Mansurov A. A., Ilkhomov O. E., Abrorkhonov A. A.
JSC "Republican Specialized Scientific and Practical Medical Center of Surgery Named after Academician V. Vakhidov"
Correspondence to: Ilkhomov O. E., JSC "Republican Specialized Scientific and Practical Medical Center of Surgery Named after Academician V. Vakhidov".
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The aim of the study was to assess the tactical and technical aspects of surgical treatment of patients with coronary heart disease and atherosclerotic lesions of the cerebral vessels. Methods: The study was based on the results of treatment of 203 patients with multifocal atherosclerosis, combined lesions of the coronary and brachiocephalic arteries, which were divided into two groups depending on the study periods: - the comparison group (retrospective analysis) consisted of 102 patients who received treatment for the period from 2011 to 2015. inclusive. - the main group (prospective analysis) consisted of 101 patients who received treatment from 2016 to 2020. according to the developed treatment and diagnostic algorithm and improved tactical and technical aspects. Results: Optimization of the tactical and technical aspects of surgical operation of combined CA and BCA lesions made it possible to achieve a reduction in the overall incidence of complicated postoperative course from 22.2% (18 out of 81) in the comparison group to 7.5% (6 out of 80) in the main group, specific cardiac - from 21.0% (17 out of 81) to 8.75% (7 out of 80), and neurological complications from 22.2% (18 out of 81) to 6.25% (5 out of 80).
Keywords:
Combined atherosclerotic damage, Brachiocephalic artery, Coronary artery
Cite this paper: Mansurov A. A., Ilkhomov O. E., Abrorkhonov A. A., Improvement of Tactical and Technical Aspects of Surgical Treatment of Patients with Combined Atherosclerotic Damage of the Coronary and Brachiocephalic Arteries, American Journal of Medicine and Medical Sciences, Vol. 12 No. 2, 2022, pp. 189-194. doi: 10.5923/j.ajmms.20221202.28.
1. Introduction
As a result of long-term systemic atherosclerotic progression, many patients with coronary atherosclerosis also have occlusive-stenotic atherosclerotic lesions of the carotid arteries (CA) [1,2,4], this issue is of particular relevance in elderly and senile patients due to the high prevalence of multifocal atherosclerotic lesions. Thus, among patients who underwent carotid endarterectomy (CEA), in 28% of cases, coronary artery bypass grafting (CABG) was indicated. Similarly, a hemodynamically significant CA lesion with more than 80% lumen stenosis can be detected in 12% of patients with indications for coronary revascularization [3,4,5,12].The ideal therapeutic strategy for concomitant atherosclerotic disease of the brachiocephalic arteries (BCA) and coronary arteries (CA) remains difficult to achieve. Although investigators have argued for the potential benefits of different management protocols based on either single or staged surgical treatment There is still no consensus between national and international guidelines for reducing the risk of postoperative neurological complications. The advantages of a single-stage approach include: reduced intraoperative mortality in patients with symptomatic coronary artery and carotid artery stenosis, reduced cost of hospitalization and surgical procedures, shorter hospital stay, and lower risk of stroke during long-term follow-up [6,7,8,9]. There are also studies favoring a stepwise approach with CEA prior to CABG and vice versa, due to the apparent benefit of shortening the operation time and minimizing the surgical complexity of the two surgical procedures [10,11].All this determines the relevance of the chosen topic and gives ground for reflection and development of improved tactical and technical aspects of the surgical treatment of this pathology.The purpose of this study is to evaluate the tactical and technical aspects of the surgical treatment of patients with coronary artery disease with concomitant atherosclerotic lesions of the cerebral vessels.
2. Material and Methods
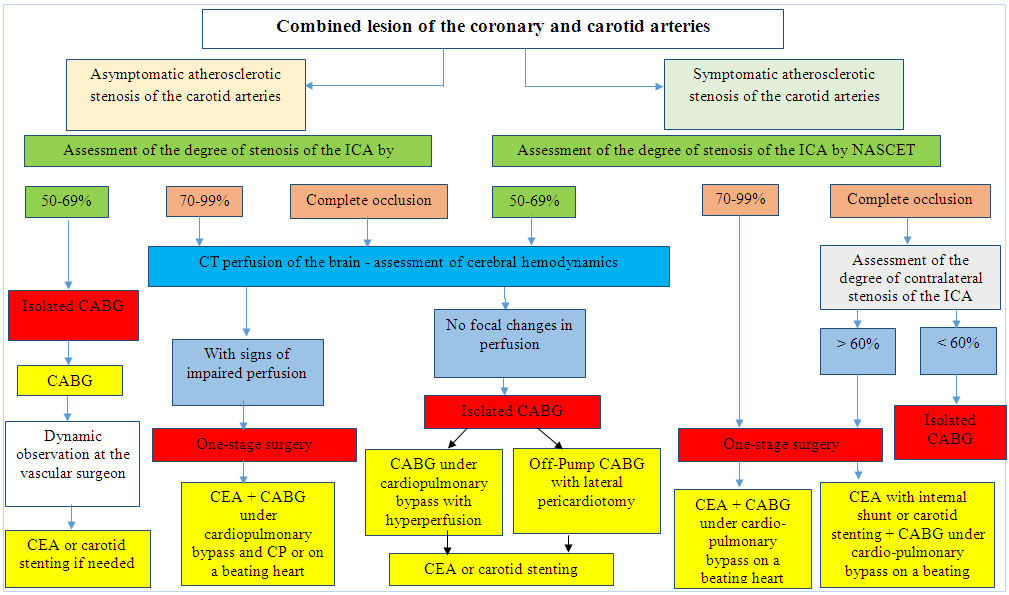
The study was based on the results of treatment of 203 patients with multifocal atherosclerosis, concomitant lesions of the coronary and brachiocephalic arteries. Who underwent simultaneous and staged operations on the coronary artery and BCA in the Department of Surgery for IHD and its Complications and in the Department of Vascular Surgery of RSSPMCS named after V.Vakhidov for the period from 2011 to 2020.The patients were divided into two groups depending on the periods of the study:- the comparison group (retrospective analysis) consisted of 102 patients who received treatment for the period from 2011 to 2015 (inclusive).- the main group (prospective analysis) consisted of 101 patients who received treatment from 2016 to 2020 according to the developed diagnostic and treatment algorithm (Fig. 1) and improved tactical and technical aspects.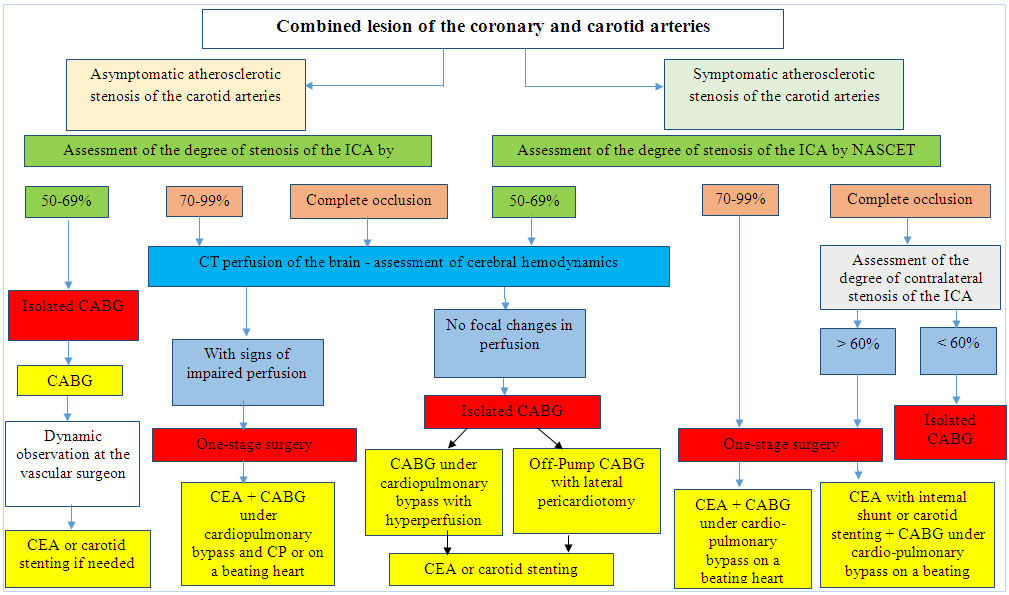 | Figure 1. Algorithm for Surgical Treatment of Combined Lesions of the Coronary and Brachiocephalic Arteries |
3. Results
3.1. The Results of Simultaneous Surgical Interventions on the Coronary and Carotid Arteries
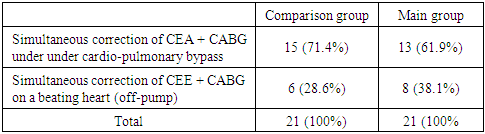
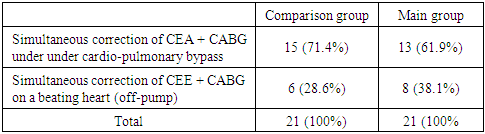
With simultaneous surgical interventions (Table 1), in most cases in the comparison group (71.4%; 15 out of 21), CABG was performed under EC, while in the main group this type of operation was performed less frequently and amounted to 61.9% (13 out of 21). 21). Simultaneous correction of CEA + CABG on a beating heart (off-pump) was performed in 6 out of 21 (28.6%) patients in the comparison group and in 8 out of 21 (38.1%) patients in the main group, i.e. with a higher frequency than in the comparison group.Table 1. Distribution of Patients According to the Tactics of Simultaneous Correction of Combined Lesions of the CA and BCA
 |
| |
|
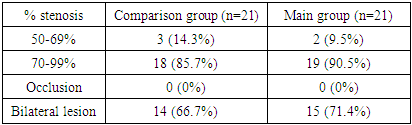
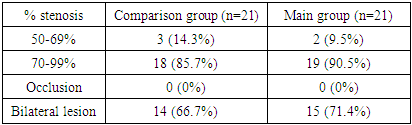
The distribution of patients with indications for simultaneous surgical correction according to the degree of carotid artery stenosis (Table 2) showed that most patients had 70-99% stenosis of the CA lumen: in the comparison group, in 85.7% (18 of 21) cases, in the main group – 90.5% (19 out of 21). Cases with complete CA occlusion were not noted in both groups. At the same time, in most cases patients with bilateral lesions were selected for simultaneous surgery, both in the comparison group (66.7%) and in the main group of patients (71.4%).Table 2. Distribution of patients with indications for simultaneous surgical correction according to the degree of carotid artery stenosis
 |
| |
|
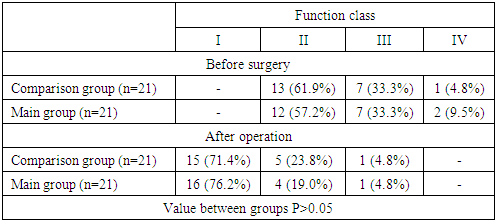
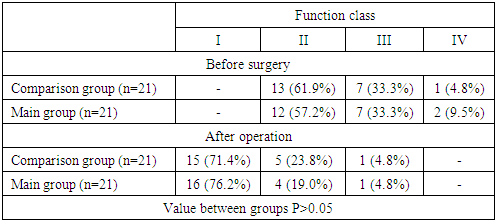
The distribution of patients according to the FC of CHF according to the NYHA classification in the mid-term postoperative period did not show a statistical difference between the study groups. Both in the comparison group (71.4%) and in the main group (76.2%), most patients were transferred to functional class I (Table 3).Table 3. Dynamics of the Functional Class of CHF According to the NYHA Classification Before Surgery and in the Medium-Long Term (6 months) After Simultaneous Operations on the Coronary Artery and BCA
 |
| |
|
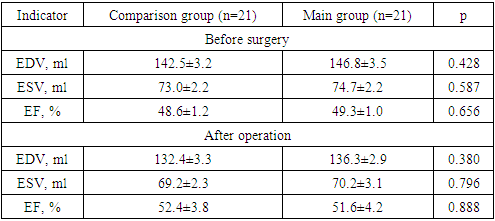
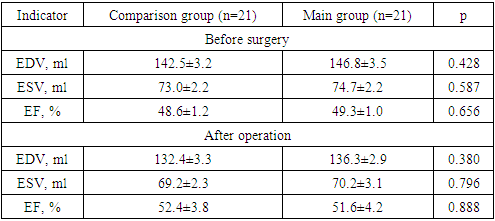
Analysis of the dynamics of EchoCG parameters showed that in both study groups, EDV decreased with a significant difference in relation to preoperative values – from 142.5±3.2 ml to 132.4±3.3 ml in the comparison group and from 146.8±3.5 ml to 136.3±2.9 ml in the main group, however, there was no intergroup difference (p=0.380). Similar dynamics was revealed in relation to CSR, where in the comparison group the postoperative indicator was 69.2±2.3 ml in the comparison group and 70.2±3.1 ml in the main group (p=0.796). The LV EF in the early postoperative period was 52.4±3.8% in the comparison group and 51.6± 4.2% in the main group (p=0.888). Thus, the effectiveness of simultaneous operations in the study groups was statistically comparable in terms of improving the most important parameters of the contractile function of the heart (Table 4).Table 4. Dynamics of EchoCG Parameters Before and After Simultaneous Operations on the CA and BCA
 |
| |
|
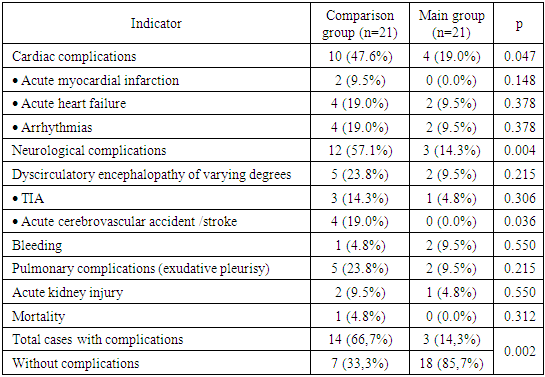
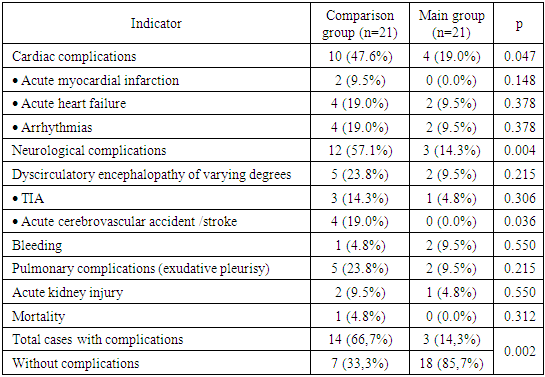
Comparative analysis of the frequency of postoperative complications (Table 5) after simultaneous surgical interventions on CA and BCA showed that hemorrhagic complications were observed in 4.8% (1 out of 21) of cases in the comparison group and 9.5% (2 out of 21) in the main group, which was due, as noted above, to the maintenance of higher blood pressure during CPB.Table 5. Analysis of the Frequency of Postoperative Complications in Simultaneous Coronary and Carotid Surgery
 |
| |
|
Pulmonary complications in the form of exudative pleurisy were observed with a higher frequency in the comparison group (23.8%; 5 out of 21) than in the main group (9.5%; 2 out of 21), without statistical difference (p=0.215). In addition, in relation to the incidence of acute kidney injury, no statistical difference was obtained (p = 0.550, 4.8% in the main group versus 9.5% in the control group).Further, cardiovascular complications are considered as the most significant group of complications characteristic of combined surgery of the coronary and carotid arteries. Thus, AMI was noted in the comparison group in 2 (9.5%) patients, while in the main group AMI was not observed (p=0.148). Acute postoperative heart failure developed in 9.5% (2 out of 21) of cases in the main group and was higher than in the comparison group (19.0%; 4 out of 21) without significant difference (p=378). The same values were obtained in relation to the frequency of occurrence of various arrhythmias (AF, tachycardia). The overall incidence of cardiac complications decreased from 47.6% (10 out of 21) in the comparison group to 19.0% (4 out of 21) in the main group (p=0.047).The overall incidence of various neurological complications was 57.1% (12 out of 21) in the comparison group and 14.3% (3 out of 21) in the main group (p=0.004). At the same time, dyscirculatory encephalopathy was noted in 5 (23.8%) patients in the comparison group and 2 (9.5%) in the main group (p=0.215). The frequency of TIA was also higher in the control group (14.3% vs. 4.8%; p=0.306). At the same time, in the main group of patients, postoperative stroke/stroke was not observed, its proportion was 19.0% (4 out of 21) and had a statistical difference (p = 0.036) in the comparison group, where 1 (4.8%) death was also noted. Outcome due to stroke and OSHF.
3.2. The Results of a Staged Approach to the Surgical Treatment of Combined Lesions of the Coronary and Carotid Arteries
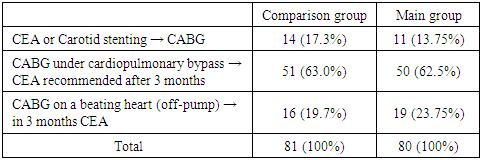
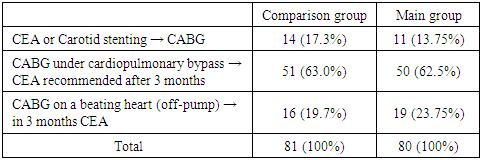
With staged surgical interventions (Table 6), in most cases, the first stage was CABG under EC: 63.0% (51 out of 81) in the comparison group and 62.5% (50 out of 80) in the main group. CABG on a beating heart was performed as the first stage in 17.3% (14 out of 81) cases in the comparison group and 13.75% (11 out of 80) in the main group of patients. There were 14 (17.3%) patients after CEE and with indications for CABG in the comparison group and 11 (13.75%) in the main group.Table 6. Distribution of Patients According to the Tactics of Staged Correction of Combined Lesions of the CA and BCA
 |
| |
|
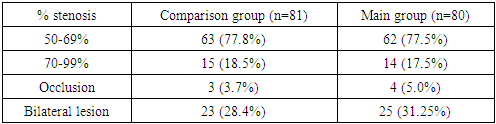
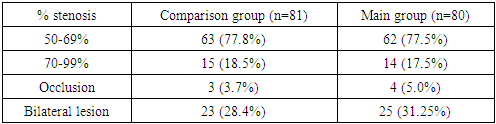
Staged surgical correction of combined lesions of the CA and BCA in most cases was performed by patients with 50-69% CA stenosis, both in the comparison group (77.8%; 63 out of 81) and in the main group (77.5%; 62 out of 80). ) (Table 7). In all cases with occlusion of the carotid arteries, both in the comparison group (n=3) and in the main group (n=4), more than 60% collateral stenosis was noted, due to which staged operations were performed (isolated CABG, subsequent dynamic monitoring was recommended in vascular surgeon). Also, in this cohort of patients, the majority of patients with bilateral lesions of the CA included in this scientific work were observed. Thus, 23 (28.4%) patients in the comparison group and 25 (31.25%) in the main group had bilateral lesions.Table 7. Distribution of patients with indications for staged surgical correction according to the degree of CA stenosis
 |
| |
|
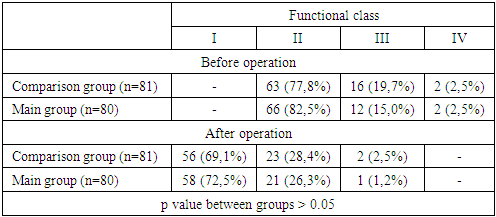
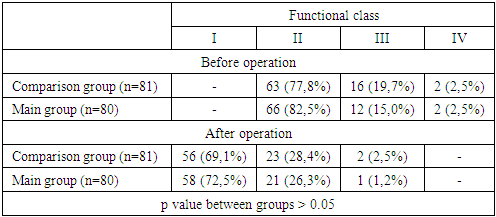
Table 8 shows that when distributing patients according to FC according to the NYHA classification in the mid-term postoperative period (6 months), there was no statistical difference in favor of any study group. So, both in the comparison group (77.8%) and in the main group (83.5%), the majority of patients before surgery were transferred to FC II. Patients with FC I were not observed in both groups (Table 8).Table 8. Dynamics of the Functional Class of NYHA in the pre- and mid-Term Periods (6 months) After Staged Surgery of CA and BCA
 |
| |
|
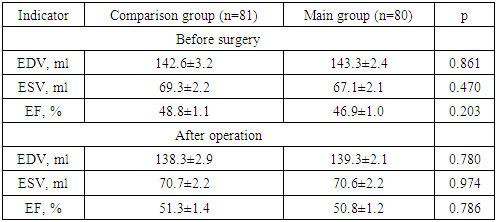
In the postoperative period, as a result of improving the functionality of the cardiovascular system, a significant proportion of patients were referred to FC I - in the comparison group 56 (69.1%), in the main group - 58 (72.5%).Analysis of the dynamics of EchoCG parameters showed that EDV decreased from the initial 142.6±3.2 ml to 138.3±2.9 ml in the comparison group and from 143.3±2.4 ml to 139.3±2.1 ml in the main group, however, there was no intergroup difference (p=0.780). Similar dynamics was revealed in relation to CSR, where in the comparison group the postoperative index increased from the initial 69.3±2.2 ml to 70.7±2.2 ml and from 67.1±2.1 ml to 70.6± 2.2 ml in the main group (p=0.974).The LV EF in the early postoperative period was 51.3± 1.4% in the comparison group and 50.8±1.2% in the main group (p=0.888). Thus, the effectiveness of a staged approach in surgery for combined lesions of the coronary artery and ACA in the study groups was statistically comparable in terms of improving the most important parameters of the contractile function of the heart (Table 9).Table 9. Dynamics of EchoCG Parameters Before and After Staged Coronary and Carotid Surgery
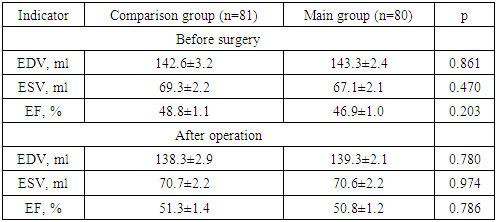 |
| |
|
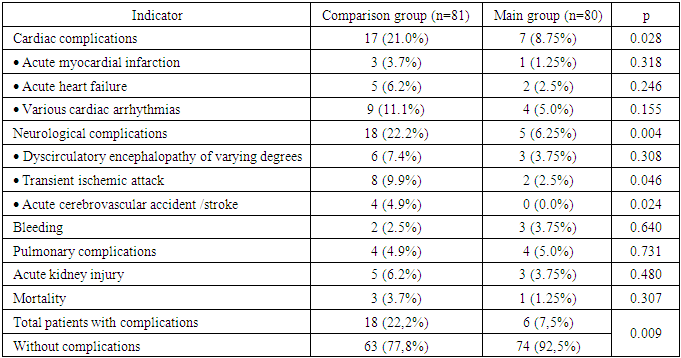
Table 10 shows that the overall incidence of complicated course after the application of the staged approach was 7.5% (6 out of 80) in the main group and 22.2% (18 out of 81) in the comparison group (p = 0.009).In a comparative analysis of the frequency of postoperative complications (Table 10), after applying the staged approach, 2 (2.5%) cases of bleeding were observed in the comparison group, in one of which resternotomy was performed to stop bleeding. In the main group, the frequency of bleeding was higher, amounting to 3.75% (3 out of 80), but in all cases it was possible to stop the bleeding conservatively.Table 10. Analysis of the Frequency of Postoperative Complications in Staged Surgery of CA and BCA
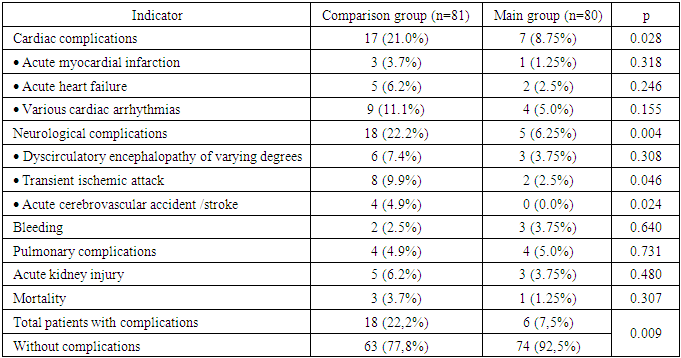 |
| |
|
Pulmonary complications in the form of exudative pleurisy were observed with almost equal frequency. Also, in relation to the incidence of acute kidney injury, no statistical difference was obtained (p = 0.480, 3.75% in the main group versus 6.2% in the control group).In the structure of cardiac complications, AMI was observed in 3 (3.7%) patients in the comparison group, while in the main group, AMI developed in 1 (1.25%) patient (p=0.318) with effective conservative therapy. Acute postoperative heart failure developed in 6.2% (5 out of 81) of cases in the main group and was higher than in the comparison group (2.5%; 2 out of 80) without significant difference (p=0.246).Various cardiac arrhythmias were noted with a higher frequency (p=0.155) in the comparison group (11.1%; 9 out of 81) than in the main group (5.0%; 4 out of 80).The overall frequency of various neurological complications was lower with a significant difference (p=0.004) in the main group (6.25%; 5 out of 80) than in the control group (22.2%; 18 out of 81). At the same time, dyscirculatory encephalopathy was noted in 6 (7.4%) patients in the comparison group and 3 (6.25%) in the main group (p=0.308). The frequency of TIA (9.9% vs. 2.5%; p=0.046) and stroke (0.0% vs. 4.9%; p=0.024) was also higher in the control group and had a statistical difference. A lethal outcome due to stroke and OSHF was observed in 3 (3.7%) cases in the comparison group and in 1 patient (1.25%) in the main group (p=0.307).
4. Conclusions
This algorithm for choosing the tactics of surgical treatment of combined atherosclerotic lesions of the coronary and brachiocephalic arteries makes it possible to determine the stages and type of surgical intervention, taking into account the results of clinical and radiological methods of investigation.Optimization of the tactical and technical aspects of performing simultaneous surgical interventions in patients with combined lesions of the coronary artery and BCA made it possible to improve the indices of intraoperative management of patients under EC conditions, to reduce the overall incidence of complicated postoperative course from 66.7% (14 out of 21) in the comparison group to 14.3 % (3 out of 21) in the main group (p=0.002), incidence of cardiac complications from 47.6% (10 out of 21) to 19.0% (4 out of 21) (p=0.047), stroke/stroke from 19, 0% (4 out of 21) to 0.0% (p=0.036) and mortality from 4.8% (1 out of 21) in the comparison group to 0.0% (p=0.312) in the main group.Optimization of the tactical and technical aspects of the staged surgical correction of combined lesions of the coronary artery and the BCA made it possible to achieve a reduction in the overall incidence of complicated postoperative course from 22.2% (18 out of 81) in the comparison group to 7.5% (6 out of 80) in the main group (p =0.009), specific cardiac complications from 21.0% (17 of 81) to 8.75% (7 of 80) (p=0.028), and neurological complications from 22.2% (18 of 81) to 6.25 % (5 out of 80) (p=0.004), in the structure of which the incidence of postoperative AMI was reduced from 3.7% (3 out of 81) to 1.25% (1 out of 80) (p=0.318), TIA - from 9, 9% (8 of 81) to 2.5% (2 of 80) (p=0.046) and stroke/stroke from 4.9% (4 of 81) to 0.0% (p=0.024). Mortality was reduced from 3.7% (3 out of 81) to 1.25% (1 out of 80) (p=0.307).
References
| [1] | Dai H, Much AA, Maor E, Asher E, Younis A, Xu Y, Lu Y, Liu X, Shu J, Bragazzi NL. Global, regional, and national burden of ischemic heart disease and its attributable risk factors, 1990-2017: results from the global Burden of Disease Study 2017. Eur Heart J Qual Care Clin Outcomes. 2020: qcaa076. |
| [2] | Nowbar AN, Gitto M, Howard JP, Francis DP, Al-Lamee R. Mortality From Ischemic Heart Disease. Circ Cardiovasc Qual Outcomes. 2019; 12(6): e005375. doi:10.1161/CIRCOUTCOMES.118.005375. |
| [3] | Bazylev V.V., Rosseikin E.V., Shmatkov M.G., Voevodin A.B. Results of one-stage open and hybrid surgeries for lesions of the coronary and carotid regions. FSBI "Federal Center for Cardiovascular Surgery", Cardiology and Cardiovascular Surgery. 2014; 4:33-38. |
| [4] | Mansurov A.A., Ilkhomov O.E., Khalikulov H.G. Modern aspects of surgical treatment of combined lesions of the coronary and brachiocephalic arteries. Surgery of Uzbekistan 2021, No. 4, 58-64. |
| [5] | Poslussny P., Gorlitzer M., Froschl A., Moidl R., Kaucky M., Weiss G. et al. Results of synchronous carotid endarterectomy and cardiac surgery: A single center experience. Thorac. Cardiovasc. Surg. 2013; 61:5. |
| [6] | Poi MJ, Echeverria A, Lin PH. Contemporary Management of Patients with Concomitant Coronary and Carotid Artery Disease. World J Surg. 2018; 42(1): 272-282. doi:10.1007/s00268-017-4103-7. |
| [7] | Feldman DN, Swaminathan RV, Geleris JD, Okin P, Minutello RM, Krishnan U, McCormick DJ, Bergman G, Singh H, Wong SC, Kim LK. Comparison of Trends and In-Hospital Outcomes of Concurrent Carotid Artery Revascularization and Coronary Artery Bypass Graft Surgery: The United States Experience 2004 to 2012. JACC Cardiovasc Interv. 2017; 10(3): 286-298. doi:10.1016/j.jcin.2016.11.032. |
| [8] | Oi K, Arai H. Stroke associated with coronary artery bypass grafting. Gen Thorac Cardiovasc Surg. 2015 Sep; 63(9): 487-95. doi: 10.1007/s11748-015-0572-5. |
| [9] | Taylor C, Walsh E, Stamm S. Synchronous CEA and CABG in asymptomatic carotid artery stenosis: A case study. J Vasc Nurs. 2019 Sep; 37(3): 194-198. doi:10.1016/j.jvn.2019.03.002. |
| [10] | Zhang J, Dong Z, Liu P, Fan X, Chen J, Zheng X, Ma B, Ye Z. Different Strategies in Simultaneous Coronary and Carotid Artery Revascularization - A Single Center Experience. Arch Iran Med. 2019 Mar 1; 22(3): 132-136. |
| [11] | Masabni K, Raza S, Blackstone EH, Gornik HL, Sabik JF 3rd. Does preoperative carotid stenosis screening reduce perioperative stroke in patients undergoing coronary artery bypass grafting? J Thorac Cardiovasc Surg. 2015; 149(5): 1253-60. doi: 10.1016/j.jtcvs.2015.02.003. |
| [12] | Shahian DM, He X, Jacobs JP, Kurlansky PA, et al. The Society of Thoracic Surgeons Composite Measure of Individual Surgeon Performance for Adult Cardiac Surgery: A Report of The Society of Thoracic Surgeons Quality Measurement Task Force. Ann Thorac Surg. 2015; 100(4): 1315-24; doi: 10.1016/j.athoracsur.2015.06.122. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML