-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(2): 195-199
doi:10.5923/j.ajmms.20221202.29
Received: Jan. 28, 2022; Accepted: Feb. 12, 2022; Published: Feb. 24, 2022

Efficiency of Reconstructive Surgery for Neuroischemic Ulcers on the Background of Diabetic Foot Syndrome
K. J. Matmurotov, T. Sh. Atajanov, D. N. Saitov, I. T. Dushamov, N. A. Ruzmetov
Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: K. J. Matmurotov, Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Increased number of patients with diabetes mellitus (DM) in the world, the number of surgical complications is also steadily growing. In surgical practice, purulent complications associated with diabetic foot syndrome (DFS) are the most common. Damage to the bone structure of the foot is often a tragedy for patients with neuropathic DFS and in most cases leads to the loss of the lower limb. To solve this issue in modern medicine, a deep knowledge of a specialist in this area and the development of new optimal methods of surgical treatment are required.
Keywords: Diabetes mellitus, Diabetic foot syndrome, Diabetic neuroosteoarthropathy
Cite this paper: K. J. Matmurotov, T. Sh. Atajanov, D. N. Saitov, I. T. Dushamov, N. A. Ruzmetov, Efficiency of Reconstructive Surgery for Neuroischemic Ulcers on the Background of Diabetic Foot Syndrome, American Journal of Medicine and Medical Sciences, Vol. 12 No. 2, 2022, pp. 195-199. doi: 10.5923/j.ajmms.20221202.29.
Article Outline
1. Introduction
- One of the most severe complications of diabetes mellitus (DM) which leads to surgery is diabetic foot syndrome (DFS). The diabetic foot syndrome manifests itself in the form of the development of widespread purulent-necrotic lesions in the lower extremities, which develop in 35-60% of patients with DM [4]. Diabetic neuroosteoarthropathy (DNOAP, Charcot's foot, Charcot's joint) is a rare but extremely severe complication of diabetes mellitus, leading to irreversible disability in case of inadequate treatment [1,3].The occurrence of complications in the bone tissue on the background of diabetes mellitus can be called one of the most mysterious forms of diabetic foot syndrome, since it is extremely difficult to predict the development of DNOAP and identify risk groups among patients with diabetes mellitus [7].This complication of diabetes is encountered by doctors of various specialties such as surgeons, endocrinologists, orthopedists, but it is far from always recognized in time. Pathogenetically, with the appearance of signs of diabetic neuropathy in patients, it is possible to detect a violation of arterial blood flow in the lower extremities, and according to the literature data, the primary substrate or trigger of the etiological manifestation of diabetic foot syndrome is precisely neuropathy [2].The prevalence of this complication among patients with diabetes mellitus is less than 1% [5], although in the literature one can find information about various manifestations of DNOAP in 18–25% of people with a duration of diabetes of more than 20 years [3,9]. Such inconsistency of information is obviously associated with differences in the examination methodology and different criteria for diagnosing neuroosteoarthropathy.An untimely diagnosis of the acute stage of DNOAP and, accordingly, late treatment led to pronounced changes in the bones and joints of the foot and the formation of irreversible deformities [10]. In the future, due to the resulting bone protrusions and a change in the biomechanics of the foot, high pressure zones are formed with crushing of the underlying soft tissues and, as a result, long-term non-healing, recurrent ulcerative defects. Attachment of signs of ischemia complicates the problem before the practicing surgeon to obtain the expected result of treatment [6,13].Infection of wound defects, development of phlegmon, bone osteomyelitis, and destructive osteoarthritis significantly increase the risk of high amputations in neuro-ischemic ulcers [12]. Data on the frequency of purulent complications, amputations, as well as long-term results of reconstructive surgery in this category of patients are contradictory [8,14].In connection with the foregoing, the following clinical observation of a patient with a neuro-ischemic ulcer of the plantar surface against the background of severe ischemia, who retained the support function of the foot with the help of an individually developed strategy of surgical treatment, consisting of repeated surgical treatments (for phlegmon of the foot and purulent lesions of bones and joints), is of interest) and plastic reconstruction of the foot.In this regard, the purpose of this study was to improve the results of treatment of patients with neuro-ischemic foot ulcers against the background of diabetic foot syndrome (DFS).
2. Material and Methods
- The results for 2019-2020 years were analyzed which surgical treatment has been done on 27 patients who received inpatient treatment with chronic neuro-ischemic ulcers against the background of DFSin the department of purulent surgery at the multidisciplinary clinic of the Tashkent Medical Academy.The average duration of diabetes mellitus was 12.3±4.7 years. The age of the patients ranged from 41 to 68 years (average 53.6±4.9 years). Among the patients there were 18 (66.7%) men and 9 (33.3%) women. In all cases, a neuro-ischemic form of diabetic foot syndrome was diagnosed. The duration of inpatient treatment of patients averaged 5-7 days. Prior to admission to the clinic, the duration of neuro-ischemic foot ulcer in patients was on average from 4 months to 3 years.During the examination, 15 (55.6 %) patients showed signs of coronary heart disease (CHD). In 2 (7.4%) cases, there were signs of transient cerebrovascular accidents in the anamnesis. Arterial hypertension was detected in 11 (40.7 %) patients.An instrumental method for assessing the state of macrocirculation was ultrasonic duplex scanning of the lower extremities, performed on an ultrasonic duplex system Medison-X6 (Samsung, Germany) using a standard technique with a linear probe with a frequency of 7-15 MHz. Ankle-brachial index (ABI) was also determined using ultrasound to assess arterial blood flow disorders and the degree of foot ischemia.The final diagnostic method was multi-slice computed tomography (MSCT) of the arteries of the lower extremities. After receiving information about the state of the peripheral arterial bed, all patients underwent restoration of blood flow by balloon angioplasty. In the case of elevated urea and creatinine in the blood, MRI was done - arterial vessels of the lower extremities. Statistical data processing was carried out using the application software for statistical processing of the database DBASE and STAT4.For patients after endovascular revascularization against the background of improved arterial circulation, we applied an improved method of foot reconstruction in chronic neuro-ischemic ulcers in patients with diabetic foot syndrome, by myoplasty (closing the operating bed) after resection of bones or joints and with the removal of fragmented particles of bone tissue, taking into account the preservation of arterial network of the foot (Republic of Uzbekistan No. IAP 2019 0202 dated 05/13/2019 "Method of reconstruction of the foot with neuro-ischemic ulcers against the background of diabetic foot syndrome").The proposed operation is performed under local conduction anesthesia. At the first stage of foot reconstruction, in order to prevent arterial network disorders (damage to the plantar arteries), the pathological focus is accessed from the dorsal surface. And at the second stage, the head of the metatarsal bone is resected with the removal of fragmented particles. The final stage of the operation includes myoplasty with m. flexor digiti minimi brevis on a feeding leg with filling of the resected bone tissue bed.
3. Results
- With helping developed method of reconstructive surgery of the foot in patients with neuro-ischemic wound on the background of diabetes mellitus, we managed to obtain good results and in 96.3% of cases primary healing of the postoperative wound was noted. Only one patient showed signs of secondary suppuration of the postoperative wound, and this was due to non-compliance of the patient, because despite the recommendations for unloading the limb after discharge from the clinic, he actively moved with the help of the affected limb. In this case, the patient was re-hospitalized and a course of antibiotic and infusion therapy was carried out along with repeated sanitation. As a result, the postoperative wound healed by secondary intention without any other complications.In other cases, the sutures were removed after the control radiography of the foot, and in this case, we focused on the appearance of a primary callus and consolidation in the area of the resected foot bone. After the operation, patients were recommended to wear orthopedic shoes. At the same time, in most cases, we imposed Total Contact Cast (TCC) on patients to prevent possible further complications.Clinical ObservationPatient K.N., born in 1954 Source Patient No. 378/27, 01/05/2020 turned to our department with complaints of a purulent non-healing wound of the plantar surface of the left foot, fever, pain and redness of the foot. For the first time, a purulent wound appeared 2.5 years ago, and the patient repeatedly received inpatient treatment in surgical departments at the place of residence. Suffering from diabetes. The last 3 days the purulent discharge began to increase and the pains on the foot intensified. Locally: the lower limbs are asymmetric, due to swelling of the left foot. On the plantar surface of the left foot there is a purulent-necrotic wound measuring 3.0 x 4.0 cm. A copious purulent discharge with a fetid odor is released from the wound. In the area of the plantar and dorsal surfaces of the foot, there is a pronounced infiltration and soreness. On peripheral arteries the pulsation is not defined. The patient was recommended a contrast study of the vessels of the lower extremities.The patient was found to have signs of a neuroischemic ulcer of the plantar surface of the left foot, complicated by phlegmon, against the background of critical ischemia of the foot (see Fig. 1).
 | Figure 1. Neuroischemic ulcer of the plantar surface of the foot and subluxation of the head of the V-metatarsal bone with destruction |
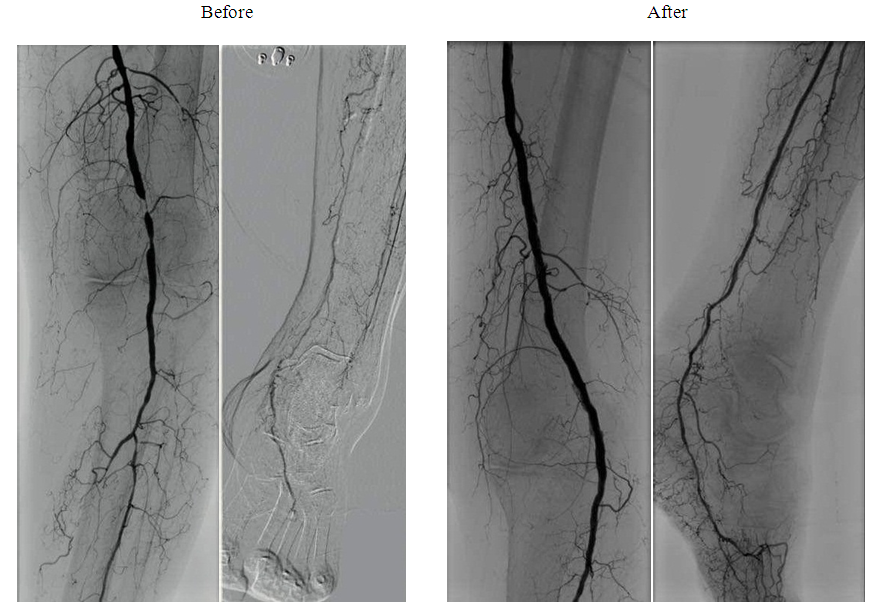 | Figure 2. Segmental occlusion of popliteal artery (PoA), total occlusion of the arteries of the lower leg before and after balloon angioplasty (BAP) |
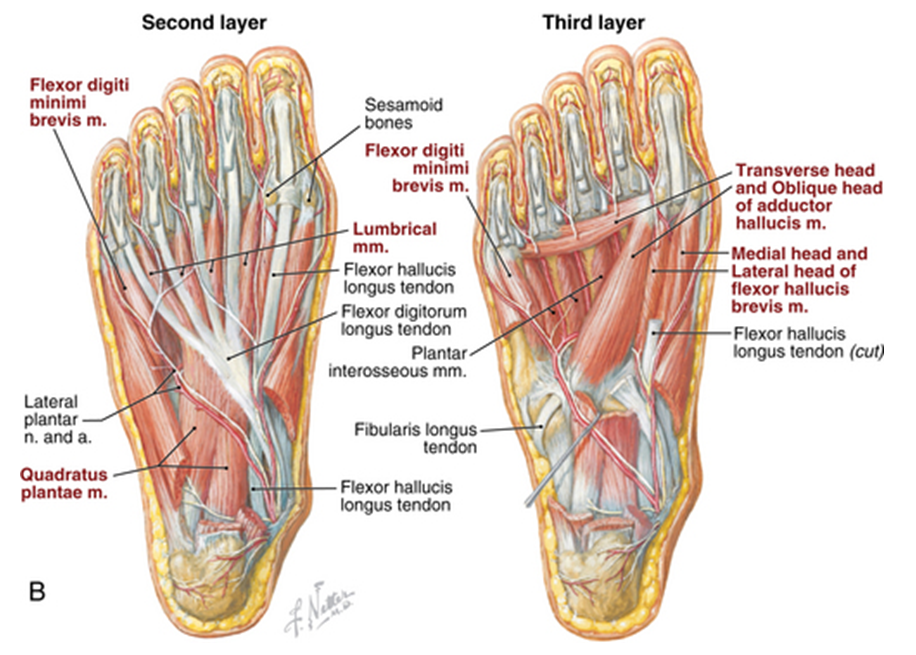 | Figure 3. The pathological focus and the muscle for plasty (Photo was taken from the website: musculoskeletalkey.com) |
 | Figure 4. View of the foot after reconstruction |
 | Figure 5. Day 17 after foot reconstruction |
4. Discussion
- Analysis of the results of treatment of patients with neuroischemic foot ulcer against the background of diabetic foot syndrome showed that with the correct definition of the treatment strategy, in 96.3% of cases it is possible to ensure a smooth course of the wound process, with the primary tension of the postoperative wound. These results were achieved due to the correct selection of operational equipment according to the original method developed by us.To choose an adequate technique of surgical intervention on the foot in the presence of chronic neuroischemic ulcers, in our opinion, is possible only by conducting a comprehensive examination of the patient, taking into account a number of objective data. When determining the treatment strategy, one should take into account the general condition of the patient, the degree of damage to local tissues on the foot, and the compensation of limb ischemia.The issue of the need for revascularization operations of the lower extremity in patients with trophic ulcers on the foot should be decided only after assessing the possibility of endovascular intervention, the successful implementation of which can reduce the level of postoperative complications and high amputations of the lower extremities. The question of the possibility of direct revascularization of the limb should be decided before surgery, based on the data of detailed duplex scanning and MSCT of the arteries of the lower extremities. At the same time, to determine the scope of the operation, an objective assessment of the degree of impairment of peripheral arterial blood flow is required based on the data of the above research methods.When preparing patients for a complex of therapeutic measures, it is important to pay special attention to the correction of rheological and coagulation properties of blood, normalization of the functional state of cardiac activity, as well as to convey important information to the patient and relatives about further rehabilitation tactics, in particular, wearing orthopedic shoes to prevent recurrent purulent complications of the foot.
5. Conclusions
- Complete information about the state of foot tissues in chronic neuroischemic ulcers against the background of diabetic foot syndrome allows choosing an adequate treatment strategy using minimally invasive and surgical interventions on the foot. The optimal intervention for lesions of the plantar surface is the use of the original method of foot reconstruction, which in 96.3% of cases will provide an excellent treatment result.Patients with a purulent-necrotic process in the foot area with diabetes mellitus are shown adequate comprehensive diagnostics to determine individual treatment tactics. Determining the level of occlusive-stenotic lesions of the peripheral arteries of the lower extremities, if indicated, its correction by the endovascular route plays an important role in achieving the expected result in purulent-necrotic lesions of the feet in patients with diabetes mellitus.
Consent
- It is not applicable.
Ethical Approval
- It is not applicable.
Competing Interests
- Authors have declared that no competing interests exist.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML