-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(2): 205-210
doi:10.5923/j.ajmms.20221202.31
Received: Jan. 24, 2022; Accepted: Feb. 20, 2022; Published: Feb. 24, 2022

Acute Adhesive Small Bowel Obstruction: New Approaches to Treatment
Khakimov M. Sh., Karimov M. R., Elmuratov I. U., Tsay V. E., Kamalova S. Ya.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The treatment results of 272 patients with acute adhesive intestinal obstruction were analyzed. All patients were divided into two groups: Group I - 148 patients with the use of standard treatment tactics of AcuteAdhesive Small Bowel Obstruction: Group II - 124 patients, where the volume of surgical intervention and intraoperative prevention of adhesive obstruction were carried out according to the system proposed by the author for assessing the severity of the adhesive process. The authors proposed a morphological classification of the severity of adhesive disease; nasoenteral tube has been improved; an algorithm of therapeutic measures which consists in choosing a certain amount of surgical intervention and intraoperative prevention of the adhesive process has been proposed. The performed therapeutic measures allowed to significantly reduce the frequency of postoperative complications from 20.3% to 8.9%, postoperative mortality - from 6.1% to 3.2%.
Keywords: Adhesive small bowel obstruction, Nasoenteral tube, Classification of the disease, Therapeutic algorithm
Cite this paper: Khakimov M. Sh., Karimov M. R., Elmuratov I. U., Tsay V. E., Kamalova S. Ya., Acute Adhesive Small Bowel Obstruction: New Approaches to Treatment, American Journal of Medicine and Medical Sciences, Vol. 12 No. 2, 2022, pp. 205-210. doi: 10.5923/j.ajmms.20221202.31.
1. Introduction
- Acute adhesive small bowel obstruction (ASBO) is one of the leading causes of surgical emergencies and, in particular, requiring emergency surgical interventions. About 1% of previously operated patients are treated annually in surgical hospitals for adhesive disease, in 60-75% of whom acute adhesive intestinal obstruction is developed, the mortality from which ranges from 13-55% [1]. Surgical treatment of acute ASBO in almost every second patient leads to a relapse of the disease [2]. According to some authors’ data, the incidence of postoperative adhesive disease reaches 80% [3]. In Uzbekistan, according to various authors, despite the modern achievements of abdominal surgery and postoperative intensive care, the treatment results of patients with acute ASBO cannot be considered satisfactory, since the mortality rate achieves 17-29% [4-8].The risk of AASBO is highest after colorectal, oncological, gynecological surgeries [9]. In every tenth patient at least one episode of acute small bowel obstruction is developed within 3 years after colectomy [10]. Repeated surgeries due to AASBO occur in 4.2-12.6% of patients after gynecological operations [11]. Relapses of acute ASBO are also not uncommon: 12% of conservatively treated patients are re-hospitalized within 1 year, and after 5 years this index increases up to 20% [12]. The risk of relapse is slightly lower after surgical treatment: 8% after 1 year and 16% after 5 years [13].The most commonly used classification of adhesions in general surgery is the scale of adhesions according to Zühlke H.V. et al. [14]. The estimation is based on the prevalence of adhesions process in the abdominal cavity. The advantages of this scale are that it is easy to use, and the classification does not require explanations for most surgeons and gynecologists. The main disadvantage of the scale is that it does not take into account the morphological aspects of the adhesive process in different parts of the abdominal cavity. The most used evaluation system in gynecological surgery is the American Fertility Society (AFS) [15].According to the above mentioned, it seems promising to develop a system for assessing the severity of the adhesive process, as well as improving technical means to reduce the frequency of postoperative complications and mortality in this group of patients.The aim of our study was to improve the surgical treatment results of patients with AASBO by a differentiated approach to the choice of surgical treatment depending on the intraoperative assessment of the clinical situation severity.
2. Material and Methods
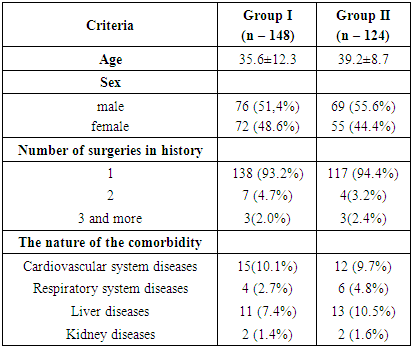
- This research is a single-center study of the treatment results of 272 patients with acute ASBO who were hospitalized and underwent various surgical interventions in the department of emergency Surgery of the Multidisciplinary Clinic of the Tashkent Medical Academy for the period from 2005 to 2021. Signed informed consent forms were received from all patients included in the study.All patients were divided into two groups: Group I – 148 patients admitted in the period from 2005 to 2012, whose treatment results were analyzed retrospectively; group II – 124 patients who sought surgical care in 2013-2021 and whose treatment efficiency was evaluated prospectively. Such a division was associated with different approaches to treatment as treatment measures are developed and improved. In Group I standard acute ASBO treatment tactics was used. In group II, the volume of surgical intervention and intraoperative prevention of adhesive obstruction were carried out according to our proposed system for assessing the severity of the adhesive process.The age of the patients ranged from 18 to 76 years (mean age was 37.6±10.3 years). More than 40% of patients were at a young, most able-bodied age – it emphasized the relevance and social significance of the problem. The sex ratio was dominated by males – 145 (53.3%) patients. The severity of the adhesive process is also influenced by the number of surgeries carried out in the anamnesis. The majority of patients (255 (93.8%)) underwent one surgery. 17 (6.2%) patients were performed two or more surgeries before contacting our hospital. By the nature of the surgeries undergone, acute ASBO developed after the following interventions: appendectomy (76 (27.9%) patients), hernia repair (62 (22.8%) patients), cholecystectomy (32 (11.8%) patients), obstetric and gynecological pathology (26 (9.6%) patients) and stab wounds (13 (4.8%) patients. When collecting anamnesis and objective examination of patients, we took into account the presence and severity of comorbidity, which influenced the course and severity of acute ASBO, as well as the treatment results (Tab 1.).
|
|
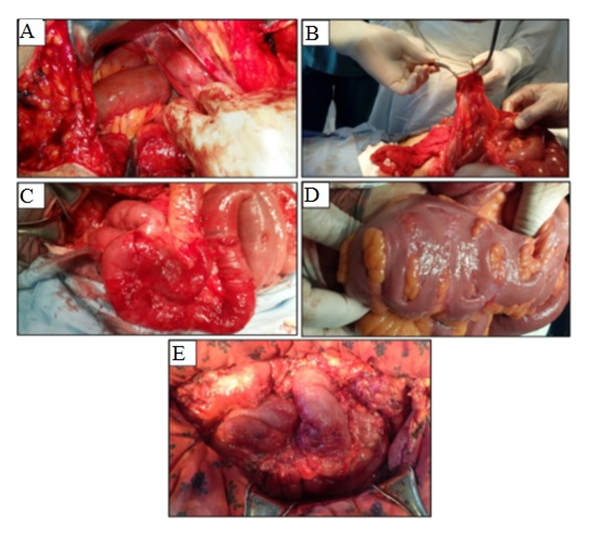
3. Results
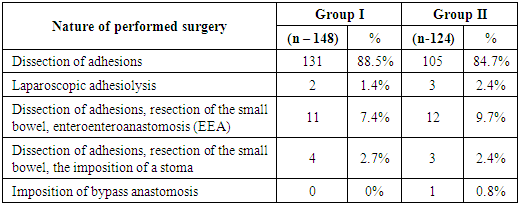
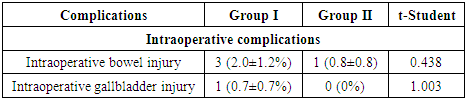
- The time from hospitalization to the start of surgery ranged from 2 to 36 hours. Majority of patients (236 (86.8%)) were performed dissection of adhesions: in 5 (1.8%) cases the surgery was performed laparoscopically; in 23 (8.5%) cases along with dissection of adhesions, resection of the small bowel was performed with the imposition of entero-enteroanastomosis (EEA); in 7 (2.6%) observations an enterostomy was imposed due to the presence of peritonitis after resection of the small bowel; in 1 (0.4%) case, a bypass interintestinal anastomosis was performed. In 250 (91.9%) cases surgical intervention was supplemented with nasoenteral intubation of the small bowel.The critical analysis of the existing acute ASBO classifications and systems of intraoperative assessment of the adhesive process severity, as well as histological examination of peritoneal adhesions, allowed us to propose an optimal system for assessing the severity of the adhesive process in the abdominal cavity. Five degrees of severity are distinguished according to the system of assessment of the adhesive process severity developed by us (Fig. 1.):
 | Figure 1. Macroscopic pattern of the adhesive process severity: A. Degree I; B. Degree II; C. Degree III; D. Degree IV; E. Degree V |
 | Figure 2. Advanced enteral tube |
|
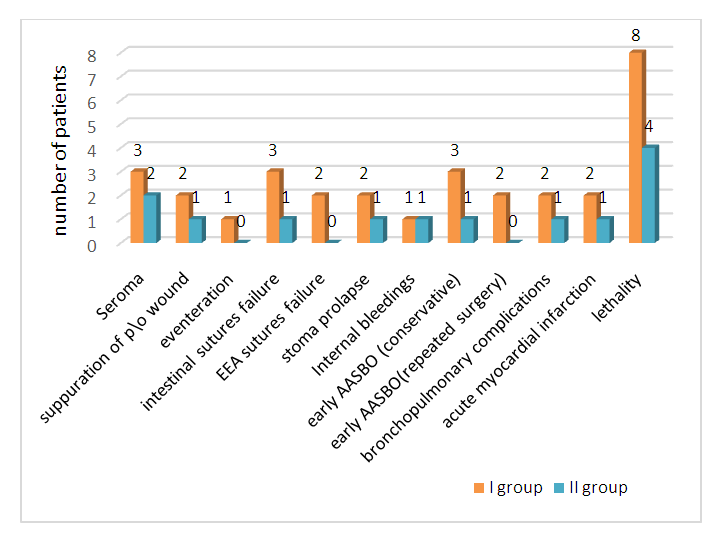 | Figure 3. Complications and mortality in the early postoperative period |
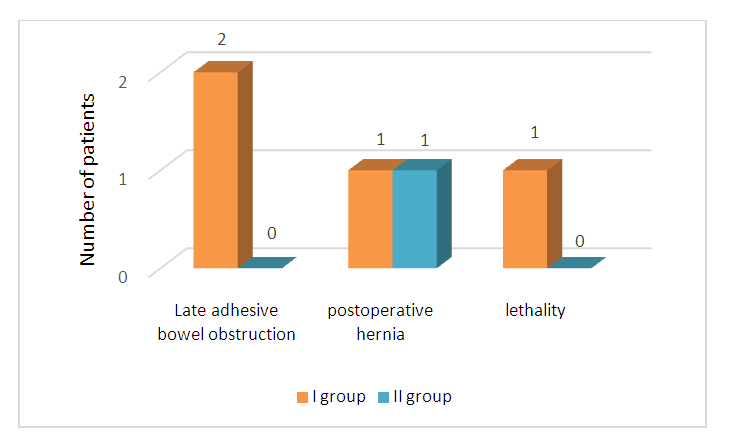 | Figure 4. Complications and mortality in the long-term period |
4. Discussion
- Acute ASBO makes up 12-16% of emergency surgical hospitalizations and 20% of emergency surgical interventions [7]. Even with the advent of laparoscopic surgery, intra-abdominal adhesions remain the main cause of bowel obstruction making up 65% of cases among other etiologies [8].The acute ASBO Working Group introduced the Peritoneal Adhesion Index (PAI), which measures the severity of adhesions on a scale from 1 to 3 in 10 specific places, followed by summation of points [16]. This score is the only one that has been validated as predictive of recovery after acute ASBO surgery and the risk of injury during adhesiolysis. The limitation for all these assessment scales of the adhesive process is that they are applicable only to operational cases, since they require an operational assessment. Besides, none of them has been confirmed yet in correlation with the long-term risk of relapse and complications associated with the adhesive process.The conducted critical analysis of the existing acute ASBO classifications and systems for estimation the severity of the adhesive process allowed us to propose an optimal system in terms of evaluation and practical in terms of choosing surgical tactics for assessing the severity of the adhesive process in the abdominal cavity.The main criteria for gradations into degrees were the nature of the adhesive process, the degree of involvement of the intestinal walls in the adhesive process, the possibility of dissection with or without violating the integrity of the intestinal walls.Based on the classification of the adhesive process severity developed by us, we performed intraoperative prevention of adhesions by introducing various substances into the abdominal cavity. At degree I, only after dissection and a combination of dissection using hydrocortisone, the development of a light and loose adhesive process was noted. Dissection of adhesions at degree II of the adhesive process without the use of any means was accompanied by the preservation of a relatively deep adhesive process. The use of mesogel with dissection of adhesions gave the most favorable effect in the form of the development of a light adhesive process. Anti-adhesive therapy at degree III showed that when dissection of adhesions was combined with the use of hydrocortisone, the preservation of moderately dense adhesions was noted.When using mesogel, a mild adhesive process was developed.Besides, all patients with acute ASBO should undergo bowel decompression using a wide lumen nasogastric tube or a long bowel tube to reduce enteral insufficiency and reduce the incidence of interintestinal anastomoses [17]. The nasogastric tube is easier to insert but less effective in decompressing the distal small bowel. Long bowel tubes can provide distal decompression. However, the introduction of such tubes requires special skills and can also lead to regurgitation, vomiting, respiratory and abdominal disorders, especially if the tube is dislodged, as well as to the potential risk of aspiration pneumonia [7].The standard enteral tube improved by us, due to the technical features of the structure, has certain advantages over existing analogues:• the possibility of selective decompression, drainage and enteral lavage of the intestinal suture zone; • at the development of partial suture failure, the restriction of the anastomosis zone on both sides warns to isolate this area from the intestinal contents and promotes the healing of the insolvency zone; • performing of radiopaque examination allows diagnosing the failure of the sutures of the interintestinal anastomosis.When analyzing the clinical results in the compared groups in the immediate and long-term periods, we obtained a significant decrease in the total number of postoperative complications from 20.3±3.3% (in Group I) to 8.9±2.6% (in Group II) (t=2.730). Postoperative mortality decreased by 1.9 times - from 6.1±2.0% to 3.2±1.6.Thus, the clinical results of using the developed complex treatment of patients with acute ASBOS using the tactical and technical improvements proposed by us showed the validity of their application. As a result of the complex treatment of acute ASBO, we have achieved a reduction in the frequency of postoperative complications, their severity and the number of fatal cases was decreased.
5. Conclusions
- To assess the adhesive process severity in the abdominal cavity, the most convenient to use and practical in using is the system proposed by us, according to which five degrees of severity of the pathological process were distinguished, the gradation of which was justified by morphological studies.The morphological studies carried out allowed to determine the most optimal volume of surgical intervention (from dissection of adhesions with intestinal resection to the imposition of intestinal anastomoses) and a more effective way of intraoperative prevention of adhesions (the use of hydrocortisone or mesogel), depending on the severity of the pathological process in the abdominal cavity.An improved enteral tube and a differentiated approach to choosing a method for preventing adhesions can reduce the incidence of such terrible complications as intestinal suture failure and interintestinal anastomoses, reduce the development of early acute ASBO and relapses of adhesive disease, as well as the associated mortality.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML