Kilichev I. A., Adambaev Z. I., Matyokubov M. O., Khudayberganov N. Yu., Niyazmetov M. R.
Urgench Branch of the Tashkent Medical Academy, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The Register of cerebral strokes was carried out in the desert-steppe zones of Uzbekistan on the example of the Khorezm region for 2019. 3569 cases of stroke were identified, of which: 2552 (71.5%) cases were hospitalized, 1350 patients died. The morbidity of stroke, calculated for the entire population of Khorezm region, corresponded to 194.43 cases per 100 thousand, at the age of 20 years and older was 310.32 cases per 100 thousand. Mortality - 73.6 and 117.46 cases per 100 thousand, respectively. Lethality in all types of cerebral stroke was 35.2%. The ratio of ischemic (IS) to hemorrhagic strokes (HS) was 3: 1. Among the main risk factors for the development of stroke, arterial hypertension prevailed in 62.3%, atherosclerosis - in 19.5%, coronary heart disease - in 7.5%, diabetes mellitus - in 3.8%, combined and other risk factors - in 6.9%. Seasonality analysis by types of strokes revealed that IS and HS prevailed in the winter (28.1% and 29.7%) and spring (31.7% and 25.0%), respectively.
Keywords:
Register, Cerebral strokes, Morbidity, Mortality, Lethality, Risk factors, Seasonality
Cite this paper: Kilichev I. A., Adambaev Z. I., Matyokubov M. O., Khudayberganov N. Yu., Niyazmetov M. R., Register of Stroke in Desert-Steppe Zones of Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 12 No. 4, 2022, pp. 412-417. doi: 10.5923/j.ajmms.20221204.09.
1. Introduction
The problem of cerebrovascular disease remains highly relevant due to the high morbidity and mortality, including from acute cerebral stroke [2,7]. Accurate data on the incidence, mortality and risk factors of strokes are essential for the informed deployment of a skilled care network and the successful management of strokes [3,8,16]. The World Health Organization has developed the program "Registry of Cerebral Stroke", which standardizes the diagnostic criteria and research methodology [14]. This program allows, when using it, to obtain the true indicators of morbidity, mortality and lethality from acute cerebral stroke [4,9,17]. Given the urgency of the problem, the aim of the research was: conducting a register of stroke in the desert-steppe zones of Uzbekistan using the example of the Khorezm region.
2. Material and Research Methods
To achieve the set goals, we conducted the "Register of cerebral strokes" of the Khorezm region for 2019. The studies were carried out by a continuous method. All new and repeated cases of stroke that developed during the observation period in residents of the Khorezm region, as well as all cases of death from stroke, were subject to registration. Patients over the age of 20 were examined.Demographic characteristics and features of the structure of the population of the Khorezm region. According to the data of the State Statistics Service of the region, the population was 1,835,690 people as of 01.01.2019, with an equal distribution of the female and male population: 917989 and 917701, respectively. The share of people under the age of 20 was 37.3%. The population of 20 years and older was 1,150,135 people, men - 565,722 people, women - 584,413.
3. Research Results and Discussion
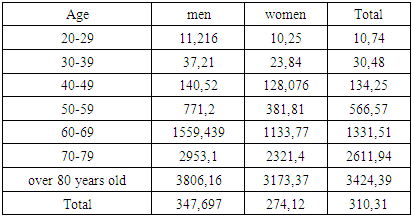
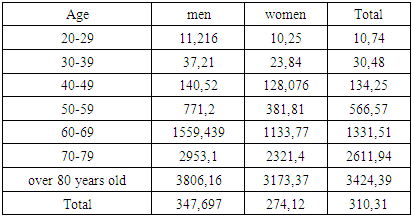
According to the results of the register, 3569 cases of stroke were detected in Khorezm region in 2019, of which: 2552 (71.5%) cases were hospitalized, 1350 patients died.The morbidity of stroke, calculated for the average annual number of permanent residents in Khorezm region at the age of 20 and older, amounted to 310.32 cases per 100 thousand. The morbidity, calculated for the entire population in Khorezm region, corresponded to 194.43 cases per 100 thousand. The morbidity of stroke increased with age, as in men and in women and the maximum values reached in the age group 80 years and older and corresponded to 3806.16 and 3173.37 per 100 thousand population. The morbidity of stroke among men significantly (p <0.05) exceeded the incidence among women: 347.69 and 274.12 cases per 100 thousand, respectively. This trend of prevalence of morbidity among men was also noted in all age groups (Table 1).Table 1. The morbidity of stroke among residents of the Khorezm region over 20 years old, taking into account gender and age (per 100 thousand)
 |
| |
|
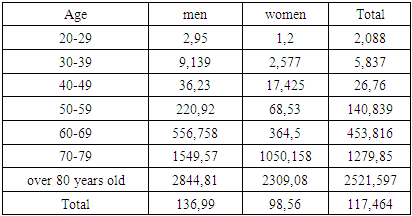
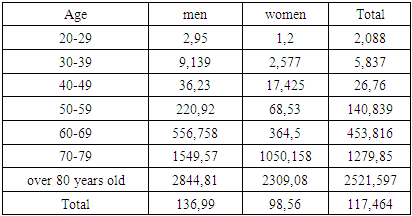
The mortality of stroke was 73.6 cases per 100 thousand for the entire population of the Khorezm region. The mortality for the adult population (20 years and older) was 117.46 cases per 100 thousand. The largest, five-fold increase in the mortality from stroke was observed in the age groups 40-49 and 50-59 years, in relation to the previous age groups. A significant increase in this indicator was noted both among all residents of the Khorezm region and among both sexes, however, in men, a sharp prevalence of mortality begins with the age category 40-49 and 50-59 years, and in women - 40-49 and 60-69 years. Such an increase in mortality in the age group in men can be explained by an additional risk factor in this age group for the development of myocardial infarction, and in women - and increase in mortality in the age group 40-49 years is explained by climacteric age (Table 2).Table 2. The mortality of stroke among residents of the Khorezm region over 20 years old, taking into account gender and age (per 100 thousand)
 |
| |
|
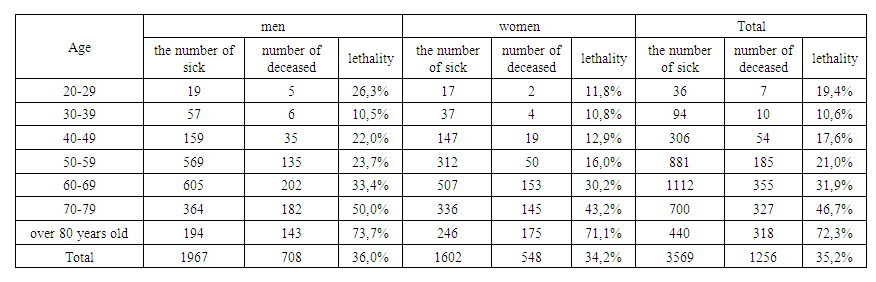
Lethality in all types of stroke was 35.2%. There is an unreliable prevalence of lethality among men (36.0%) over women (34.2%). When analyzing lethality by age groups, it was found that both sexes have a small peak in mortality in the age group 20-29 years old, with a gradual increase in lethality in subsequent age groups, again with a sharp jump in lethality from the age group 70 and older. Lethality in the age group 20-29 years old is due to lethality from subarachnoid hemorrhage (SAH), and in the age group 70 and older - natural causes (Table 3).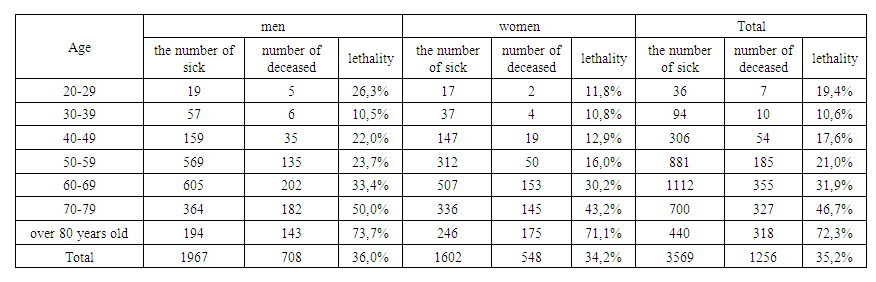 | Table 3. The lethality of stroke among residents of the Khorezm region over 20 years old, taking into account gender and age |
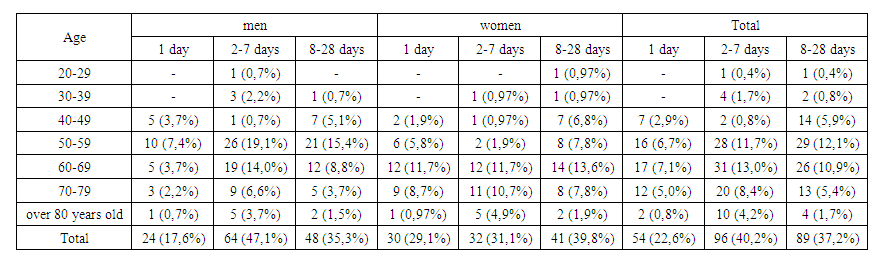
When analyzing the distribution of the timing of death from strokes (in the 1st, up to 7, up to 28 days) in patients who received inpatient treatment, it was revealed that when analyzing both sexes, a large proportion of deaths fall on the periods 2-7 (40.2%) and 8 -28 (37.2%) days. When analyzing the timing of death by sex, it was revealed that in men most of the deaths (47.1%) occur on days 2-7 and in the age group 50-59 (19.1%) and 60-69 (14%) years, and for women (39.8%) - on days 8-28, with a dome-shaped growth in the age groups from 50 to 79 years old with a peak in the age group 60-69 years old - 13.6% (Table 4).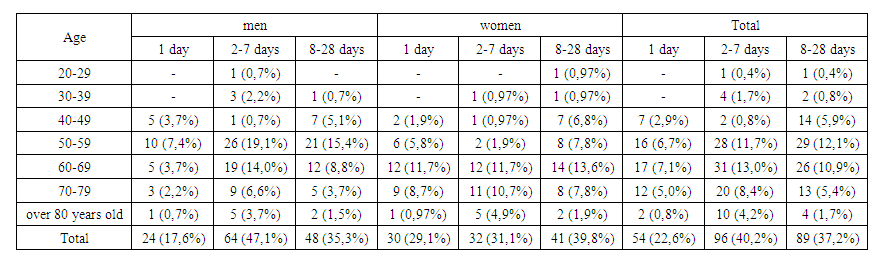 | Table 4. Dates of death from strokes in hospitals of the Khorezm region over 20 years old, taking into account gender and age |
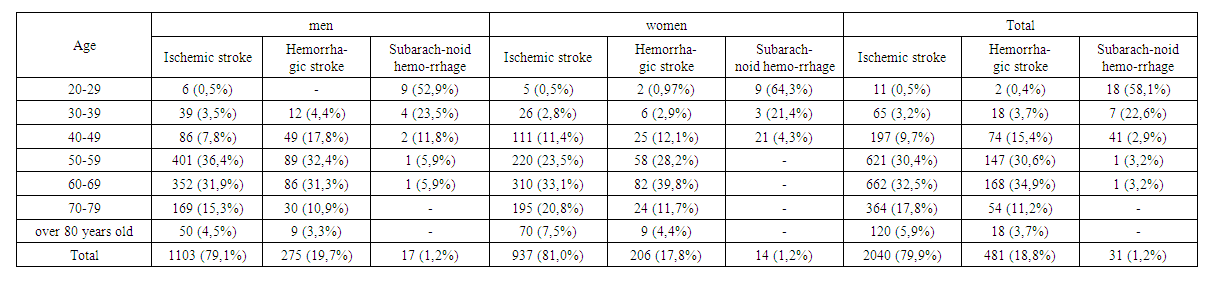
When analyzing the distribution of the timing of death depending on the type of stroke, it was found that in the analysis of both sexes, a large proportion of deaths, both IS and HS, fall on days 2-7 and 8-28. When analyzing the timing of death depending on the type of stroke by gender, it was revealed that in men most of the deaths of both IS and HS occur on days 2-7, and in women, both IS and HS, on days 8-28 (Table 4).In the general structure, IS accounted for 2,193 (61.44%) cases, HS - 676 (18.94%), SAH - 38 (1.1%), undifferentiated stroke - 662 (18.55%). Thus, the ratio of ischemic strokes to hemorrhagic strokes was 3: 1. The indicator is very alarming - the identified strokes of an undetermined type are 18.6%, which directly affects the ratio of ischemic strokes to hemorrhagic strokes obtained by us – 3: 1. This ratio in many population studies is equal to 4: 1 [8,14,17]. The average age of patients with stroke was 63.85 ± 0.2 years, for men - 62.98 ± 0.3 years, for women - 65.1 ± 0.3 years.The structure of strokes in inpatients. Within the framework of the registry of strokes, 2552 patients with strokes were identified who was in the neurological and therapeutic departments of the hospitals of the Khorezm region. Of these, 1395 men (54.7%) prevailed over 1157 women (45.3%). The average age of patients was 60.7 ± 0.2 years, 60.0 ± 0.3 years for men, 61.6 ± 0.4 years for women. Among of strokes, IS accounted for 2040 (79.9%) cases, GS - 481 (18.8%), SAH - 31 (1.2%). The ratio of IS and GS in both women and men was 4: 1. The largest proportion of strokes, both IS and GS, in both men and women, are in the age group 50-59 years old and 60-69 years old. And SAH in both men and women prevails in the age groups of 20-29 and 30-39 years. Significant differences in strokes structure were established among men and women with a predominance of intracranial hemorrhages in men (20.9%), in women (19%). The incidence of cerebral infarction in women was slightly higher (81%) than in men (79.1%). Comparison of the structure of strokes did not reveal statistically significant differences among the male and female populations of the studied region (Table 5). Hemispheric strokes occurred in 99.4%, and stem strokes - in 0.6% of cases. Among hemispheric strokes, localization of the focus in the right hemisphere was found in 47.6%, in the left hemisphere - in 51.8%.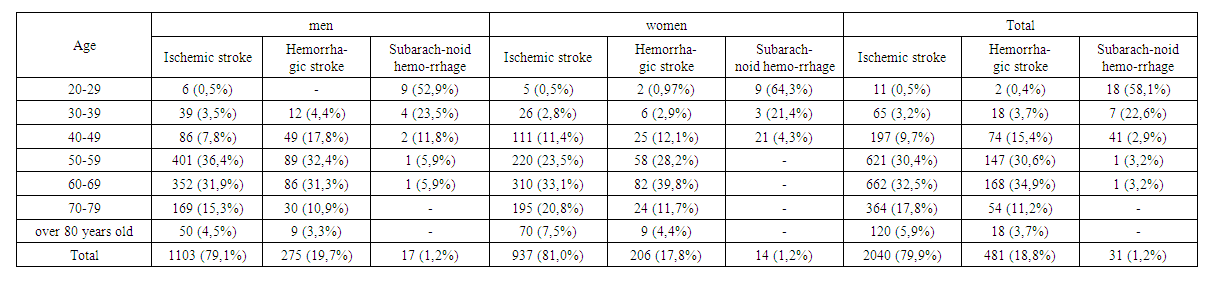 | Table 5. The structure of strokes in inpatients of the Khorezm region over 20 years old, taking into account gender and age |
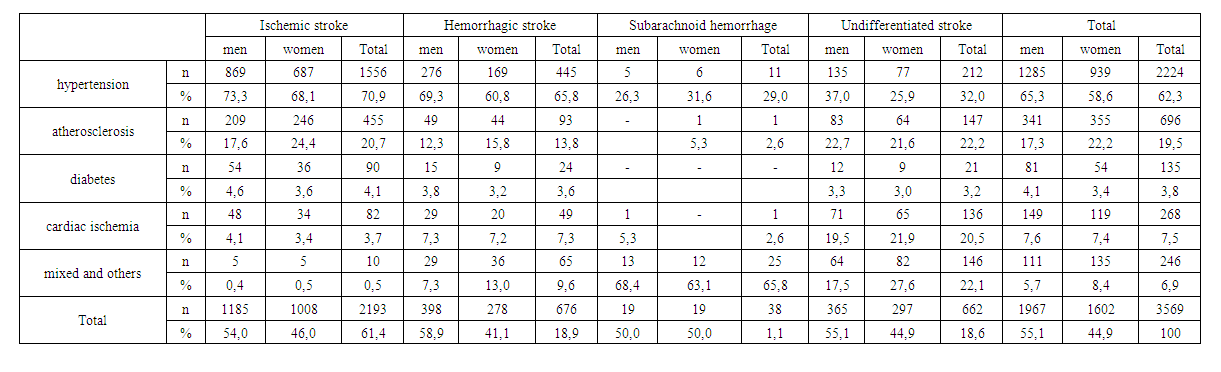
Hospital lethality from strokes. Hospital lethality was 9.36%. Moreover, the highest in-hospital lethality was with HS - 16.2%, then with SAH - 12.9%, and the lowest - with IS - 7.7%. When analyzing hospital lethality by decades, it was found that with IS, it tended to gradually increase from the age group 30-39 to 80 years and older. Moreover, men have small peaks of HS in the age groups 50-59 years old and 80 years old and above, and women have small peaks in the age groups 60-69 and 70-79 years old. With HS, hospital lethality in the age groups of 20-29 and 30-39 years was due to SAH, and with hemispheric hemorrhages, it tended to gradually increase from the age group 40-49 to 80 and older.The main risk factors (RF) of strokes in the desert-steppe zones of Uzbekistan according to the register of 2019.When analyzing the main RFs, it was revealed that among RFs, arterial hypertension (AH) is 62.3%, atherosclerosis (AZ) - 19.5%, coronary heart disease (CHD) - 7.5%, diabetes mellitus (DM) - 3.8%, combined and other FRs - 6.9% (Table 6). This prevalence of hypertension among patients with stroke can be explained by the fact that drinking water in the CW, which is taken from the Amu Darya River and its Shavat channel, due to the environmental disaster in the Aral Sea region, has a high mineralization. In the selected water samples, the mineralization exceeds the maximum permissible concentration (MPC) by 0.36-0.83 times, sulfates exceeds the MPC by 8-10 times [13], which leads to the fact that the population of the region has a very high proportion of gallstone (157.5 per 100,000 population) and urolithiasis (146.2 per 100,000 population), with an increase in kidney diseases among the population (pyelonephritis - 1035, glomerulonephritis - 108.8, diabetic nephropathy - 138.3 per 100,000 population) and, accordingly, hypertension (1610.2 per 100,000 population) [1,12]. The low proportion of AZ and DM among the population is explained by the culinary tradition of the region, where dietary dishes predominate.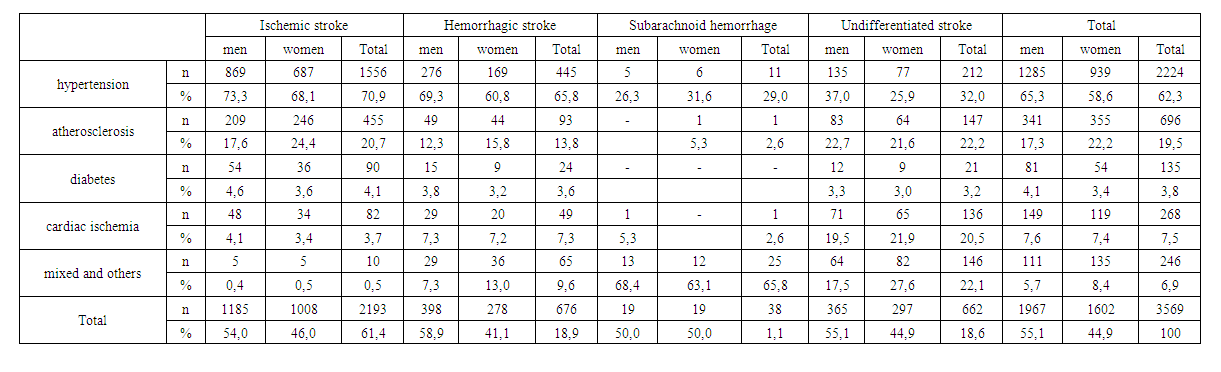 | Table 6. Distribution of risk factors depending on the type of stroke in patients with strokes in the Khorezm region |
In the gender analysis of the main RFs, it was found that RFs such as AH (65.3%), DM (4.1%) and CHD (7.6%) prevail in men, while AZ prevails in women (22.2%) (Table 6).When analyzing RF depending on the type of stroke, it was revealed that with IS and HS, risk factors such as AH and AZ prevail, with a slight prevalence in IS. And with SAH, the risk factors for the development of stroke are hypertension and cerebral aneurysms (Table 6).Seasonality of stroke in the desert-steppe zones of Uzbekistan. According to our study, strokes are recorded throughout the year, but the largest number of strokes developed in the winter (28.0%) and spring (28.6%). Strokes are recorded relatively less frequently in the summer and autumn.When analyzing seasonality by types of strokes, it was revealed that IS and HS also prevailed in the winter (28.1% and 29.7%) and spring (31.7% and 25.0%) months, respectively. SAH predominated in the summer (36.8%) months and autumn (31.6%) months. To identify the reasons for the development of seasonality in different types of strokes, we analyzed the frequency of occurrence of various meteopathic factors by seasons in the desert-steppe zones of Uzbekistan. Apparently, this dynamics is explained by unstable weather in the winter and spring months, when temperature drops during one day (from 6° to 18°С), high humidity is most often noted, and these changes are very sharp. When comparing our data on meteorological factors in the desert-steppe zones of Uzbekistan [5,6,10,11,15,18] by seasons with the medical classification of weather according to V.F. Ovcharova, we found that "spastic" type of weather prevails in winter and spring, "hypoxic" in summer, and "unstable with the transition of the indifferent to the “spastic” type”. In winter and spring, the "spastic" type of weather is a provoking meteorological risk factor for the development of IS and HS. In summer - "hypoxic", and in autumn - "unstable with the transition of indifferent to "spastic" types of weather are provoking meteorological factors for the development of SAH.
4. Conclusions
1. According to the registry of stroke in the desert-steppe zones of Uzbekistan, on the example of the Khorezm region in 2019, among the total population of 1,835,690 people and the population over 20 years old – 1,150,135 people, 3,569 cases of strokes were identified. Of these: 2552 (71.5%) cases were hospitalized, 1350 patients died.2. The average age of patients with stroke was 63.85 ± 0.2 years. For men - 62.9 ± 0.3 years, for women - 65.1 ± 0.3 years.3. The morbidity of stroke was 310.32 cases per 100 thousand for the population over 20 years old and 194.43 cases per 100 thousand of the total population. The morbidity of stroke increased with age and significantly (p <0.05) prevailed among men compared with women: 347.69 and 274.12 cases per 100 thousand, respectively.4. The mortality of strokes was 117.46 cases per 100 thousand of the population over 20 years old and 73.6 cases per 100 thousand of the total population. The largest, five-fold increase in mortality from stroke was observed in the age groups 40-49 and 50-59 years, in relation to the previous age groups.5. Lethality in all types of stroke was 35.2%. There is an unreliable prevalence of lethality among men (36.0%) over women (34.2%). Lethality tends to increase with age, with lethality peaks in the age group 20-29 years, due to lethality from SAH and in the age group 70 and older, due to natural aging of the body. Hospital lethality was 9.36%. Moreover, the highest hospital lethality was in hemorrhagic stroke - 16.2%, then in SAH - 12.9% and the lowest - in ischemic stroke - 7.7%.6. Dates of death from strokes (in the 1st, up to 7, up to 28 days): 40.2% of deaths accounted for the periods of 2-7 days and 37.2% of deaths at 8-28 days.7. The structure of strokes was dominated by ischemic strokes - 61.4%, hemorrhagic - 20% (of which 1.1% - SAH) and indeterminate type - 18.6%. The ratio of ischemic to hemorrhagic strokes was 3: 1. However, the structure of strokes in hospital patients differed: ischemic strokes - 79.9%, Hemorrhagic - 18.8% and SAH 1.2%, and the ratio of ischemic to hemorrhagic strokes was 4: 1.8. Among the main risk factors for the development of strokes, AH prevailed in 62.3%, atherosclerosis - in 19.5%, CHD - in 7.5%, diabetes - in 3.8%, combined and other risk factors - in 6.9 %. In gender analysis, such risk factors as AH (in 65.3%), diabetes (in 4.1%) and coronary artery disease (in 7.6%) prevail in men, while in women, AZ (22.2%) prevails. In IS and HS, risk factors such as AH and AZ prevail, with a slight prevalence in IS. And with SAH risk factors of stroke development are cerebral aneurysms and hypertension.9. When studying the seasonality of strokes, the prevalence was revealed in the winter (28.0%) and spring (28.6%). In winter and spring, the "spastic" type of weather is a provoking meteorological risk factor for the development of IS and HS. In summer - "hypoxic", and in autumn - "unstable with the transition of indifferent to" spastic "types of weather are provoking meteorological factors for the development of SAH.
ACKNOWLEDGEMENTS
The authors are grateful to: Professor Kilichev I.A. in the organization and control of the Register of cerebral strokes in the desert-steppe zones of Uzbekistan, employees of the Department of Neurology and Psychiatry of the Urgench branch of the Tashkent Medical Academy for conducting the Register of cerebral strokes; Adambaev Z.I. in the analysis of the obtained data from the Register of Cerebral Strokes and in the writing of the article. The authors declare that they have no conflicts of interest when writing this article. The publication is funded from its own funds.
References
| [1] | Abdrimov Zh.A. Health Department of the Khorezm region. Report Form 12, 2019. |
| [2] | Adogu P. O. U., Ubajaka C. F., Emelumadu O. F., Alutu C. O. C. Epidemiologic Transition of Diseases and Health-Related Events in Developing Countries: A Review. American Journal of Medicine and Medical Sciences. 2015; 5(4): 150–157. |
| [3] | Akpanova D.M., Berkinbaev S.F., Musagalieva A.T. et al. Features of the clinical and demographic characteristics of patients with strokes and concomitant atrial fibrillation / Cardiology. 2018; 58 (S9): 48-57. |
| [4] | Auer P. L., Nalls M., Meschia J. F., et al. Rare and coding region genetic variants associated with risk of ischemic stroke: The NHLBI Exome Sequence Project. JAMA Neurology. 2015; 72(7): 781–788. |
| [5] | Dolgusheva, Yu.A. Results of a retrospective multidisciplinary study of the peculiarities of the influence of heliogeophysical activity on mortality from stroke (according to data from Rostov-on-Don and Ulan Bator) // Bulletin of Neurology, Psychiatry and Neurosurgery. – 2017; 8: 51-56. |
| [6] | Dolgusheva, Yu.A. The role and significance of heliogeomagnetic activity in the genesis of the development of cerebral stroke / Yu. A. Dolgusheva // Handbook of a general practitioner. – 2017; 1: 23-28. |
| [7] | Eric S. Doncor Stroke in the 21st Century: A Snapshot of the Burden, Epidemiology, and Quality of Life / Stroke Res Treat 2018; 3238165. doi: 10.1155/2018/3238165. |
| [8] | Feigin V.L., Norrving B., George M.G., Foltz J.L., Roth G.A., Mensah G.A. Prevention of stroke: A strategic global imperative. Nature Reviews Neurology. 2016; 12(9): 501–512. doi: 10.1038/nrneurol.2016.107. |
| [9] | GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and causespecific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388 (10053): 1459–544. DOI:10.1016/S0140–6736 (16) 31012–1. |
| [10] | Grigoriev K.I., Povazhnaya E.L. Methods of medical weather forecasts 50 years old / ISSUES OF RESORTOLOGY, PHYSIOTHERAPY AND THERAPEUTIC PHYSICAL CULTURE 2014; 1: 57-62. |
| [11] | Kilichev I.A. “Brain strokes in different climatic regions of Uzbekistan. Development of weather forecasting and meteorological prevention”. Dis. d.m.s. 1999, - 245 p. |
| [12] | Kilichev I.A., Khudaibergenov N.Yu., Adambaev Z.I. Cerebrovascular diseases in the Aral Sea region. Lambert Academic Publishing, Riga, Latviya, 2018, 70 p. |
| [13] | Mambetkarimov G.A., Zhiemuratova G.K., Utemuratov K.S. The role of the water factor in the Aral Sea region in the formation of children's health / Bulletin of Science and Practice, 2016; 6: 85-89. |
| [14] | Narayanaswamy Venketasubramanian, Byung Woo Yoon, Jeyaraj Pandian, Jose C. Navarro Stroke Epidemiology in South, East, and South-East Asia: A Review / Journal of Stroke 2017; 19(3): 286-294. DOI: https://doi.org/10.5853/jos.2017.00234. |
| [15] | Ovcharova V.F. Homeokinesis in weather hypoxia and hyperoxia. Tr. Int. WMO / WHO / UNEP Symposium “Climate and Human Health”. - L.: Gidrometeoizdat, 1988; 142-149. |
| [16] | Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. Journal of the American College of Cardiology. 2017; 70 (1): 1–25. DOI:10.1016/j. jacc. 2017.04.052 |
| [17] | Stakhovskaya L.V., Klochikhina O.A., Bogatyreva M.D., Kovalenko V.V. Epidemiology of stroke in Russia according to the results of the territorial population register (2009-2010). Journal of Neurology and Psychiatry. S.S. Korsakov. 2013; 5: 4-10. |
| [18] | Uyanaeva A.I., Tupitsyna Yu.Yu., Rassulova M.A. and others. Influence of climate and weather on the mechanisms of formation of increased meteosensitivity (review) / ISSUES OF RESORTOLOGY, PHYSIOTHERAPY AND THERAPEUTIC PHYSICAL CULTURE 2016; 5: 52-57. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML