-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(5): 466-470
doi:10.5923/j.ajmms.20221205.04
Received: April 19, 2022; Accepted: May 7, 2022; Published: May 10, 2022

Morphological Changes in the Oral Mucous Membrane in Patients with COVID-19
Rizaev Jasur Alimjanovich, Ahrorova Malika Shavkatovna, Kubaev Aziz Saydalimovich, Hazratov Alisher Isamiddinovich
Samarkand State Medical Institute, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The objects of the study were 105 patients with Covid-19 disease. The aim of the study is to examine morphological changes in the oral mucosa and taste sensitivity in patients with COVID-19 with varying degrees of severity. COVID-19 is predisposing factors for oral lesion formation. Stress-induced oral ulcers may increase among patients due to pandemic-associated fear. The study determined morphological and taste changes in the oral cavity. Conclusions: lesions of the oral mucosa (oral manifestation) indicate the highest expression of ACE-2 receptors in the oral cavity, which requires special attention to the organization of therapeutic and preventive consultations by dentists for patients in order to actively treat diseases of the oral cavity and prevent oral-vascular diseases. pulmonary route of development of the COVID-19 virus.
Keywords: COVID-19, Oral mucous membrane, Osseointegration, Microcirculation, Vacuum therapy
Cite this paper: Rizaev Jasur Alimjanovich, Ahrorova Malika Shavkatovna, Kubaev Aziz Saydalimovich, Hazratov Alisher Isamiddinovich, Morphological Changes in the Oral Mucous Membrane in Patients with COVID-19, American Journal of Medicine and Medical Sciences, Vol. 12 No. 5, 2022, pp. 466-470. doi: 10.5923/j.ajmms.20221205.04.
Article Outline
1. Relevance of the Problem
- Today, COVID-19 is a very common disease worldwide. Coronavirus disease 2019 (COVID-19), caused by RNA coronavirus 2 severe acute respiratory syndrome (SARS-CoV-2), belonging to the beta-corona virus subfamily, is the most urgent, socio-economic public health problem that has acquired pandemic proportions. Up to date, a new strain of COVID-19 has been identified. Given the ongoing trend of strain modification, COVID-19 is an unprecedented, serious medical and social problem of all mankind, far from being solved. [2,3].Today, it has been established that age over 65 years, male gender [4], cardiovascular disease [5], diabetes mellitus [6], obesity [7], chronic obstructive pulmonary bronchitis [8], smoking, lack of oral hygiene [9], neoplastic disease, liver disease, opportunistic infections, stress, immunosuppression, vasculitis, and COVID-19-induced hyperinflammatory response are predisposing factors for oral lesions in this category of patients. Stress-induced oral ulcers may increase among patients due to pandemic-associated fear. Also, older age and higher severity of COVID-19 disease is associated with severe oral disease [10-12].At present, in the world practice, the most relevant questions remain regarding the complex diagnosis of clinical forms and courses of this disease based on determining the initial state of the oral mucosa in combination with the study of markers of the body's immune and inflammatory responses. Numerous scientific studies are ongoing to investigate the direct/indirectly proportional effect of baseline oral mucosal health on clinical disease, clinical outcome, and convalescence in SARS-CoV-2, as well as the association of baseline relative abundance of oral bacterial species with pro-inflammatory cytokine response and associations local immune response with the clinical course of the disease.The mucosal immune system is the largest component of the entire immune system, which has evolved to provide protection at the main sites of infection: in the mucosa. Since COVID-19 primarily affects the upper respiratory tract, its first interactions with the immune system should occur predominantly on the mucosal surfaces of the respiratory tract during both the induction and effector phases of the response. However, almost all research on the immune response in COVID-19 has focused exclusively on serum antibodies and systemic cell-mediated immunity, including innate responses [2,5].At the present stage of domestic healthcare development, large-scale work continues on social protection of the population and healthcare system reform. In the field of virology, in particular, in improving the timely diagnosis and detection of high-risk SARS-CoV-2 patients, and in the rehabilitation of patients after this virus transfer, positive results have been achieved. At the same time, in order to improve an immediate and long-term treatment results, as well as to prevent severe complications after the passing active phase of the disease, these patients require evidence-based studies to assess the comprehensive oral mucosa assessment state within the study of morphological changes in the oral cavity.PURPOSE OF THE WORK study of morphological changes in the oral mucosa and taste sensitivity in patients with COVID-19 with varying degrees of severity.
2. Materials and Research Methods
- The study included 105 patients (total number of patients 254 patients) (62 men and 43 women) aged 18 to 55 years (mean age 41.6 ± 4.7 years), who were included in the study, since 149 patients were excluded by exclusion criteria - 3 patients were under 18 years of age, 7 patients were over 55 years, 15 patients were smokers, 30 were severely obese, 1 patient was pregnant, 87 patients had comorbidities, and 6 patients refused to provide consent to complete the questionnaire. All patients were positive in the polymerase chain reaction test for COVID-19.The study design was a cross-sectional survey based on a questionnaire. This survey contains the following demographic data: gender, age, weight, height, educational level, and overall health. The questionnaire was divided into two parts:1) The first part includes the oral hygiene assessment state results obtained by a group of dentists.2) The second part contains data on the COVID-19 severity, which was obtained through a phone call.All patients underwent a daily visual examination of the oral cavity, registration and clinical course assessment, temperature severity, symptoms of intoxication.
3. Study Results
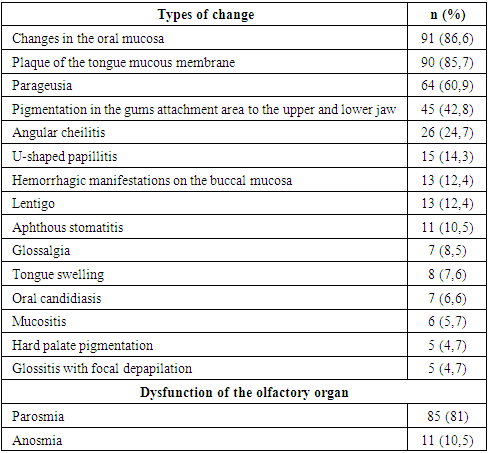
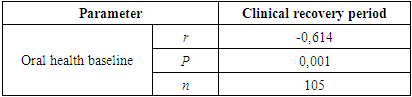
- On examination, changes were found in the oral mucosa in 91 patients (86.6%) (Table 1).
|
|
|
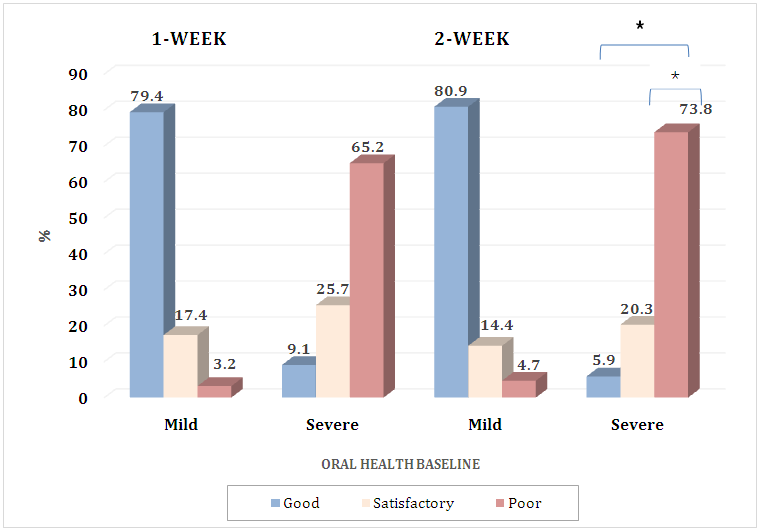
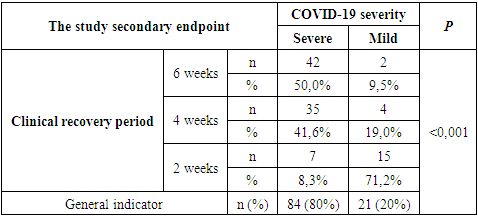
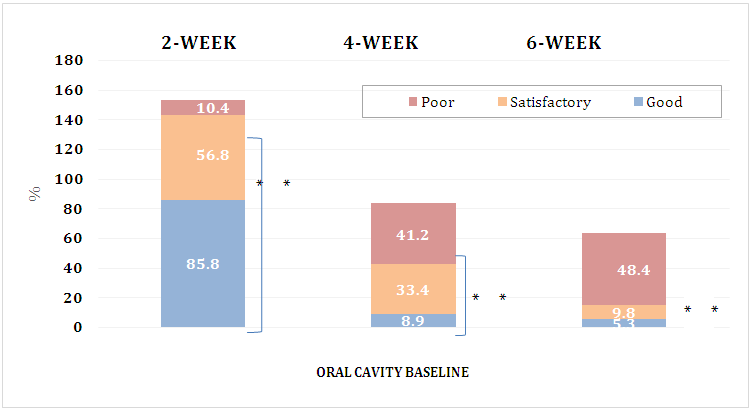 | Figure 2. Exploring the secondary endpoint. Initial state of oral health relationship with the period of clinical recovery. **p <0,001 |
|
|
4. Conclusions
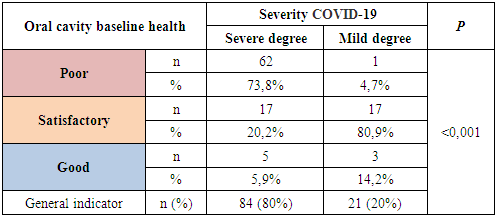
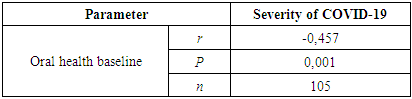
- According to the analysis, a high level of damage to the oral mucosa was determined, which occurred in 91 patients (86.6%). It should be noted that 13 (12.4%) patients had hemorrhagic manifestations on the buccal mucosa, while the anamnesis of this disease was not aggravated. In addition, there were petechial hemorrhages on the lips and cheeks mucous membrane. Also, lips cyanosis was established in these patients. The color of the oral mucosa varied from the usual pale pink to cyanotic due to the lips inner surface mucous membrane appearance of different levels according to the vascular pattern severity. Pigmentation in the area of gums attachment to the upper and lower jaws occurred in 45 (42.8%) patients, while in 5 (4.7%) pigmentation was observed in the hard palate area. Also, lentigo - a brown spot caused by the accumulation of melanin, rising above the surface of the upper and lower lips mucous membrane, was detected in 13 (12.3%) patients. Mycological culture analysis was performed in all cases and was positive in 6.6% of patients (n = 7). Other mucosal manifestations were aphthous stomatitis in 10.5% of patients (n = 11) and mucositis in 5.7% (n = 6). 8.5% of the patient (n = 7) complained of glossalgia, which is the appearance of a burning sensation of the tongue or the entire oral mucosa. In addition, the most common change manifestation in the tongue mucous membrane was pronounced angular cheilitis, consisting in the mouth corners inflammation, characterized by cracks formation, crusts and redness of the mouth mucous membrane in 26 (24.7%) patients. Particular attention was paid to transient U-shaped papillitis detected in 15 patients (14.3%), while tongue edema was detected in 8 patients (7.6%). Inflammatory disease of the tongue, characterized by glossitis with focal depapilation, was observed in 5 patients (4.7%). Plaque of the mucous membrane of the tongue was detected in 90 patients (85.7%), the color of which varied from white to light cinnamon and brown. At the same time, the plaque was easily removed by scraping, papillae, uniform in severity, were also noted over the entire surface of the tongue.A perversion of taste sensitivity, the appearance of taste sensations in the absence of an appropriate stimulus - parageusia was determined in 60.9% of patients (n = 64), which is often accompanied by complaints of distorted perception of smells - parosmia in 81% of patients (n = 85) after 5 days of observation. In addition, 10.5% (n = 11) of patients had a lack of odor perception - anosmia.Thus, the above high level of manifestation in the form of oral mucosa lesion (oral manifestation) indicates the highest expression of ACE-2 receptors in the oral cavity, which requires special attention in the organization of treatment and preventive consultations by dentists for patients in order to actively treat oral cavity diseases, and oral-vascular-pulmonary route development prevention in the COVID-19 virus, as well as monitoring compliance with clinical guidelines developed by the European Federation of Periodontology [1].
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML