-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(4): 404-411
doi:10.5923/j.ajmms.20221204.08
Received: Mar. 27, 2022; Accepted: Apr. 15, 2022; Published: Apr. 16, 2022

Back Pain in the Elderly: Diagnosis and Treatment Approaches
Adambaev Z. I.1, Kilichev I. A.1, Boltayeva Z. O.2, Khudoibergenov N. Yu.1, Niyazmetov M. R.1
1Department of Neurology and Psychiatry, Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan
2Neurologist, Sanatorium "Urgench" for the Elderly and Disabled, Veterans of War and Labor, Uzbekistan
Correspondence to: Adambaev Z. I., Department of Neurology and Psychiatry, Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan.
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article provides information about back pain in common pathologies in the elderly. These diseases that cause back pain are described separately and divided into three groups: degenerative-dystrophic diseases of the spine, other diseases of the spine, diseases of the internal organs with reflected pain in the spine. 120 elderly patients with degenerative-dystrophic diseases of the spine (DDSD) were examined and treated. Based on the CT and/or MRI examination of the spine, the patients were divided into groups with full, limited or minimal sanatorium treatment regimens. A differentiated approach to the treatment of elderly patients with DDSD with dorsopathy based on neuroimaging diagnostics showed effectiveness in 95% of cases with no complications.
Keywords: Back pain, Dorsopathy, Degenerative-dystrophic diseases of the spine, The elderly, Clinic, Diagnostics, Magnetic resonance imaging, Sanatorium treatment, Physiotherapy
Cite this paper: Adambaev Z. I., Kilichev I. A., Boltayeva Z. O., Khudoibergenov N. Yu., Niyazmetov M. R., Back Pain in the Elderly: Diagnosis and Treatment Approaches, American Journal of Medicine and Medical Sciences, Vol. 12 No. 4, 2022, pp. 404-411. doi: 10.5923/j.ajmms.20221204.08.
1. Introduction
- The growth of economic development of countries with an improvement in the quality of life of the population leads to a gradual increase in life expectancy and, consequently, to its aging. If in 1950 worldwide, according to the Demographic Division of the UN Department of Economic and Social Affairs, there were 188 million people aged 60 and over, then by 2000 this figure increased to 585 million. Approximately every tenth - twelve inhabitant of the planet is an elderly (from 60 to 74 years old) or senile (from 75 to 89 years old) age [1]. A similar trend can be traced in Uzbekistan. According to the State Committee of the Republic of Uzbekistan on Statistics, as of January 1, 2020, the share of people of retirement age accounted for a little more than 10% of the population of Uzbekistan, namely 3.56 million people (1.26 million men and 2.3 million women) [2].Back pain is a common complaint in the elderly. It is associated with degenerative diseases of the spine, occurs during life in 80% of the population, and in old age, pain is experienced by almost all inhabitants of the planet [3].The largest part of mechanical pain episodes in the back in elderly patients is due to musculo-ligamentous dysfunction, somewhat less often - degenerative lesions of the spine (spondylosis, osteoarthritis of the facet joints), herniated disc, non-traumatic osteoporetic compression of the vertebrae, spinal stenosis, spondylolisthesis.Spondyloarthrosis is the cause of dorsalgia in 80% of people over 65 and in 50% of the population over 50 [4], and is also the cause of dorsalgia at the lumbar level in 30–60% of cases, at the cervical level - in 49–60%, and at the chest level - in 42–48% of cases [5].The mechanism of occurrence of dorsalgia in spondyloarthritis, some researchers explain many years of repetitive microtraumatization and increased load on degeneratively altered intervertebral discs. Gradually, the loads from the disc are transferred to the joints, leading to erosions, cartilage destruction, further to periarticular fibrosis, the formation of osteophytes and, as a result, to significant degeneration and almost complete loss of cartilage [6].Pain that occurs with spondylarthrosis is an example of nociceptive pain - due to direct mechanical irritation of the nociceptors of the joint capsule. Dorsalgia in spondylarthrosis in most cases is diffuse in nature, have a moderate intensity. Patients describe this pain as "aching", "pressing", "squeezing", "deep", "twisting". Characterized by the phenomenon of "morning stiffness" and the maximum severity of pain in the morning (signs reflecting the inflammatory component), as well as after exercise at the end of the day.A distinctive feature of dorsalgia in spondyloarthrosis at the lumbar level is an increase in pain during back extension of the trunk and rotation of the trunk (rotation in the lumbar spine). Pain is projected over the affected joint. Pain in spondylarthrosis in the lumbar region radiates to the buttock, coccyx, hip joint, upper thigh, sometimes to the inguinal region; more often bilateral; in the cervical region - in the occipital region, in the shoulder, suprascapular and scapular regions. With the localization of the facet syndrome of the intervertebral joint C2-C3 - pain spreads from the upper cervical region to the occipital region, to the eye region, face, temporal region. Pain in spondylarthrosis of the thoracic spine is localized in the thoracic region in the paravertebral region. May spread to the intercostal area. The appearance of short-term morning stiffness is typical, and exercises on the spine bring relief [7].A neurological examination of the patient does not reveal symptoms of a violation in the motor and sensitive areas, no pronounced symptoms of tension (Lasega, Matskevich, Wasserman) are detected. Vertebral examination reveals smoothness of the lumbar lordosis, increased kyphosis in the thoracic region, and possible scoliosis in the thoracic and lumbar regions. Local tenderness is determined on palpation in the projection of the “problem” facet joint, tension of the paravertebral and square muscles of the back, discomfort and limited range of motion when bending back are detected [8].Hernias of intervertebral disks. The most common cause of low back pain is a herniated disc [9]. In the elderly, with age, the nucleus pulposus of the disc loses elasticity and, against the background of age-related degenerative changes, can lead to protrusion (prolapse), and if the fibrous ring is ruptured, to a hernia. A herniated disc within the spinal canal can cause compression of the nerve roots and spinal cord, causing back and limb pain (compression mechanism). The substance of the nucleus pulposus, being a chemical irritant for the nervous tissue, contributes to the occurrence of a local inflammatory reaction, edema, and microcirculatory disorders. This causes local irritation of sensitive receptors and muscle spasm, leading to limited mobility in the affected area (reflex mechanism). The prolonged existence of spasm leads to a violation of posture, the development of a pathological motor stereotype and maintains pain. Thus, reflex muscle tension initially has a protective character, since it leads to immobilization of the affected segment, but later becomes a factor that additionally provokes pain (“vicious circle”: pain–spasm–pain) [10].The main diagnostic criteria for a herniated disc are:• the presence of vertebrogenic syndrome, manifested by pain, limited mobility and deformities (antalgic scoliosis) in the affected spine;• tonic tension of paravertebral muscles;• sensory disorders in the area of the neurometamer of the affected root;• movement disorders in the muscles innervated by the affected root;• decrease or loss of reflexes;• the presence of relatively deep biomechanical disturbances in the compensation of the motor act;• data from computed tomography (CT), magnetic resonance imaging (MRI) or radiographic examination, verifying the pathology of the intervertebral disc, spinal canal and intervertebral foramina; data of an electroneurophysiological study (F-wave, H-reflex, somatosensory evoked potentials, transcranial magnetic stimulation), recording a violation of the conduction along the root, as well as the results of needle electromyography with an analysis of the action potentials of motor units, which make it possible to establish the presence of denervation changes in the muscles of the affected myotome.Vertebral osteoporosis. Many authors, when considering the problem of back pain, point to osteoporosis of the spine as its possible cause. However, osteoporosis of the vertebrae, not accompanied by fractures, is not a source of pain [11]. Neurological manifestations in osteoporosis of the spine occur only with a fracture of one or more vertebrae and gradually increasing deformation of the spinal column or individual vertebrae (“fish vertebrae”, vertebrae in the form of a coil, wedge-shaped deformity of the vertebrae), a violation of the statics of the spine with the development of kyphosis or kyphoscoliosis. The sources of back pain are: a damaged deformed vertebra, spasmodic muscles surrounding it, periarticular tissues, intervertebral joints, ligamentous apparatus of the spinal segment, etc. Pain may be associated with irritation of pain receptors in the periosteum of the vertebrae, capsules of the facet joints, posterior longitudinal, yellow, interspinous ligaments, the outer third of the fibrous ring of the intervertebral discs, the dura mater, epidural fatty tissue, the walls of arterioles and veins [12].Vertebral compression fractures in osteoporosis in the elderly are most common in women who have developed postmenopausal osteoporosis and have the following clinical features [11]:• arise as a result of a compression load (lifting a load, changing the position of the body);• suffer from vertebrae experiencing the greatest axial load (lower thoracic and upper lumbar vertebrae);• pain can radiate to the chest, abdominal cavity with a sharp limitation of movements; when the fracture is localized in the 1st lumbar vertebra, the pain may radiate to the iliac crests and thighs;• pain syndrome lasts 1-2 weeks, then gradually subsides within 2-3 months.The following signs may indicate the presence of an osteoporotic fracture of the vertebra:• decrease in height by 2 cm or more over 1–3 years of follow-up and by 4 cm compared with growth at 25 years old - a reason for performing x-rays spine to detect vertebral fractures (GR: B);• increased thoracic kyphosis (B);• decrease in the distance between the ribs and the iliac crest - less than the width of 2 fingers (B);• the appearance of the distance from the back of the patient's head to the wall in the standing position (B);• tooth loss < 20 and weight loss < 51 kg (C).If a compression fracture is suspected, an X-ray of the spine is performed in frontal and lateral projections. Mandatory methods for the differential diagnosis of osteoporosis with metabolic diseases of the skeleton include determining the levels of total calcium and phosphorus in the blood serum, calcium in the morning portion of urine as a marker of bone resorption, daily excretion of calcium in the urine to assess calcium absorption in the intestine, total alkaline phosphatase activity as a marker of osteoblastic function, parathyroid hormone, creatinine and thyroid-stimulating hormone clearance in women, testosterone in men, and vitamin 25(OH)D3 content.Spinal stenosis. Most often, spinal canal stenosis is formed against the background of growth of the marginal surface of the facet joints, protrusions and herniations of the intervertebral discs, posterior osteophytes, spondylolisthesis, and yellow ligament hypertrophy [13]. Post-traumatic stenosis occurs as a result of an undiagnosed vertebral fracture with deformation and narrowing of the spinal canal against the background of instability and cicatricial changes in the epidural space. Lumbar stenosis, as a rule, manifests as aching pain in the legs, aggravated at the beginning of walking and relieved when it is stopped, as well as when sitting, bending forward (intermittent neurogenic claudication). When combined with congenital narrowing of the channel, the symptoms may increase with extension. At rest, a neurological examination does not reveal abnormalities, but immediately after exercise, weakness in the lower extremities, decreased reflexes, and sensitivity disorder are determined [14].Degenerative spondylolisthesis. There are 2 variants of degenerative spondylolisthesis: simple, or degenerative without spondylolysis (non-lytic or arthrogenic), and spondylolysis, which is also called discogenic. lolis, which is also called discogenic. There is both a single spondylolisthesis and multiple - "ladder degenerative spondylolisthesis." Pain in the back and posterior thigh that occurs after rising from a sitting or lying position is typical of spondylolisthesis at the LV–SI level, but may be a symptom of segmental instability in the lumbar spine [15].An objective examination of the stepwise displacement of the spinal process may be the key to the diagnosis of spondylolisthesis, localized 1 segment below the level of displacement. Spondylolisthesis is visualized when performing radiography in the lateral projection. X-rays with functional tests (flexion, extension) may be useful in diagnosing mild lesions and spinal instability (spondylolitic instability).Myofascial pain syndrome in the paravertebral muscles develops more often against the background of osteochondrosis, but occasionally on its own (with chronic microtraumatization, overstretching or compression of the muscles during injury and prolonged immobilization). Myofascial pain is manifested by muscle tension and the presence of trigger points in them. There are no symptoms of damage to the peripheral nervous system, except for those cases when tense muscles compress the nerve trunk [16].Other diseases of the spineDegenerative-dystrophic diseases of the spine in the elderly must be differentiated from tumors and infectious diseases of the spine. The following are the main clinical signs or "red flags" to suspect these conditions:• fever (characteristic of a cancerous lesion, vertebral osteomyelitis, disc infection, sepsis, tuberculosis);• weight loss (malignant tumors);• inability to find a comfortable position (metastases, as well as aortic aneurysm, urolithiasis);• night pains (tumors, metastases);• intense local pain (erosive process);• inefficiency of analgesic therapy.Tumors of the spine are primary and metastatic. Primary tumors include chordoma, hemangioma, and osteosarcoma. Among all cases of metastatic lesions of the spine, the cervical region is involved in the pathological process in 10% of cases, the thoracic region in 70%, and the lumbar region in 20%. Most often, breast cancer, prostate cancer, and lung cancer metastasize to the spine, and somewhat less frequently, melanoma, kidney cancer, and thyroid cancer [17].Tumors of the spine may manifest as the only clinical symptom in the form of back pain. The pain does not go away at rest, worse at night and with percussion. Tumors of the spinal canal are characterized by acute pain of the radicular type [16].Myeloma. Damage to the spine is also observed in multiple myeloma, in which flat bones (skull, pelvis, sternum, ribs) are also affected. It belongs to the group of paraproteinemic hemoblastoses, characterized by the proliferation of plasma cells with hyperproduction of monoclonal antibodies. With multiple myeloma, osteodestruction and osteoporosis of the spine are detected. The lumbosacral spine is more often affected; constant intense pain in the back and chest is characteristic, subsiding in the supine position (in contrast to pain in metastatic lesions). The presence of an M-gradient in the electrophoregram of blood serum proteins and / or the detection of Bence-Jones protein in the urine play a decisive role in making a diagnosis. The disease is characterized by a sharp increase in the level of total protein in the blood serum, persistent proteinuria, a persistent and prolonged increase in the erythrocyte sedimentation rate (ESR), hypercalcemia, hypogammaglobulinemia, plasma cell infiltration of the bone marrow (the number of plasma cells reaches > 15%) [18].Among infectious lesions of the spine in the elderly, osteomyelitis of the vertebrae, discitis and tuberculous spondylitis are distinguished. They can develop as a result of hematogenous spread of infection from skin lesions, genitourinary, gastrointestinal, respiratory tracts. Predisposing factors for the development of infectious lesions of the spine are long-term immunosuppressive therapy, alcoholism, diabetes mellitus and other comorbid conditions. In tuberculosis, the lumbar region is involved in 30% of cases. Destruction of 2 adjacent vertebrae (anterior wedge-shaped deformity) is characteristic. Back pain in osteomyelitis is intense, in 15% of cases it occurs with symptoms of radicular or spinal compression. Fever occurs in 50% of cases. X-rays are shown computed tomography (CT) and MRI combined [16].In somatic diseases (gastric ulcer, pancreatitis, pyelonephritis, etc.), referred back pain is usually local in nature, combined with other manifestations of the disease, accompanied by tension in the back muscles, not associated with movements in the spine; typical zones of irritation and repercussion are revealed in the form of hyperesthesia zones (Zakharyin–Ged zones) [16].Gynecological diseases: uterine prolapse, fibroids, endometritis, adnexitis, uterine cancer, endometriosis, pelvic varicose veins, menstrual pain and even pregnancy are the most common source of chronic lumbodynia in women. In these conditions, pain of moderate intensity is more often localized in the sacrum and increases with prolonged standing. In men, diseases of the prostate gland, including chronic prostatitis, can lead to the appearance of such lumbar pain [16].Insufficient content of magnesium in the body can be manifested by pain in the back, increased muscle tone, leg cramps and paresthesia. The appearance of such neuromuscular signs as paresthesia - a burning sensation and tingling, "goosebumps", coldness; restless legs syndrome, muscle contractures, cramps in the calf muscles - cramps, urination disorders (frequent urges, pain in the bladder area); shooting and aching pains in the lower back, other unpleasant sensations that do not have a clear anatomical distribution and objective confirmation are also associated with magnesium deficiency. In the elderly in such situations, it is important to determine the concentration of magnesium in the blood serum [19].Psychogenic back pain.Low back pain in the absence of significant deviations in the somatic and neuroorthopedic status is quite often a mask of depression [17].Pain syndrome within the framework of depression is characterized by the following features:• the clinical picture of the pain syndrome does not fit into any of the known somatic or neurological diseases;• repeated diagnostic studies do not reveal a current organic disease that could explain the pain syndrome;• the duration of the pain syndrome is at least 3 months, the pain history is typical;• senestopathic coloration of pain - burning, "goosebumps", a feeling of cold, "crawling and stirring under the skin"; often the pain is described in "non-painful terms": "heaviness", "woolness", etc.;• active questioning reveals multiple pain syndromes that often change their localization;• characteristic pain behavior with a tendency to spare the "sick organ";• the presence of a characteristic syndromic environment: symptoms of a depressive circle, polysystemic vegetative symptoms.Fibromyalgia is a chronic disease characterized by pain, stiffness, and soreness in the muscles, tendons, and joints. Fibromyalgia pain is most common in the neck, shoulders, chest, upper torso, and buttocks. In addition, sensitive zones are identified - these are limited areas where there is increased sensitivity. Fibromyalgia is also characterized by sleep disturbance, chronic fatigue, depression, anxiety, and bowel dysfunction. Emotional disorders, poor concentration, impaired fixation memory, irritability occur in more than half of patients with fibromyalgia. Fibromyalgia affects mainly women (up to 80% of women are ill) aged 35 to 55 years, much less often - men, children and the elderly. The cause of occurrence is still unknown. There are no tests or x-rays to support a diagnosis of fibromyalgia. Tests and examinations are prescribed to rule out other diseases. Fibromyalgia is diagnosed based on the history of the disease and physical examination data - detection of tender points, nodules (up to 80% of cases) on palpation, located in the region of the trapezius muscles, posterior cervical muscles and in the upper sections of the gluteal muscles and with the exclusion of other diseases [20].Thus, back pain in the elderly has a diverse character, the diseases leading to them can be conditionally divided into three large groups: a) degenerative-dystrophic diseases of the spine, b) other diseases of the spine, c) diseases of the internal organs with reflected pain in the spine. Difficulties in differential diagnosis between these nosologies are also associated with the fact that in the elderly there is a blurring of symptoms and a chronic pain syndrome, a layering of comorbid diseases, along with an increasing development of cognitive and dementia disorders in this age group of patients, complicating the subjectivization of pain syndrome assessment.The treatment of back pain is based on the principles of evidence-based medicine. The effectiveness of non-steroidal anti-inflammatory drugs has a high degree of evidence. The doctor must always remember that the treatment of back pain in the elderly, who very often have comorbidities, should be especially differentiated and sparing, giving preference to cyclooxygenase-2 (COX-2) preparations. The duration of admission is, as a rule, on average, from 7 to 14 days [21,22,23].An important step in the relief of muscle spasm that accompanies pain is the appointment of muscle relaxants. They reduce pain, reduce reflex muscle tension, improve motor functions, which allows more active rehabilitation measures, including physiotherapy exercises. Therapy with muscle relaxants in elderly patients begins with the usual dose (in malnourished patients, the dose can be reduced by 1/2 or 1/3) and continue from several days to several weeks during the entire period of the pain syndrome [21].Pathogenetic therapy for degenerative-dystrophic processes in the joints of the spine is the long-term administration of chondroprotectors [24].To enhance the therapeutic effect, patients with dorsalgia add physiotherapy aimed at reducing reflex muscle spasm, reducing root compression, and improving microcirculation. However, for the treatment of back pain in the elderly with comorbid diseases, only gentle physiotherapy can be used, which include traction of the spine with light weight (in the absence of osteophytes), phonophoresis with papaya melon tree preparations, magnetotherapy (in the absence of a pacemaker in the heart)), massage and exercise therapy [25,26].The appointment or exclusion of methods of therapeutic intervention in the program of sanatorium treatment in patients with manifestations of DDSD, detected during a comprehensive X-ray study, is influenced by [27]:- the presence of a decrease in the mineral density of the bone structure (the exclusion of vertical and the appointment of horizontal underwater traction, the appointment of kinesitherapy);- the presence of spondylolisthesis of the 1st degree with a violation of the stability of the Spinal motion segment (SMS) (the exclusion of Charcot's shower, traction therapy, the appointment of detenser therapy, restrictions on manual exposure, the appointment of kinesitherapy on a passive suspension system);- the presence of hemangiomas (excluding acupuncture, heat therapy, hydrogen sulfide baths; the appointment of iodine-bromine baths and transcranial electroanalgesia);- the presence and severity of osteoarthritis and spondylosis (the appointment of pelotherapy or hydrogen sulfide baths; the choice of methods of apparatus physiotherapy);- the nature of the narrowing of the radicular holes (the choice of methods of hardware physiotherapy).In the complex treatment of dorsopathies, sanatorium treatment is carried out in the chronic stage of the disease without exacerbation of the pathological process [28,29]. The main role of the sanatorium-and-spa treatment of dorsopathy is to minimize neurological manifestations, reduce pain, reduce the severity of structural changes, improve the functional and psychological state of patients and improve the quality of life of patients, which makes it possible to achieve long-term remission, and the medical base of the sanatorium provides great opportunities in compiling individualized treatment programs [29,30,31]. In dorsopathies, there is often a discrepancy between radiologically detected anatomical disorders and clinical and neurological symptoms, which requires a comprehensive diagnosis and, based on their choice, individualized treatment programs [32].There are specific restrictions and contraindications in the appointment of methods of sanatorium treatment, due to the mechanisms of action of therapeutic factors and their therapeutic effects. For example, traction treatment is one of the methods of pathogenetic therapy of osteochondrosis of the spine, but for its implementation it is necessary to additionally clarify the state of the spinal motion segments (SMS), since the presence of sequestered disc herniation, massive extrusion, SMS instability and severe spondylolisthesis, spinal neoplasms, pronounced manifestations osteoarthrosis of the joints of the spine and spondylosis, stenosis of the spinal canal, disorders of bone tissue mineralization in the form of osteoporosis is an absolute contraindication to this type of treatment [29,33]. The same can be said about the appointment of manual therapy, which is also one of the most commonly used and effective types of physiotherapy and spa treatment of degenerative-dystrophic diseases of the spine (DDSD), but also has a number of contraindications and limitations to the use of its various methods, and the correct prescription of manual actions requires not only a high qualification of a specialist, but also the availability of information about structural and functional changes in the spine in the area of medical manipulations [34,35].Thus, in the complex treatment of elderly and senile patients with dorsalgia, they have their own characteristics in the form of the presence of comorbid diseases, neuroimaging features of DDSD, a decrease in regenerative processes, a decrease in the plasticity of the nervous system, chronic pain syndrome, as well as the appointment of drugs and physiotherapy, which gentle effect.The aim of the study was to evaluate the effectiveness of differentiated complex (drug and sanatorium) treatment in the elderly with dorsalgia.
2. Materials and Methods
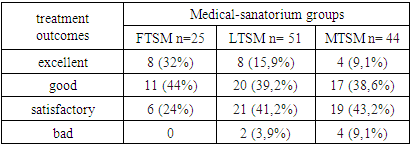
- The results of observation of 120 elderly patients who received sanatorium treatment in the «Urgench» sanatorium during 2020-21, aged 60-74 years, were analyzed, including 71 women, 49 men. All patients underwent neurological examination, X-ray, CT or MRI of the spine. Pain syndrome was determined using a 10-point visual analogue scale (VAS).All radiological studies were carried out to determine the indications for excluding contraindications to the appointment of methods and techniques of sanatorium treatment, to assess the severity of manifestations of DDSD in order to determine the regimen of the intensity of therapeutic effects and to select the most appropriate and effective schemes for sanatorium treatment.Changes in the intervertebral discs (IVD) were assessed: a decrease in height, a change in structure, localization, size and prevalence of protrusions and extrusions; presence of signs of IVD sequestration, assessment of the width and narrowing of the spinal canal, lateral and root canals by intervertebral disc prolapses; changes in bone structures: decreased density and mineralization; the presence of osteophytes, their severity and prevalence; the presence and severity of osteoarthritis; the presence of degenerative stenosis of the spinal canal; narrowing of the root foramens due to osteophytes; calcification of the fibrous ring of the disc; changes in the ligaments of the spine (hypertrophy and calcification).For practical convenience and expediency, we have divided the range of sanatorium treatment for the elderly with dorsalgia into the following categories:Full treatment-sanatorium mode (FTSM): this is a sanatorium mode of maximum intensity of therapeutic effect. In patients, according to the data of radiation studies, minimal and mild manifestations of DDSD are revealed, there are no absolute contraindications to the appointment of a full range of methods and techniques of therapeutic effects available in the sanatorium. In this mode, the appointment of methods of mechanotherapeutic and manual effects of maximum intensity in combination with various preformed physical factors and methods of balneo- and hydrotherapy is noted; exercise therapy in general groups for patients with diseases of the organs of support and movement and in most cases were combined with mechanokinesotherapy on simulators.Limited treatment-sanatorium mode (LTSM): this is a sanatorium mode of limited intensity of therapeutic effects. According to radiological studies, patients have manifestations of DDSD or other conditions of the spine, which are relative contraindications and limitations to the appointment of a full range of therapeutic methods. Compared with the previous group, the use of mechanotherapeutic and manual effects was limited in these patients, the dosages of the procedures used were reduced, their intensity was reduced, and they were alternated instead of jointly prescribed to prevent deterioration of the general condition and reduce adaptive capabilities instead of the expected improvement. Therapy exercises in these patients were carried out in the general group in a mode of moderate intensity, due to the presence of morphological changes in the radiation pattern, which limit the tolerance of functional loads from the spine.Minimal treatment-sanatorium mode (MTSM): a sanatorium mode of minimal intensity of therapeutic exposure in patients due to the presence of various combinations of pronounced and pronounced degenerative changes according to radiation studies, which lead to a significant number of contraindications to the appointment of various methods and techniques of sanatorium treatment. At the same time, the appointment of horizontal and vertical underwater traction of the spine (traction therapy), manual and mechanokinesotherapy was excluded, and exercise therapy was prescribed in individual groups, and some physiotherapy in the most gentle mode.Depending on the identified neuroimaging characteristics of DDSD, we divided the patients into 3 treatment and sanatorium groups: there were 25 patients in the FTSM, 51 patients in the LTSM, and 44 patients in the MTSM.To assess the outcomes of rehabilitation treatment, we used the MacNab scale, which distinguishes 4 possible outcomes of treatment: • excellent - no pain and no mobility restrictions, return to the previous level of activity; • good - infrequent/periodic non-radicular pain, improvement in the severity of existing symptoms, return to work with minor restrictions; • satisfactory - some increase in functional activity, the patient remains disabled; • poor - symptoms of root compression persist, re-treatment or surgery is necessary.
3. Results and Discussions
- During the clinical and neurological examination upon admission to the sanatorium, 27 patients had manifestations of vertebrogenic reflex syndrome, 55 - compression radicular syndrome, 38 - vascular radicular-spinal syndrome. The intensity of pain according to VAS in 30 (25%) patients corresponded to mild (3 points), in 87 (72.5%) - moderate (from 4 to 6 points, mean value 4.7 ± 0.71) and in 3 (2.5%) - strong (7 points).In the 1st group - FTSM, 25 patients (23.83%) were selected, in whom, due to the presence of minimal and mild manifestations of DDPD, according to radiological studies, there were no absolute contraindications to prescribing the full range of methods and techniques of therapeutic effects available in a sanatorium.In the 2nd group - LTSM, 51 patients were selected, in whom, according to the data of X-ray studies, the presence of manifestations of DDSD or other conditions of the spine, which are relative contraindications and limitations to the appointment of a full range of methods of therapeutic effect, namely, not pronounced osteoporosis (in 18 patients) was noted, spondylolisthesis of the 1st degree (in 11), lowering of the IVD height to 1/3, with the presence of extrusions up to 7 mm (in 16), the presence of unexpressed manifestations of spondylosis and osteoarthritis (in 21), vertebral hemangioma up to 1.5 cm (in 8), the presence of degenerative relative stenosis of the spinal canal without severe pain syndrome (9 patients).The 3rd group - MTSM included 44 patients, who, due to the presence of various combinations of pronounced and pronounced degenerative changes, according to radiation studies, showed pronounced osteoporosis (in 20 patients), degenerative stenosis of the spinal canal (in 12), spondylolisthesis II degree and higher (in 8), as well as a radiation picture corresponding to severe manifestations of Forestier's or Bechterew's disease (in 3), a decrease in IVD height to 1/2 or more, with extrusions of 8 mm or more (in 15); the presence of pronounced manifestations of spondylosis and osteoarthrosis with narrowing of the radicular foramina (in 13), instability of the SMS during functional tests (in 11).It should be noted that if massive (over 7 mm) extrusions, signs of their sequestration, and degenerative stenosis of the spinal canal were detected in a patient, a mandatory consultation with a neurosurgeon was required to decide whether these patients could undergo sanatorium treatment or cancel it and prescribe surgical intervention.After the treatment, we analyzed the outcomes of treatment according to the MacNab scale in the treatment-sanatorium groups.As can be seen from Table 1, in all three treatment-sanatorium groups there was a positive trend after the treatment. However, the best results were in the FTSM group, slightly worse results in the LTSM group, and lower results in the MTSM group. This is understandable, that the more restrictions there are in the treatment and sanatorium groups, the less the effect will be. However, it should be noted that as a result of such a distribution of patients into treatment and sanatorium groups, not a single patient had deterioration or complications, and most patients had an improvement, and only 6 (5%) patients had no changes. Thus, we have fulfilled the main requirement of medicine - "Do no harm!" and significantly in 95% of patients noted improvement of varying degrees.
|
ACKNOWLEDGEMENTS
- The authors are grateful to: the staff of the Department of Neurology and Psychiatry of the Urgench branch of the Tashkent Medical Academy in helping to select patients; to the employees of the sanatorium "Urgench" for their help in selecting patients and conducting differentiated treatment. The authors declare that they have no conflicts of interest when writing this article. The publication is funded from its own funds.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML