-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(4): 441-445
doi:10.5923/j.ajmms.20221204.15
Received: Apr. 8, 2022; Accepted: Apr. 22, 2022; Published: Apr. 29, 2022

Comparative Analysis of the Efficiency of Radiation Methods in the Diagnostics of Functional Parameters in Total Anomalous Pulmonary Venous Drainage
Abrolov H. K., Kholmuratov A. A., Khaidarov A. E., Mamatov M. A., Akbarkhonov B. J., Berdiev K. B., Kobilzhonov B. Kh., Eshonov A. A.
Republican Scientific and Practical Medical Centre for Surgery is Named after Academician V. Vahidov
Correspondence to: Kholmuratov A. A., Republican Scientific and Practical Medical Centre for Surgery is Named after Academician V. Vahidov.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance. Total anomalous pulmonary venous drainage(TAPVD) is a malformation in which all pulmonary veins drain into the right atrium, vena cava, or a combination of both. The incidence of TAPVR ranges from 0.5% to 2% of all congenital heart defects (CHD), or 1/10000 of newborns. The prognosis and outcome of the clinical course of the defect depend largely on the variant anatomy of TAPVD and the functional state of the small circle. TAPVD has a mortality rate of up to 50% in the first 3 months of life and up to 80% by the end of 1 year of life. Objective. To improve surgical outcomes in patients with TAPVD by using modern diagnostic modalities, to evaluate the convergence and divergence between MSCT and ACG in patients with TAPVD. Methods. In-State Institution of Republican Scientific and Practical Medical Centre for Surgery named after Academician V.Vahidov the diagnostic interventions have been carried out on 59 patients from January 2008 up to December 2021. Male patients made up 41 (69.49%), female 18 (30.51%). The sensitivity, specificity, and overall accuracy of ASD and OFO in TAPVD were studied, and comparative correlation analysis between echocardiography, angiocardiography, and multislice computed tomography was performed. Results. We found the following correlation dependence on the left ventricular end-diastolic volume between findings of echocardiography and angiocardiography (Spearman's R 0.89; Kendall's Tau 0.77 and Gamma 0.79; Pearson's correlation coefficient 0.96). The obtained correlation relationship indicates high accuracy of EchoCG data about ACG data, which allows relying on echocardiography data for estimation of left ventricular volumetric and linear parameters. Conclusions. MSCT demonstrates outstanding diagnostic performance, which significantly affects the tactical aspects of the surgical treatment of the defect and its outcome. When assessing the state of the pulmonary circulation, there are significant problems regarding the effectiveness of the standard radiation methods used in assessing the throughput of the pulmonary circulation, which is due to their physical limitations and the difficulty in interpreting the obtained diagnostic information.
Keywords: Total anomalous pulmonary venous return, Echocardiography, Angiocardiography, Computed tomography, Diagnostic efficiency, Open foramen ovale
Cite this paper: Abrolov H. K., Kholmuratov A. A., Khaidarov A. E., Mamatov M. A., Akbarkhonov B. J., Berdiev K. B., Kobilzhonov B. Kh., Eshonov A. A., Comparative Analysis of the Efficiency of Radiation Methods in the Diagnostics of Functional Parameters in Total Anomalous Pulmonary Venous Drainage, American Journal of Medicine and Medical Sciences, Vol. 12 No. 4, 2022, pp. 441-445. doi: 10.5923/j.ajmms.20221204.15.
Article Outline
1. Relevance
- Total anomalous pulmonary venous drainage (TAPVD) is a defect in which all of the pulmonary veins return into the right atrium, vena cava, or a combination of both. The frequency of TAPVR is from 0.5 to 2% of all congenital heart diseases (CHDs), or 1/10,000 newborns. According to the literature, the defect is rare in isolated form, in most cases, it is accompanied by an atrial septal defect (ASD), or other intracardiac shunts [1].According to Darling's classification, there are four types of TAPVD: Supracardial - where the pulmonary veins flow into the superior vena cava system and account for up to 50% of all cases; Cardial - where the pulmonary veins flow into the right atrial cavity or coronary sinus and account for 25% of all cases; Infracardial - where the pulmonary veins flow into the inferior vena cava system in 20% of cases; Mixed type - characterized by a combination of different levels of TAPVR inflow and occurs in 5% of cases. In total abnormal pulmonary vein drainage (TAPVD), all pulmonary veins drain into the right atrium and vena cava system at different levels. The ratio of TAPVD in males to females is 3.6:1 respectively.In TAPVR, pulmonary hypertension has a more aggressive course and is characterized by a severe clinical manifestation requiring urgent surgical care. About 60% of patients with TAPVD have hemodynamic abnormalities that are incompatible with life because of severe pulmonary hypertension and small or no intracardiac shunt (ASD). This causes the rapid development of critical conditions and the death of patients soon after birth, necessitating emergency surgery for vital indications.The prognosis and outcome of the clinical course of the defect depend largely on the variant anatomy of TAPVD and the functional state of the pulmonary circle. In TAPVD, the mortality rate is up to 50% in the first 3 months of life and up to 80% by the end of 1 year of life. The average life expectancy in patients without pulmonary vein occlusion is 2.5 months and 3 weeks in those with occlusion. The study aims to evaluate the convergence and divergence between MSCT and ACG in TAPVD patients.
2. Methods
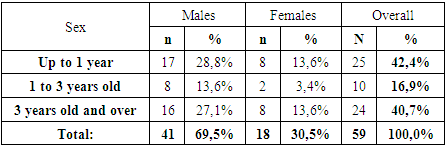
- In the Department of Congenital Heart Disease Surgery of the State Institution of Republican Scientific and Practical Medical Centre for Surgery named after Academician V.Vahidov from January 2008 to December 2021 diagnostic interventions were carried out in 59 patients with TAPVD, of which 52 patients with TAPVD underwent radical correction. The age of patients at the time of inclusion in the study ranged from 1 month. up to 25 years (average 4.3 ± 5.6 years). The weight of the patients varied from 4.0 kg to 75 kg (average 16.94±36.55 kg). The body surface area (BSA) ranged from 0.25 m2 to 1.63 m2 (0.6 ± 0.36 m2 on average). Males were 41 (69.49%) patients, female 18 (30.51%) with a sex ratio (2.28:1) presented in Table 1.
|
|
3. Results
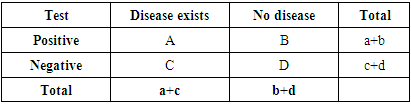
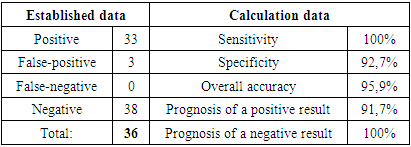
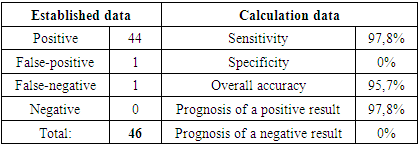
- Despite the importance of accurate preoperative diagnosis of TAPVD, these defect components, even detected as findings during intraoperative revision, do not significantly influence the surgical approach and can be successfully managed if the patient previously met the criteria for operability, including the degree of pulmonary hypertension, which often has a significant impact on the intra- and postoperative course [6].We, therefore, performed a comparative analysis of our radiological methods, taking into account their main advantages and disadvantages to objectively assess their limitations in the diagnosis of TAPVD and its natural course complication of pulmonary hypertension. Due to the hemodynamic and pathophysiological features, TAPVD without Pulmonary Artery Stenosis is always complicated by pulmonary hypertension, which can be of key importance in establishing a contraindication for surgical treatment in grades IIIB-IV [7]. We assessed the correlation of tensiometry findings from echocardiography with angiocardiography and intraoperative tensiometry. Considering that angiocardiography is now the "gold standard" in the diagnosis of pulmonary hypertension, we analyzed echocardiography for sensitivity, specificity, and overall accuracy in pulmonary hypertension presented in Table 3.
|
|
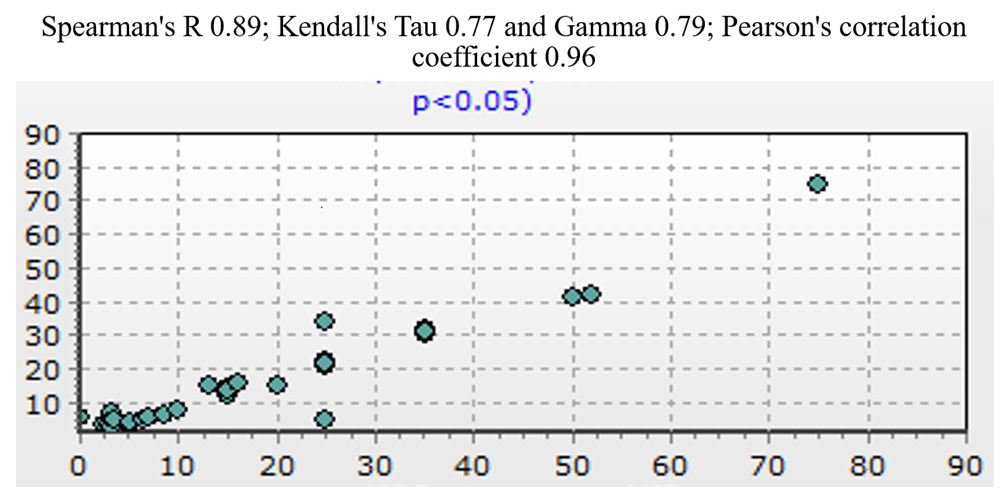 | Figure 1. Scatterplot of correlation dependence on LV EDV between echocardiography and angiocardiography |
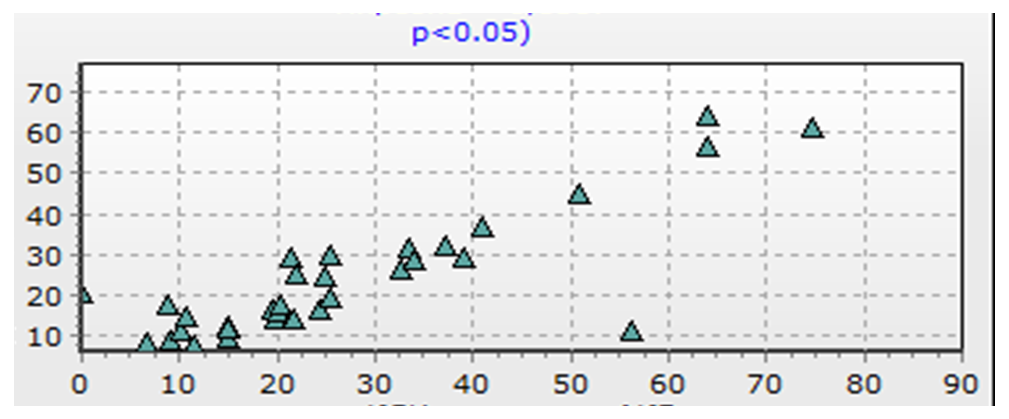 | Figure 2. Scatterplot of the correlation between LV CDI between echocardiography and angiocardiography |
4. Discussion
- In this regard, despite rather close values on LV volume-linear values, it is obvious that the nominal value of LV volume according to echocardiography and angiocardiography has a more close value in comparison with the indexed one. We studied the volume-linear parameters of the LV because several studies on LV geometry in TAPVD state that the small LV volume differs significantly from the typical small, globular LV geometry in hypoplasia of the left heart and has a flattened or sickle-shaped shape, compressed by the dilated RV, which is overloaded by pressure and volume [12].The authors suggest that intrauterine LV volume is normal or close to normal, whereas right ventricular overload with compression of the LV is formed postnatally. According to the authors, a small LV size does not affect the results of surgical correction of TAPVD [13]. Of interest is the fact that, according to some authors, the main reason for the preoperative decrease in LV EDV in patients with TAPVD is the anterior deviation of the interventricular septum due to high pressure in the RV, the so-called LV hypoplasia is determined not so much by compression as by its insufficient filling [14]. Our studies revealed that in patients with TAPVD the baseline LV dimensions correlate with the diameter of the interatrial communication, confirming the importance of the preoperative LV preload restriction mechanism (LV hypovolemia). Based on their findings, the authors believe that the preoperative decrease in LV EDV in patients with TAPVD is predominantly due to deviation.In patients with TAPVD, in the early postoperative period, normalization of the size and increase in LV volume are noted after the elimination of the overload of the right heart by pressure and volume. The hemodynamic integrity of the LV and its ability to provide adequate systemic ejection is further confirmed by the absence of an alternative pathway for left heart chamber decompression in the patient group under study. Thus, based on the comparison of echocardiography data with angiocardiography, we concluded that a strong correlation between echocardiography and angiocardiography data will make it possible to accurately determine LV EDV, which, according to several authoritative studies, is important at the stage of preoperative assessment of TAPVD and in the postoperative period. Since, despite the initial reduction in LV size, elimination of compression and creation of adequate preload ensures 'hemodynamic rehabilitation' of the LV with normalization of its size in the early postoperative period.
5. Conclusions
- Based on comparative correlation analysis, we found a strong correlation between the results of left ventricular assessment obtained from EchoCG and angiocardiography, which in turn also allows us to limit preoperative preparation to ultrasound to reduce preoperative preparation time due to severe TAPVD to optimize the study protocol without compromising the quality and completeness of clinical diagnosis of the defect. Despite the correlations identified in this analysis regarding the effectiveness of the radiological techniques, our results are not intended to be the final truth, but they can be recommended for clinical use with a degree of certainty.
Funding
- The study was not sponsored.
Conflict of Interest
- The authors declare no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML