-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(2): 211-213
doi:10.5923/j.ajmms.20221202.32
Received: Feb. 1, 2022; Accepted: Feb. 18, 2022; Published: Feb. 24, 2022

Acute Heart Failure in Patients with Myocardial Infarction: Features of Development and High Risk of Sudden Death
Alimov D. A., Salakhitdinov Sh. N., Alimkhanov B. Sh., Akilova Sh. A., Jalolov B. Z.
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim of research was to evaluate possible predictors of the development of acute heart failure in patients with Q-wave myocardial infarction. Material and methods. The study included 112 male patients with Q-wave myocardial infarction. According to the performed thrombolysis, the patients were divided into 2 groups: group I (n=48) patients without thrombolysis, group II (n=64) with thrombolysis. Comparative analysis showed that in the group of patients without thrombolysis, acute heart failure was significantly more developed than in group 2 (87.5% vs. 42.6%, p<0.05). Using correlation analysis in a group of patients with thrombolysis, we analyzed the relationship of clinical and anamnestic indicators with the severity of acute heart failure. All patients during their stay in the hospital underwent echocardiographic examination of the heart according to the standard method - on the 1st day of the disease. An angiographic study was performed in 30 patients using the M Judkins technique, which included left and right polypositional coronary angiography to evaluate the state of the coronary bed on the 1st -5th day of myocardial infarction. Results. The analysis revealed the presence of a direct relationship between age, the presence of a history of diabetes mellitus and the severity of acute heart failure. The heart rate and radiological signs of venous congestion in the lungs were of significant importance. A direct relationship between the degree of the coronary arteries lesion and the severity of the acute heart failure was revealed according to the results of coronary angiography.
Keywords: Thrombolytic therapy, Acute heart failure, Myocardial infarction
Cite this paper: Alimov D. A., Salakhitdinov Sh. N., Alimkhanov B. Sh., Akilova Sh. A., Jalolov B. Z., Acute Heart Failure in Patients with Myocardial Infarction: Features of Development and High Risk of Sudden Death, American Journal of Medicine and Medical Sciences, Vol. 12 No. 2, 2022, pp. 211-213. doi: 10.5923/j.ajmms.20221202.32.
1. Introduction
- There is a significant decrease in the incidence of acute heart failure (AHF) due to the introduction of thrombolytic therapy (TLT) into clinical practice in the early stages of myocardial infarction (MI) [1-2]. Despite this, AHF is the most formidable complication of MI, as well as one of the urgent problems of cardiology, since it leads to death more often than other causes [3-4]. As it has been shown in many studies, the severity of AHF is stipulated by the volume of necrosis. Therefore, predicting the development of this complication in patients with MI allows to identify a group of patients with extensive lesion of the heart muscle who need more active treatment, and to reduce the duration of patients’ treatment in the hospital with a small volume of myocardial necrosis [3,5]. Researches in the field of predicting the development of AHF have been conducted for a long time, but the continuing frequency of AHF and mortality from it leaves this problem relevant [5-6,8]. It is stipulated by several reasons: polymorphism of numerous symptoms of the disease, low information content of signs determined on the first day of MI, significant influence on the course of MI of various types of treatment (thrombolysis, surgical correction in the early stages of the disease), which does not allow early prediction of complications and appropriate correction of therapeutic and diagnostic measures [6-7,9].Aim of research was to evaluate possible predictors of the development of acute heart failure in patients with Q-wave myocardial infarction.
2. Material and Methods
- We examined 112 patients (men) with large-focal myocardial infarction. Thrombolytic therapy (TLT) was performed in 64 patients at admission. As a comparison group (in order to determine the incidence of AHF in patients with large-focal MI who did not receive TLT), we selected 48 patients with MI of similar clinical forms and conditions, admitted in the first 12 hours of the disease, but for various reasons, thrombolysis was not performed ( contraindications, refusal of treatment). The diagnosis of MI was verified based on generally accepted criteria: clinical picture (anginal attack for more than 30 min); ECG data (ST-segment elevation by 1 mm and higher in standard - by 2 mm and higher in chest leads, at least in two leads); increased activity of cardiospecific enzymes in blood serum. Patients at the age from 40 to 79 years (mean age 62.5 +2.6 years) were admitted to the intensive care unit in the first 6 hours from the onset of the disease (on average after 3.6 ± 0.9 hours). Signs of myocardial reperfusion after TLT were observed in 40 (63.0%) from 64 patients. The classification of AHF proposed by Killip was used in our study. In patients who received TLT, the development of AHF was noted in 27 (42.6%) from 64 examined patients: in 24 (35.2%) – Killip class II, in 3 (7.4%) – Killip class III. AHF was developed in 42 (87.5%) from 48 patients with large-focal MI who were not performed TLT for various reasons, (p<0.05).We divided 64 patients who received TLT into two groups: the main group - 27 (42.6%) patients (according to Killip class II and III) and the control group - 37 (57.4%) patients (without clinical signs of AHF or Killip class I) to solve the set tasks. At the hospital stage of treatment, 5 (8%) from 64 patients examined by us, died. In our study, all 64 patients of the main and control groups received TLT at admission to the hospital. Treatment was carried out by intravenous injection of 1.5 million units of streptokinase for an hour. Standard therapy was prescribed after finishing TLT. All patients underwent ECG registration in 12 generally accepted leads: before TLT, immediately after thrombolysis, 24 hours after the onset of MI, on the 3rd and 5th day of MI. A troponin test was performed at admission. All patients during their stay in the hospital underwent echocardiographic (EchoCG) examination of the heart according to the standard method: on the 1st day of the disease. An angiographic study was performed in 30 patients to evaluate the state of the coronary bed on the 1st-5th day of MI using the M Judkins technique which included left and right polypositional coronary angiography. Statistical processing of the results was carried out using statistical software Statistica V10.0 (StatSoft Inc.), as well as a demo version of the program SPSS Statistics Desktop, Y22.0 (IBM). The critical level of significance when testing statistical hypotheses was taken equal to 0.05 (p-achieved level of significance). The description of quantitative data in the case of a normal distribution law was carried out in the form of an average value and a standard deviation (p ± o). The evaluation of the relationship of features was carried out using correlation analysis (the Spearman correlation coefficient was calculated).
3. Results
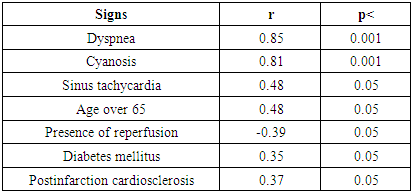
- The occurrence of AHF in patients with MI who received TLT was observed from the first hours of the disease to several days from its onset. Analysis of the data obtained showed that clinical signs of heart failure on the 1st day of MI were noted in 14 (52.2%) patients with AHF, on the 2nd day - in 8 (32.6%) cases, on the 3rd-5th day - in 5 (15.2%) patients. Signs of myocardial reperfusion after TLT were statistically significantly more common in the group of patients without AHF - in 34 (91.9%) from 37 patients in compare with 6 (23.9%) from 27 cases in patients of the main group (p<0, 05). Analysis of clinical symptoms relationship with the development of AHF revealed a significant positive correlation with sinus tachycardia and age over 65 years (Table 1).
|
4. Conclusions
- Analysis of the studied clinical parameters in patients with large-focal MI revealed that the main predictors of AHF development were: post-infarction cardiosclerosis, chronic heart aneurysm, diabetes mellitus, age over 64 years, absence of myocardial reperfusion signs after thrombolytic therapy. Instrumental laboratory predictors of acute heart failure development on the first day of myocardial infarction are: insufficient decrease of ST segment elevation (less than 50%), EF less than 50%, occlusion of the infarct-associated coronary artery.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML