-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(4): 437-440
doi:10.5923/j.ajmms.20221204.14
Received: Mar. 4, 2022; Accepted: Apr. 15, 2022; Published: Apr. 29, 2022

Mirizzi Syndrome: Prediction of Preoperative Diagnosis
Kurbonov Nizom Azizovich1, Davlatov Salim Sulaymonovich2, Rakhmanov Kosim Erdanovich1, Nabiyev Bobir Bakhodirovich2
1Samarkand State Medical Institute, Samarkand, Uzbekistan
2Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Davlatov Salim Sulaymonovich, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance. Mirizzi syndrome often manifests itself in an acute form; however, the chronic form is an equally or even more common form of manifestation. Although the clinical manifestations of Mirizzi syndrome are nonspecific, the most common form of clinical manifestations of Mirizzi syndrome is mechanical jaundice (60-100%), accompanied by abdominal pain in the upper right quadrant of the abdomen (50-100%) and fever in a patient with known or suspected cholelithiasis. The purpose of the study. Improving the results of diagnosis of Mirizzi syndrome by introducing modern research methods. Research materials. The work is based on the evaluation of the results of surgical treatment of 62 patients with cholelithiasis complicated by Mirizzi syndrome who were hospitalized in surgical departments of the Republican Specialized Scientific and Practical Center for Emergency Medical Care of the Samarkand branch for the period from 2016 to 2021. The results of the study. When examining patients with MS before surgery, 7 patients were faced with the fact that in the presence of signs indicating this complication of the cholelithiasis, they were not taken into account by diagnostic doctors and surgeons and the appropriate diagnosis was not made before surgery. It was considered necessary to identify the most important signs in relation to the diagnosis of MS, to calculate their informativeness. Conclusions. Conclusions. In the diagnosis of MS MRCPG turned out to be non-invasive, the effectiveness was 77.8%, i.e. higher than ERCPG and ultrasound. MRCPG is a method with greater resolution in the diagnosis of Mirizzi syndrome and allowing to determine the morphological type of this pathology with high diagnostic sensitivity.
Keywords: Mirizzi syndrome, Classification, Diagnosis, Computed tomography, Retrograde cholangiopancreatography, Cholecystectomy, Drainage of the common hepatic duct
Cite this paper: Kurbonov Nizom Azizovich, Davlatov Salim Sulaymonovich, Rakhmanov Kosim Erdanovich, Nabiyev Bobir Bakhodirovich, Mirizzi Syndrome: Prediction of Preoperative Diagnosis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 4, 2022, pp. 437-440. doi: 10.5923/j.ajmms.20221204.14.
Article Outline
1. Introduction
- Kehr [1] and Ruge [2] were the first to describe this condition in the early 1900s, although the term “Mirizzi Syndrome” was not adopted until after the work of Mirizzi [3] in 1948. This syndrome is an uncommon complication of chronic gallstone disease. Pathophysiologically, this condition involves extrinsic compression of the bile duct by pressure applied upon it indirectly by an impacted stone in the infundibulum or neck of the gallbladder. In turn, the resulting chronic inflammation and ulceration form varying degrees of cholecystobiliary fistula. Furthermore, cholecystoenteric fistula may also occur [4–7]. Mirizzi syndrome (MS) often manifests itself in an acute form; however, the chronic form is an equally or even more common form of manifestation [5]. Although the clinical manifestations of Mirizzi syndrome are nonspecific, the most common form of clinical manifestations of Mirizzi syndrome is mechanical jaundice (60-100%), accompanied by abdominal pain in the upper right quadrant of the abdomen (50-100%) and fever in a patient with known or suspected cholelithiasis [8,10]. Sometimes a previous recent jaundice may be detected. Often, patients with Mirizzi syndrome are treated against the background of acute cholecystitis, acute cholangitis or acute pancreatitis [8]. Mirizzi syndrome in gallstone intestinal obstruction has recently been described and confirmed as another clinical manifestation that surgeons should keep in mind [9].Preoperative diagnosis of Mirizzi syndrome followed by thoughtful surgical planning is of paramount importance [6]. The frequency of damage to the bile ducts in patients operated with Mirizzi syndrome without preoperative diagnosis can reach 17% [14]. Preoperative diagnosis of Mirizzi syndrome is complex and can be performed only in 8-62.5% of patients [6,9]. If a preoperative diagnosis is not made, it is necessary to identify during surgery and proper treatment. Inadequate recognition of this condition leads to high preoperative morbidity and mortality [12]. The diagnosis of Mirizzi syndrome is based on previously described clinical characteristics and a high index of suspicion or surgical intuition, which can be supplemented with radiological images and endoscopic procedures.The conducted analysis of the literature indicates that at the present time the diagnosis of MS belongs to one of the urgent and still unresolved problems of modern healthcare. In this regard, there is a need to revise the criteria for the radicality of surgical intervention in MS, depending on the informativeness of non-invasive medical imaging methods, which allow at the preoperative stage to assess the features of the clinical course of the disease and identify signs of aggression of the disease, and therefore, optimization of the diagnostic algorithm becomes especially relevant in order to choose the most radical tactics of surgical treatment in each case.The aim of the study was to improve the results of the diagnosis of Mirizzi syndrome by introducing modern research methods.
2. Research Material
- The work is based on the evaluation of the results of surgical treatment of 62 patients with cholelithiasis complicated by Mirizzi syndrome who were hospitalized in surgical departments of the Republican Specialized Scientific and Practical Center for Emergency Medical Care of the Samarkand branch (RSPCEMCSB) for the period from 2016 to 2021.
3. The Results of the Study
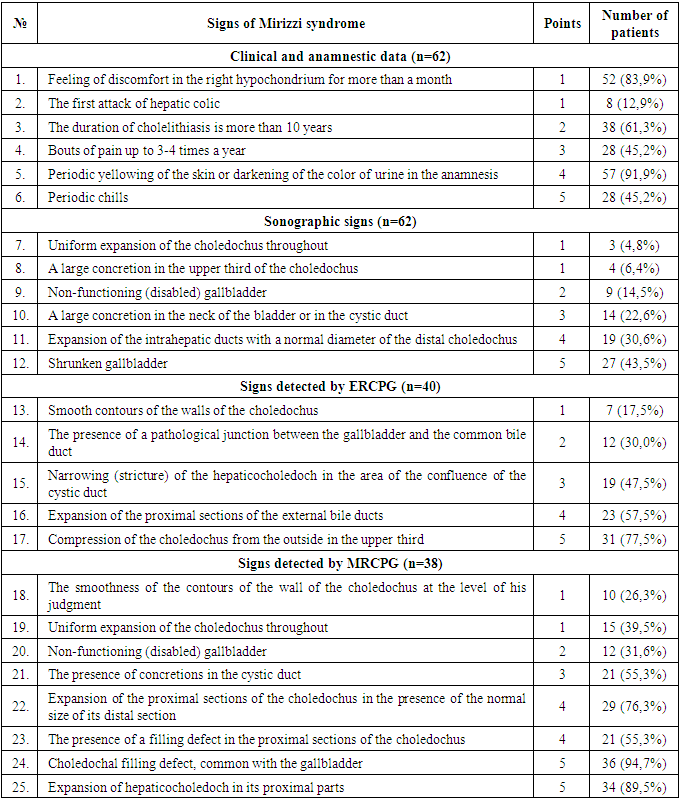
- When examining patients with MS before surgery, 7 patients were faced with the fact that in the presence of signs indicating this complication of the gastrointestinal tract, they were not taken into account by diagnostic doctors and surgeons and the appropriate diagnosis was not made before surgery. It was considered necessary to identify the most important signs in relation to the diagnosis of MS, to calculate their informativeness.We evaluated the informativeness of each feature when MS. To do this, they were grouped together:1. Clinical and anamnestic;2. Sonographic;3. ERCPG information;4. MRCPG information.Among the anamnestic data, the most informative signs were such as a history of cholelithiasis for more than 7 years, bouts of pain up to 3-4 times a year, periodic yellowing of the skin or darkening of the color of urine, a feeling of discomfort in the right hypochondrium for several months, periodic chills.In this connection, based on a review of the literature and our own experience, we have developed a program for scoring the prediction of Mirizzi syndrome in patients with cholelithiasis (Table 1).
|
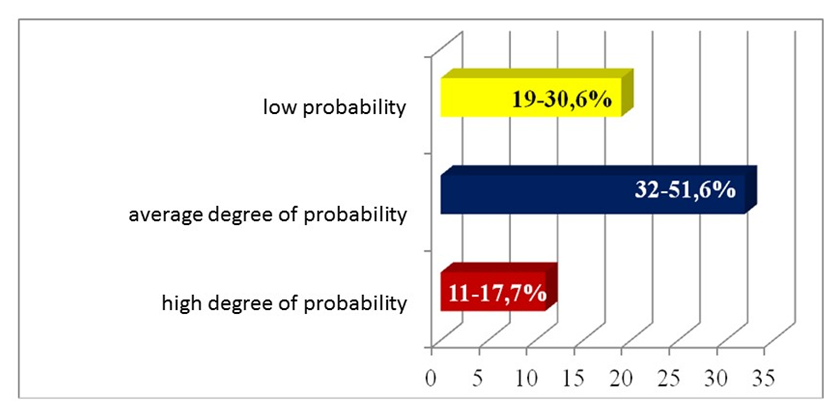 | Figure 1. Distribution of patients in the main group according to the degree of probability of Mirizzi syndrome |
4. Conclusions
- Thus, the information content of ERCPG is higher (58.3%) than ultrasound (43.6%). However, the danger of causing an increase in intra-flow pressure with the introduction of a contrast agent is probably often the reason for the absence of an image of the cholecystocholedocheal fistula and gallbladder. After endoscopic interventions with MS, signs of pancreatitis are possible. In the diagnosis of MS MRCPG turned out to be non-invasive, the effectiveness was 77.8%, i.e. higher than ERCPG and ultrasound. MRCPG is a method that has a higher resolution in the diagnosis of Mirizzi syndrome and allows determining the morphological type of this pathology with high diagnostic sensitivity.
Conflict of Interest
- The authors declare no conflicts of interest or special funding for the current study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML