
The following results were obtained using the Eysenck survey to identify advanced adaptive disorders in our patients. According to the survey, the structure of adaptive disorders developed in our patients was formed on the basis of 4 small scales of the questionnaire, namely, anxiety, aggression, frustration and rigidity, and pre-treatment and post-treatment indicators were statistically analyzed on the basis of diagrams and tables. According to the analysis, the pre-treatment and post-treatment indicators on the anxiety scale of the Eysenck survey of our patients in group 1 were as follows (Diagram 1).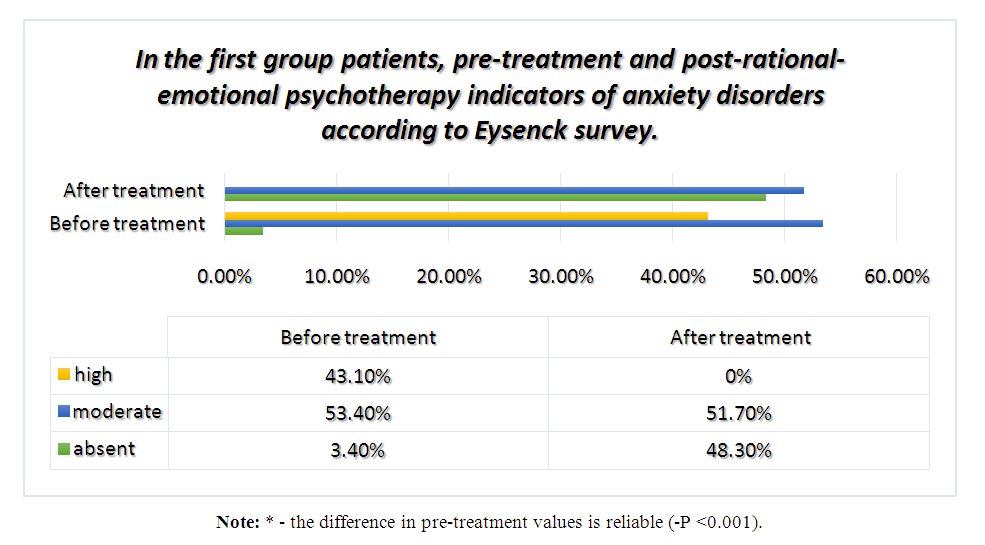 | Diagram 1 |
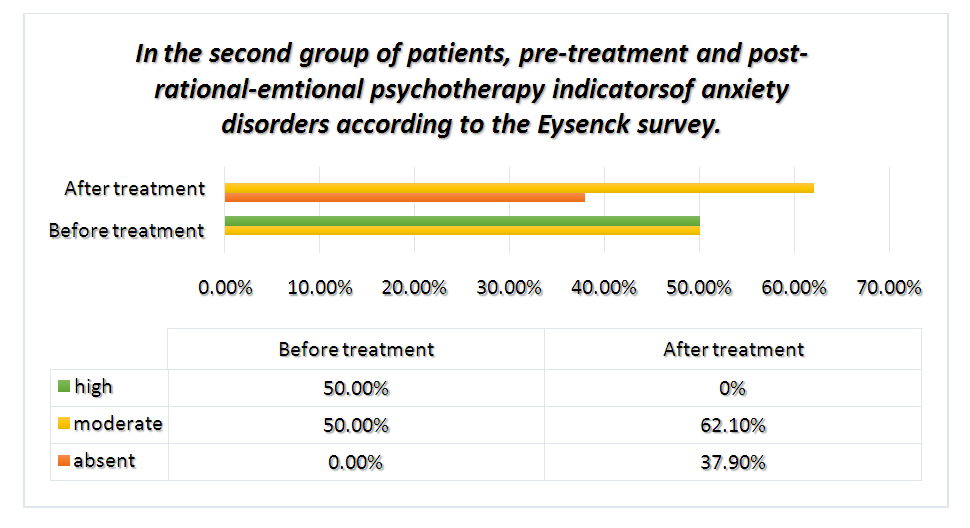
Analysis of the results showed that in 3.4% (n = 2) of our patients before the treatment there was no anxiety or mild (7.0 + 0.0), 53.4% (n = 31) (12.8 + 0.21) moderate, 43.2% (n = 25) severe (17.8 + 0.25) anxiety disorders were detected. This figure is higher in 48.3% (n=28) of patients after anxiety-sensory psychotherapy (ASP), when anxiety disorders were not detected at all or were mild (6.4 + 0.12), 51,7% (n= 0.26) anxiety disturbances (-P<0.001). In our group 2 patients, the following results were obtained during the comparative analysis of pre-treatment and post-treatment indicators (Diagram 2).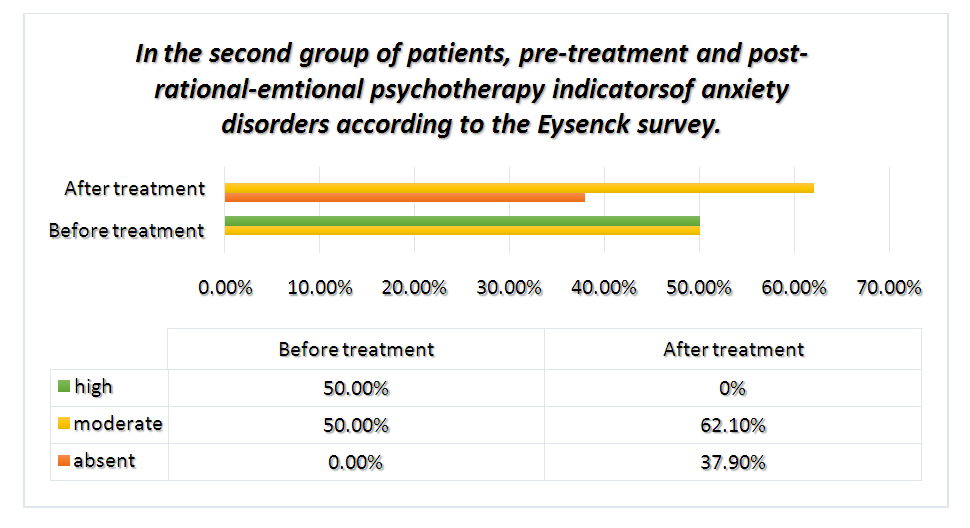 | Diagram 2 |
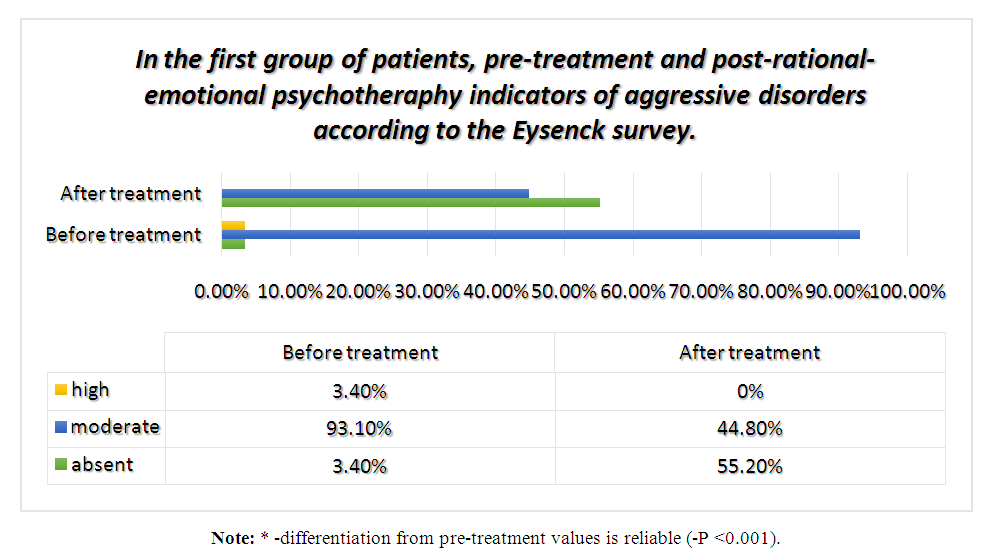
Analysis of the results showed, which obtained in the second group of patients that before treatment in 50% (n = 28) was moderate (12.6+0.21), in 50% (n = 28) was high (17.6+0.18) anxiety diturbances were detected. This figure was significantly higher in 37.9% (n = 22) of patients with anxiety disorders who were not detected at all or had a mild appearance (6.5 + 0.18) after 62 days of rational psychotherapy (RP). % (n = 36) reported moderate (9.4 + 0.22) disturbances (-p <0.001). Analyzing the indicators identified on the anxiety scale of the above Eysenck questionnaire, we can say that in patients with mild and moderate anxiety disorders after psychotherapy in both groups of symptoms associated with mild or anxiety disorders.In our patients with high levels of anxiety disorders, we can see that these indicators decreased to moderate and mild (-p <0.001).The following results were obtained when analyzing the second scale of the Eysenck questionnaire, i.e., pre-treatment aggression in patients, compared with post-treatment indicators. Analysis of the results obtained from our patients in group 1 (diagram 3).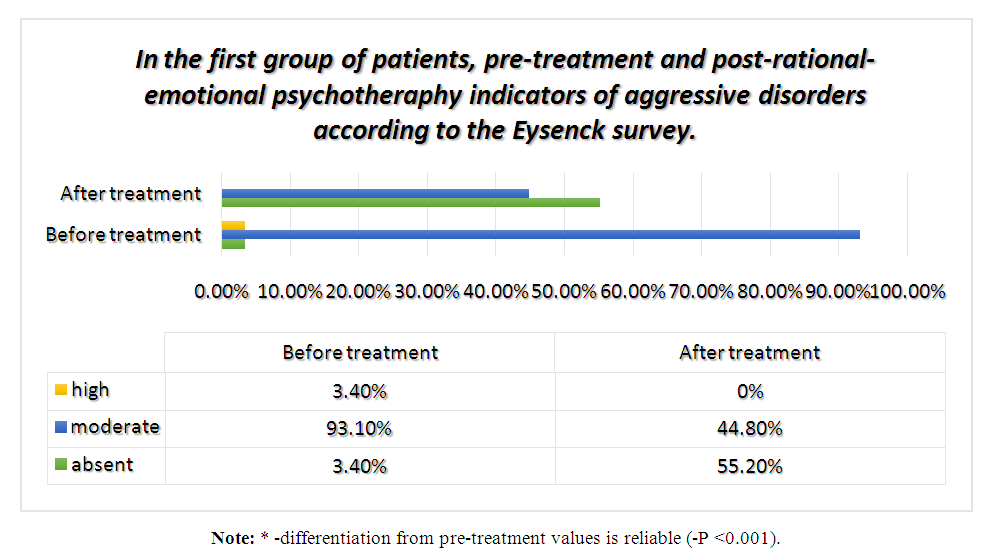 | Diagram 3 |
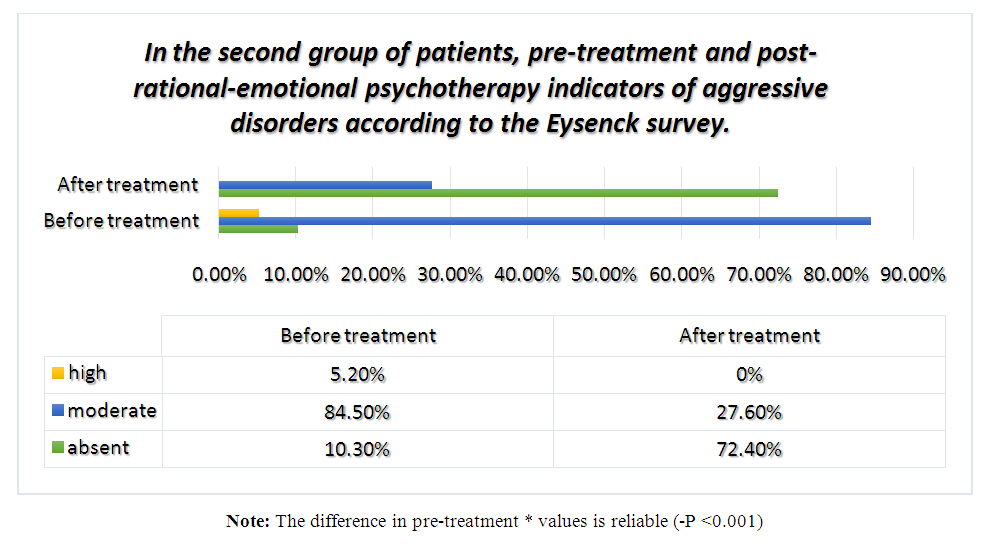
Analysis of the results obtained in group 1 showed that 3.4% (n = 2) of our patients had no aggressive disorders before treatment or were mild (7.0 + 0.0), 93.4% (n = 54) (12.0 + 0.18) moderately severe, 3.4% (n = 2) severe (18.0 + 0.0) aggressive disorders were detected.This indicator is similar to that in 55.2% (n = 32) of patients after rational-emotional psychotherapy (REP), aggressive disorders were not detected at all or were mild (6.3 + 0.09). 44.8% (n = 26) reported moderate (8.7 + 0.16) aggressive disturbances (-P <0.001).In our second group, the following results were obtained when analyzing these indicators (Diagram 4).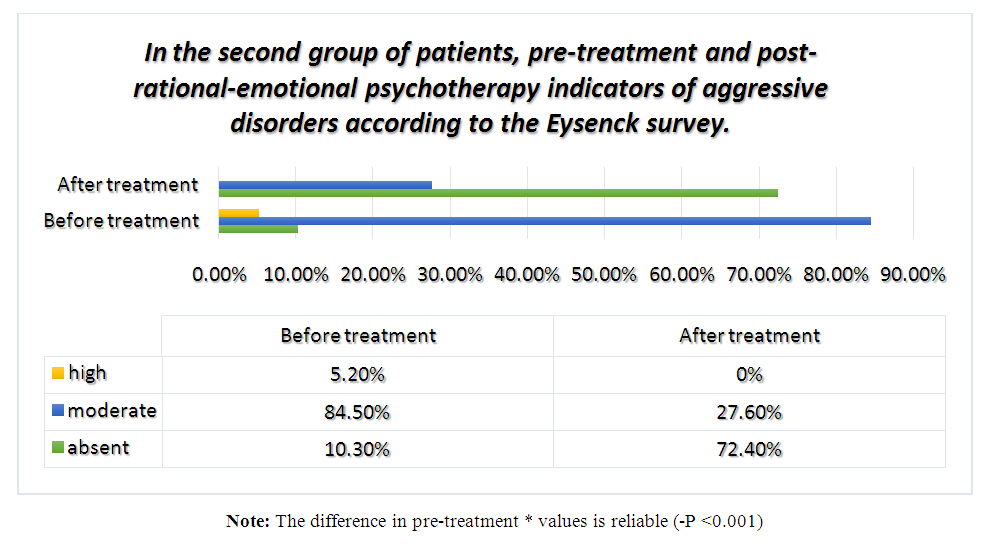 | Diagram 4 |
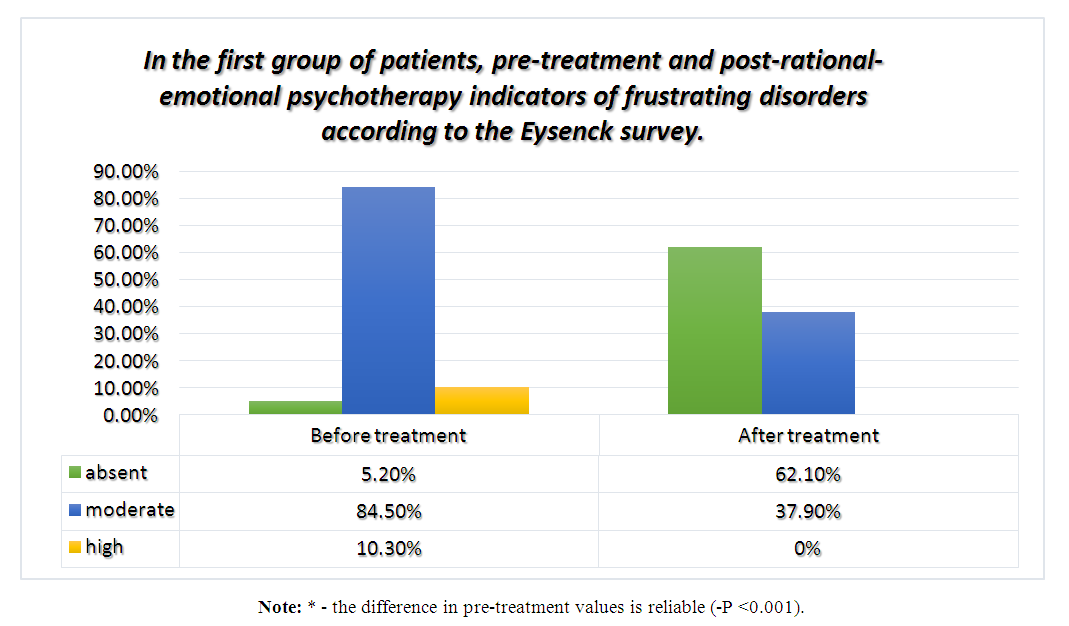
Analysis of the results obtained in group 2 showed that 10.3% (n = 6) of our patients had no aggressive disorders before treatment or were mild (7.0 + 0.0), 84.5% (n = 49). moderate (11.7 + 0.23), high-level (17.0 + 0.58) aggressive disorders were detected in 5.2% (n = 3). This figure was higher in 72.4% of patients (n = 42) after aggressive psychotherapy (AP) who had no or no aggressive symptoms at all (6.2 + 0.10), 27, 6% (n = 16) reported moderate (8.7 + 0.12) aggressive disturbances (-P <0.001). Analyzing the indicators of the Eysenck survey on the scale of aggression, we can say that the regression of symptoms associated with mild and aggressive disorders was observed in both groups after psychotherapy in patients with mild and moderate aggressive disorders identified in our patients. In our patients with high levels of aggressive disorders, we can see that these indicators decreased to moderate and mild (-p <0.001).The following results were obtained when the third scale of the Eysenck questionnaire, i.e., pre-treatment frustration indicators in patients, was compared with post-treatment indicators. Analysis of the results obtained from our patients in group 1 (diagram 5).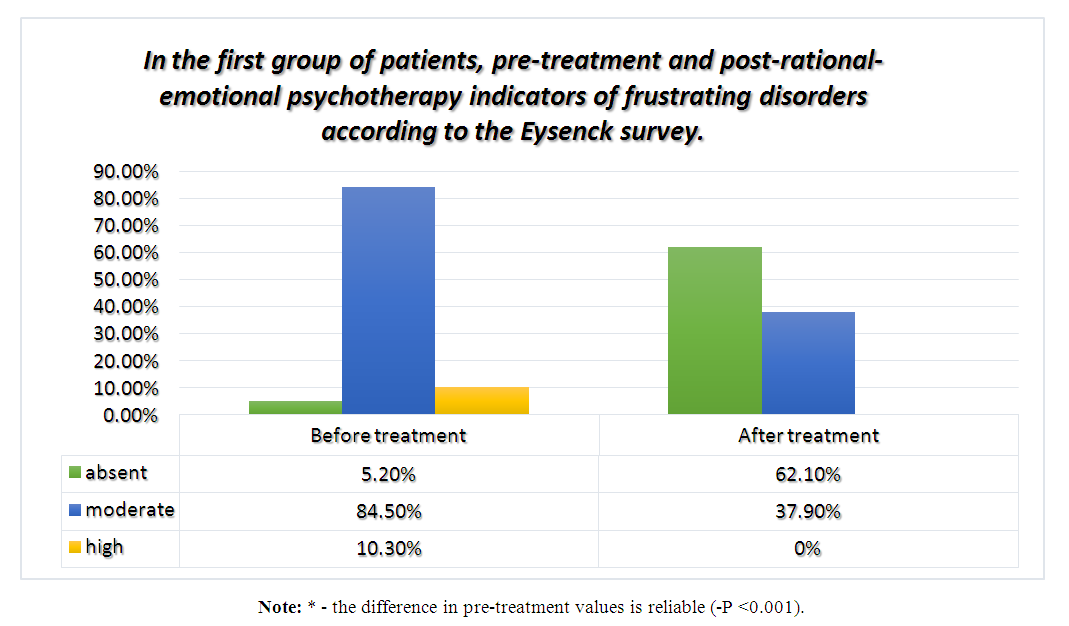 | Diagram 5 |
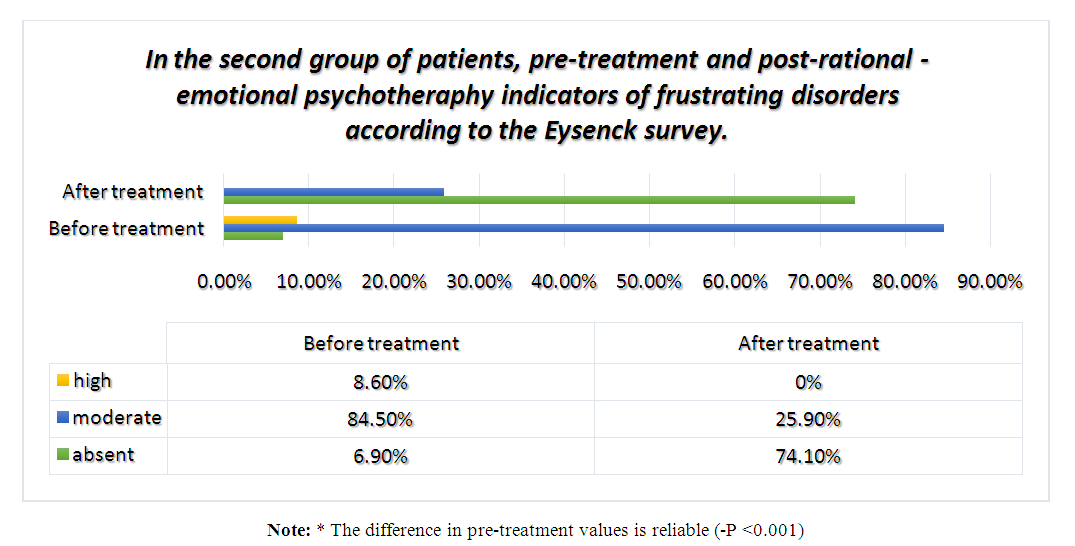
Analysis of the results obtained in group 1 showed that in 5.2% (n = 3) of patients before treatment there were no disorders of frustration or mild (7.0 + 0.0), 84.5% (n = 49) had moderate (12.6 + 0.16) and 10.3% (n = 6) had severe (18.3 + 0.21) frustration disorders. These indicators showed that frustration disorders were not detected at all or were mild in 62.1% (n = 36) of patients after rational-emotional psychotherapy (REP) (6.4 + 0.10). , 37.9% (n = 22) reported moderate (8.4 + 1.0) frustration disorders. (-P <0.001).Analysis of these indicators in patients of group 2 gave the following results (diagram 6).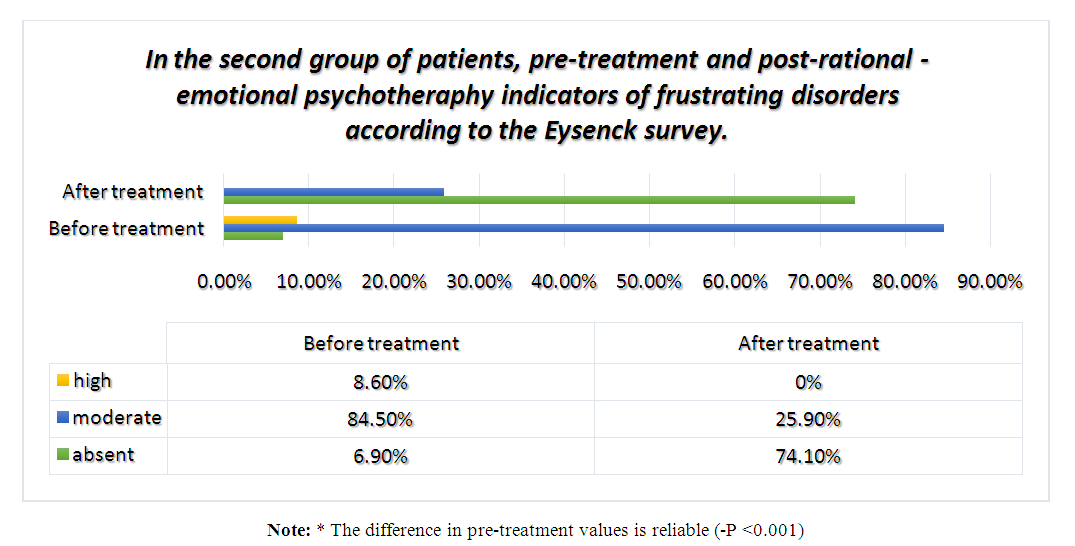 | Diagram 6 |
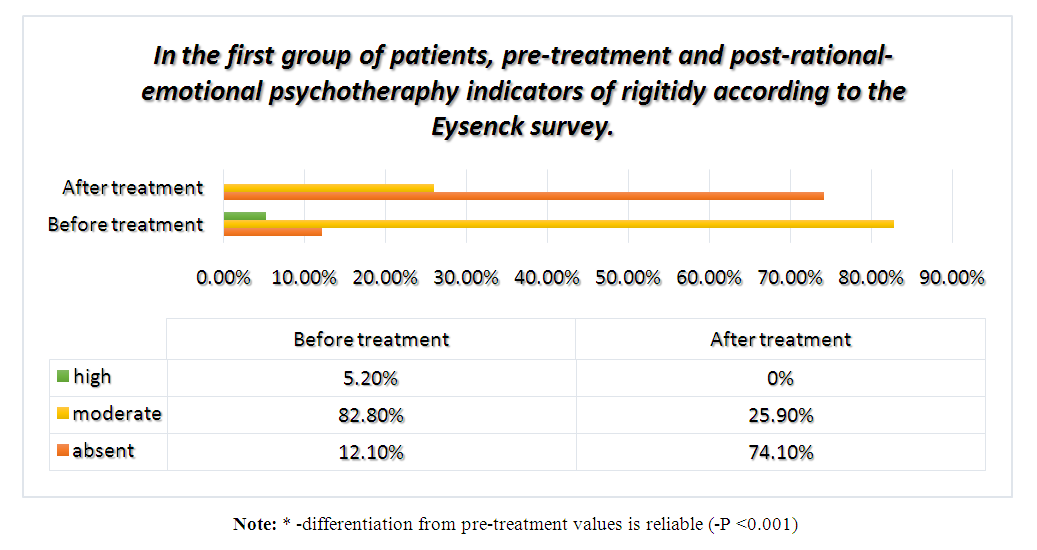
Analysis of the results obtained in group 2 showed that 6.9% (n = 4) of our patients had no frustration disorders before treatment or were mild (7.0 + 0.0), 84.5% (n = 49). moderate (12.4 + 0.22), 8.6% (n = 5) and high (17.0 + 0.58) frustration disorders were detected. These indicators showed that in 74.1% (n = 43) of patients after rational psychotherapy (RP), frustration disorders were not detected at all or were mild (6.4 + 0.12), 25, 9% (n = 15) reported moderate (8.7 + 0.18) frustration disorders (-P <0.001). Analyzing the indicators identified on the frustration scale of the Eysenck survey above, we can say that regression of symptoms associated with mild frustrating disorders was observed in both groups after psychotherapy in patients with mild to moderate frustration disorders identified in our patients. And in our patients with high levels of frustration disorders, we may see a decrease in these rates to moderate to mild (-p <0.001).The next scale of the Eysenck questionnaire, i.e., pre-treatment rigidity levels in patients, was analyzed in comparison with post-treatment indicators, and the following results were obtained. Analysis of the results obtained from our patients in group 1 (diagram 7).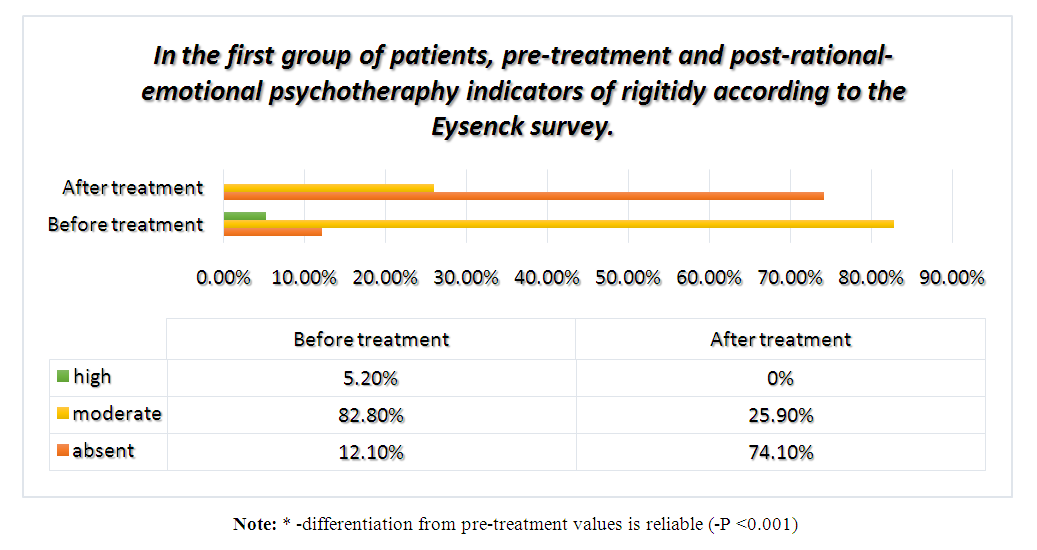 | Diagram 7 |
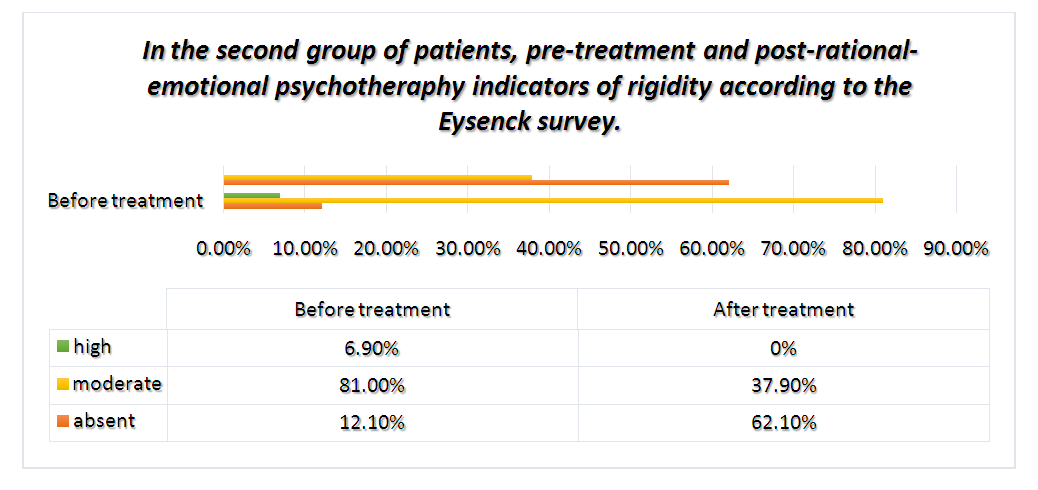
Analysis of the results obtained in group 1 showed that 12.1% (n = 7) of our patients did not have rigidity disorders before treatment or were mild (7.0 + 0.0), 82.8% (n = 48) in moderate (12.7 + 0.21), 5.2% (n = 3) in severe (18.0 + 1.5). These indicators showed that after rational-emotional psychotherapy (REP), 74.1% of patients (n = 43) had rigidity disorder. These indicators showed that in 74.1% (n = 43) of patients after rational psychotherapy (RP), frustration disorders were not detected at all or were mild (6.4 + 0.12), 25,9% (n = 15) reported moderate (8.7 + 0.18) frustration disorders (-P <0.001). In group 2 patients, the analysis of these indicators allowed to obtain the following results (Diagram 8).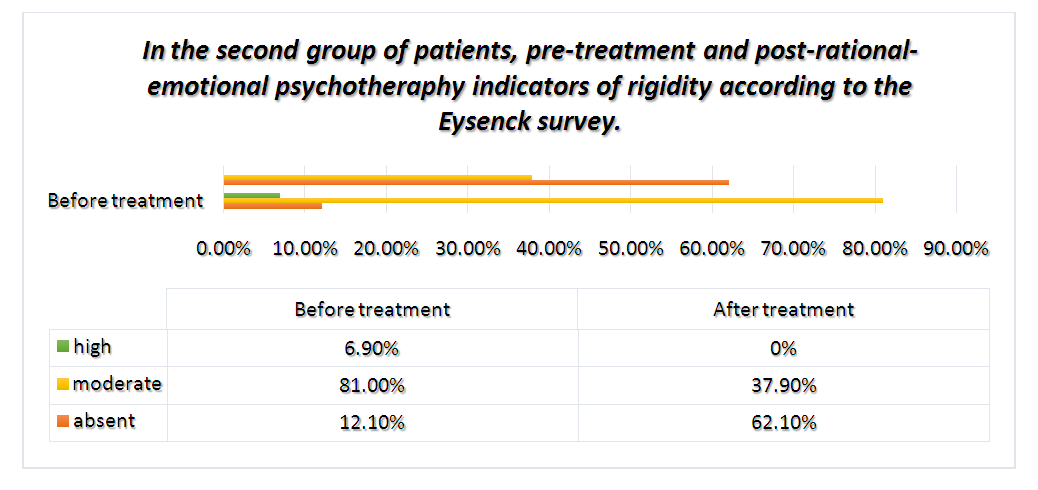 | Diagram 8 |
Analysis of the results obtained in group 2 showed that 12.1% (n = 7) of our patients had no rigidity before treatment or mild (7.0 + 0.0), moderate in 81.0% (n = 47) (12.3 + 0.24), 6.9% (n = 4) and high (8.9 + 0.19) stiffness were detected. These indicators showed that after rational psychotherapy (RP), 62.1% (n = 36) of patients had no rigidity that was not detected at all or was mild (6.4 + 0.12), 37. Medium (8.9 + 0.19) stiffness was observed in 9% (n = 22) (P <0.001). Analyzing the indicators of the rigidity scale of the Eysenck survey above, we can say that the regression of mild or rigidity-related psychological disorders was observed in both groups after psychotherapy in patients with mild to moderate rigidity identified in our patients. In our patients with high levels of rigidity, we can see that these values decreased to moderate and mild (-p <0.001).
4. Conclusions
From the above results, it can be concluded that timely psychodiagnostics of adaptive disorders in patients with type 2 diabetes plays a significant role in the analysis of the psychological status of each patient, as well as in assessing the effectiveness of psychotherapy. Secondly, during the medical and psychological care of our patients, it was found that the method of psychotherapy used in the correction of adaptive disorders in the first group of patients, the method of rational-emotional psychotherapy, was more effective than rational psychotherapy in the second group. our observations have shown that choice in correction is a method of psychotherapy and at the same time plays an important role in improving the quality of life of patients.
References
| [1] | International Diabetes Federation, Diabetes Atlas, Sixth edition. Brussels, Belgium: International Diabetes Federation, 2014. http://www.idf.org. |
| [2] | IDF. Diabetes Atlas Seventh Edition 2015. http://www.diabetatlas.org. |
| [3] | Алиева А.В., Исмаилов С.И., Рахимова Г.Н. Эпидемиология сахарного диабета и предиабета в Узбекистане: резултаты скрининга. Ж.Теор. и Клин. Мед. -2017. -№2. -С.58-61. |
| [4] | Ströhle A (2009) Physical activity, exercise, depression and anxiety disorders. J Neural Transm 116: 777–784. doi: 10.1007/s00702-008-0092-x. |
| [5] | Lin EHB, Rutter CM, Katon W, et al (2010) Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care 33:264–9. doi: 10.2337/dc09-1068. |
| [6] | Spiegel D, Giese-Davis J (2003) Depression and cancer: mechanisms and disease progression. Biol Psychiatry 54: 269–282. doi: 10.1016/S0006-3223(03)00566-3. |
| [7] | Краснов В.Н., Бобров А.Е., Старостина Е.Г. и др. Совершенствование профессиональной компетентности специалистов первичного звена здравоохранения в целях раннего выявления психических расстройств и предупреждения их неблагоприятного развития (на основе исследований, проведенных в 2008 г.): Методические рекомендации. М.: ООО «ИПУЗ», 2009. 32 с. |
| [8] | Краснов В.Н., Бобров А.Е., Довженко Т.В. и др. Проблемы, предпосылки и необходимые мероприятия по улучшению взаимодействия психиатрической (психотерапевтической) службы с врачами первичного звена здравоохранения // Психическое здоровье. 2011. Т. 63 (8). С. 3—11. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML