-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(2): 172-178
doi:10.5923/j.ajmms.20221202.25
Received: Jan. 6, 2022; Accepted: Feb. 8, 2022; Published: Feb. 24, 2022

Algorithm of Clinical Typological Diagnosis of Symptomatology of Patients with Long-Term Concomitant Subdepression
Kuchimova Charos Azamatovna, Abdurazakova Robiya Sheralievna
Department of Psychiatry, Medical Psychology and Narcology, Samarkand State Medical Institute of the Republic of Uzbekistan
Correspondence to: Kuchimova Charos Azamatovna, Department of Psychiatry, Medical Psychology and Narcology, Samarkand State Medical Institute of the Republic of Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Nowadays, dysthymia, that is, prolonged subdepression, is considered to be a common hereditary disease, leading to the inability of patients to work in their youth periods to be isolated from the social environment. The reason for the deep beating of dysthymia is that the disease is almost as common as it is difficult to identify this pathology in the early stages. Because of the suicidal risk, prognostic evaluation, pathogenetic treatment, relevance of prophylaxis, difficult to differentiate variants, this pathology is widely covered in the scientific literature. At the same time, the nosological, clinical typological and syndromological problems of dysthymia are not studied fox, the tactics of choosing adequate therapy are difficult, this pathology is analyzed psychopathologically deeply and is interested in working on this topic.
Keywords: Prolonged subdepression, Affective disorders, Psychopathological system
Cite this paper: Kuchimova Charos Azamatovna, Abdurazakova Robiya Sheralievna, Algorithm of Clinical Typological Diagnosis of Symptomatology of Patients with Long-Term Concomitant Subdepression, American Journal of Medicine and Medical Sciences, Vol. 12 No. 2, 2022, pp. 172-178. doi: 10.5923/j.ajmms.20221202.25.
Article Outline
1. Introduction
- The urgency of prolonged subdepression is high, which often tends to be prolonged, i.e., chronic. When this condition is carefully analyzed psychopathologically, it will be possible to identify different options for the course, predict its consequences, and choose treatment tactics. The relevance of this study is the clinical and psychopathological system of long-term subdepression, nosological assessment, its role in the course of affective disorders, the definition of its consequences. In many countries, the number of depressive disorders has increased dramatically over the last 40 years, and by the end of the 21st century, depressive disorders will become a “major epidemic” and a global problem. According to data from the Harvard School of Health and the BJSS, depression was the fourth leading cause of illness in the 1990s, and by 2020 it was said to be second only to ischemic disease (J.L. Murray, A.D. Lopez, 1996). To date, the nosological differentiation of prolonged subdepression has been the subject of debate, indicating that insufficient research has been done on the problem. Some researchers exclude that this disorder falls into the framework of schizophrenia, which is not comparable to similar disorders in the structure of affective disorders. Other scientists, on the other hand, view prolonged subdepression as an exacerbation of a depressive condition, or do not draw a line between simple depressive and asthenic depression with shallow prolonged depression. Some researchers believe that shallow prolonged depression is a type of apathetic depression. Thus, the insufficient study of non-deep prolonged depression, the lack of a typological classification, is the basis for research on this disorder.
2. The Purpose of the Study
- To determine the clinical syndromology and typology of patients with long-term concomitant subdepression from a nosological background.
3. Research Tasks
- 1. To study the clinical-syndromological features of prolonged subdepression at its developmental stages;2. Development of subdepression typology;3. To determine the clinical typological features of subdepression observed with functional disorders;
4. Research Materials and Methods
- The study was conducted in 2019-2021 at the rukhi kasaliklar Hospital of Samarkand region. 70 patients were recruited for the study and these patients were selected based on the following criteria: the presence of depression at a non-psychotic level; the disease began at a young age (from 20 to 40 years of age); the duration of follow-up should be at a period of not less than two years; For the research material, the following cases are excluded: the absence of organic diseases of the central nervous system in the investigated patients, chronic alcoholism, toxicomania, severe somatic diseases, mental and behavioral disorders caused by the intake of psychoactive substances, drug addiction, mental retardation, symptoms of dopol diphtheria schizophrenia, psychotic disorders. The evaluation of dysthymia in expression and mental state in dynamics is based on clinical observations and the use of evaluation scales.
5. Research Results
- Based on the conducted study, a number of outstanding psychopathological features of dysthymia were determined. They include: prominent polymorphism in the clinical landscape, fragmentation, variability of psychopathological symptoms, uncertainty of the formation of Tri Triada. The analysis showed that the features of dysthymia in the examined patients and its specificity are explained by the psychobiological factors of pubertal and its formation, in which cognitive, behavioral, somatovegetative disorders characteristic of patients in the first place arise, in which the condition not only masks depression, but also makes it difficult to withstand the disease. Affektiv in connection with this, neurotic, non-depressive states, expressed by extremely valuable ideas and psychopathological disorders, cause difficulties. The link between the disease and the ontogenesis of youth eTap is much more difficult. With a long analysis of dysthymia, it becomes clear that the clinical picture is approaching depression, the classic depression triad and the typical ideator and motor components are relatively different. The structure of the depressive syndrome is clearly noticeable, the rudimentary nature of the thymic component attracts attention with the difference in the ratio of components in the clinic. Here, apato-adinamic component dominates (37,2%), less dysphoric (25,3%), panic (22,2%), sad (15,3%) components were observed.Apato-adinamic component negativity is characterized by the predominance of signs. With a decrease in the tone of life in the clinical landscape, the diphthesis of the tendons dominates. Stored activity masks the defect that has arisen (the external form of life and the nature of activity practically does not change), but all actions are carried out "automatically", "according to the habit", as if the guyoki infected its internal meaning. Since the apathicektekt is expressed, it is observed with the impoverishment of mimicry, monotony of speech, slowing of behavior. Dysthymia is observed from the fullness with the loss of all available desires, the inability to connect with the surrounding people, the prevalence of interest in the result of one's own activities. Self-perception with a change is contrasted with the disease from tusat. In apathic dysthymia (in contrast to melancholy), Vital disorders are observed with alienation symptoms, as well as with a state of hyperesthetic symptoms. All the time also do not plan to dominate the internal dyskomfort character, turbulence, hopelessness, tension associated with weakness. The priority (even if under the guise of indifference to the events of the surrounding world) is changed, theektekt comes out with a crush associated with the awareness of events in life. Adinamic disorders are accompanied by a predominance of negativity in the phenomenon of entrepreneurial contagion. In the clinical landscape is dominated by movement braking, adinemia, aspontanity, muscle stiffness. It is observed with an increase in muscle stiffness, weakness, burning desire and inclinations. When Apato-adinamik affekt prevails, the condition of patients is often misdiagnosed as apato-abulik syndrome in the debut of schizophrenia. In this case, unlike apato-abulic depression, motor braking, manifested in the eyes in patients, is not observed. In the clinical picture, when dysphoric affekt dominates, a pessimistic mood is observed with stubbornness, discontent with respect to oneself and others around, irritability, rapid irritability, psychomotor convulsions, aggression, this condition resembles psychopathic and psychopathetic symptoms from the outside. Usually dysphoric depression is accompanied by behavioral disorders, with antisocial behavior, disguised as a reading-related and social degradation, which makes it difficult to identify it on time. Patients in this group often deny depression in themselves, and their complaints are much sluggish, which makes it difficult to diagnose. When panic attacks dominate the clinical landscape of depression, they are accompanied by irritability, accelerated speech, motion convulsions and agitation. Bunda in some patients, panic is felt physically, and it can be said that this is a Vital character. In addition, in most patients, there is a changing panic, which is often expressed in the second half of the day. When grief dominates in the clinical landscape of depression, patients experience a decrease in tone, a decrease in energy, a feeling of discomfort in the psyche. At the same time, ideas of low self-assessment, pessimistic evaluation of the future, remembering unpleasant events in his life, the idea of extinction of the goal in the existence of humanity are observed, which in turn creates the ground for the formation of an extremely valuable depressive system. Other distinctive features of the clinical landscape of dysthymia are that movement braking is not observed. When assessing patients in a subset, there is some kind of divergence in their motor skills, an increase in movements. Motor braking slow down the pace of movement, mimic poverty, distress of facial expression only 10.5% of patients have migraines. In dysthymia, it is desirable to touch again on ideator disorders. These disorders almost tripled in all patients in different manifestations. Along with this symptomatology, it also irritates patients with memory and attention disorders, which can trigger mental processes from braking as well. From the peculiarities of dysthymia, high-frequency ideator disorders observed in pubertal crises are threeraydi.In the clinical landscape, depressive syndrome is observed clinical heterogeneity, which leads to a revision of the typology of the classification of dysthymia. In this case, most researchers identified a syndromological classification of depressive states, which served as an adequate diagnosis, outcome, treatment of dysthymia observed during adolescence [7,8,9,10]. The conducted study showed that almost all the syndrome symptoms of dysthymia were observed at a young age and were nomadic in the following variants: asthenic, dysmorphobic, psychopathetic, psychostenic, depersonalization, senesto – ipohondric variants. In addition, the clinical variants of negativity, which surpassed positivity in dysthymia, attracted attention.1. Asthenic depression (exhausted depression, neurasthenic melancholia). Among these options is 31.4%. Asthenia is one of the symptoms of depression. The most characteristic sign in the clinical picture is the predominance of cognitive signs (ideator braking, high intellektual fatigue, a decrease in the concentration of attention in mental activity, inability to read). In most cases, asthenia affektiv becomes a prodromal sign of violations. In the clinical picture of asthenic depression, which is clearly visible, there is a very high state of exhaustion, decreased activity, nausea, crying, physical weakness, energy exhaustion. Any effort to overcome weakness does not lead to a feeling of satisfaction. The feeling of fatigue is felt even in a slight movement. In patients with mild depression, the performance of tasks will be preserved, but observed with exhaustion. The specificity of depressive fatigue differs from ordinary fatigue in that muscle weakness is observed with a general violation of body sensitivity. Asthenia is characterized by stagnation and non-dependence on bullying. In much more pronounced depressions, patients find it difficult to perform the usual morning movements (washing, dressing, combing their hair). These actions will overwhelm the patients and require more time than usual. Impulsive weakness and asthenic hyperesthesia are observed, patients can not bear external influences (loud sound, strong light), a variety of sensations are observed in physiological processes. Sof the characters of the net are limited, grief, panic, self-discrimination, blame ideas will not be specific.2. In the dysmorphophobic variant of dysthymia (11,7%) there is a predominance of extremely valuable ideas, a lack of satisfaction from the outside. In the overwhelming majority of cases, the ideas of the sentimental relationship, which are observed with depersonalization disorders of the obsessive-phobic, senestoalgic and somatopsychic type of depersonalization, prevail.3. Dysthymia (angedonic variant-10,8%), accompanied by alienation of somatic inclinations, is observed with symptoms of the somatic circle (somatic equivalents of depression)-a complete loss of demand for sleep, depressive anorexia, a decrease in libido of the sexual inclinations to the loss of stools. Sleep disorders (short, interrupted sleep with difficulty waking up) reduction of the feeling of hunger acquires a Total character. Vomiting from food is observed with a refusal of food, and therefore in 1-2 weeks of the disease patients lose weight. In this case, the symptoms of pathological miscarriage (circadian rhythm and depressive braking) are limited to latent hypothymia. Also somatic equivalents, which are observed with alienation of somatic inclinations, do not determine the clinical picture of depression for a long time, most often they mean the origin of other types of affektiv disorders (vital Ipoochondric depression).4. In the psychopathetic variant (9,1%) of the clinical picture of dysthymia, psychopathetic disorders come to the first place, with these behavioral disorders, with basic movements, with symptoms similar to the symptoms of pathological occurrence of pubertal crizni, with oppositions to the attitude of the surrounding people, with the exclusion of conjunctivitis, with the inability to limit sexual inclinations, delinkvent is characterized by a tendency to Bunda is characterized by stubbornness, which is a typical component of a depressive Trida. Episodes of grief, panic, apathy are poorly observed, the sad mood is characterized by dysphoria.5. Psychasthenic variant (12,5%) of dysthymia is characterized by internal discomfort, with inability to enter into a relationship with surrounding people, with self-insecurity, with inability to make a decision that was not characteristic of patients before. With low mood in most patients, panic attacks prevail.6. Depressive symptomatology in depersonalization dysthymia (9,9%) is observed with severe dysphoric, less often with grief, panic. Signs of depersonalization are expressed mainly in the form of autopsychic depersonalization, psychological anesthesia.7. Obsessive-phobic disorders in dysthymia (7.9%) with predominant dysthymia, adhesive fears are observed with pessimismmga tendency. In most patients, fear predominates.8. In Senesto-ipohondric dysthymia (6,8%) affektiv disturbances are noted in the second place, and in the first place there are unpleasant, unpleasant, abnormal sensations in different parts of the body. The patient focuses his attention on his somatic state of mind and worries about his own health. Senestopathy seems to be part of depression and is diagnosed with a disease that can not be cured.Dysthymia is a psychopathological condition of the borderline level, observed with functional disorders of the cardiovascular system, is a theoretical and practical problem due to its wide prevalence. This is reflected in the uncertainty of the essence of the disorder and the abundance of its synonyms-cardieurosis, systemic cardiovascular neurosis, tension syndrome, Da Costa syndrome, vegetative-vascular dystonia, neuro-circulatory dystonia, neuro-circulatory asthenia, functional cardiovascular syndrome, etc. As shown in the works of leading local and foreign researchers in this area, this condition accounts for a large part of somatized mental disorders and mimics cardiovascular organic pathology. Such imitations are associated with functional cardiovascular and cerebrovascular disorders that prioritize groundbreaking clinical manifestations, and in fact they are incorrectly evaluated by doctors as signs of cardiovascular system disease, while they are symptoms of dysthymia. All this indicates the practical relevance of this problem. Its theoretical significance lies in the uncertainty of the clinical and pathogenetic nature of various functional cardiovascular diseases in dysthymia. Kompl 70 patients who were included in the material of our study during the examination were excluded from the study by cardiologists and neuropathologists with diseases of the cardiovascular system. Thus, patients with diseases of the cardiovascular system are not included in the study. Of the patients surveyed (94.1%) were previously listed as PND or treated in psychiatric hospitals, 2 patients (5.9%) were identified for the first time. A large percentage (80%) of the patients identified by US underwent a stationary examination. Of the 70 patients (46.2%) were men and (53.8%) were women. The majority of age-related observations suggest that 73.9% of patients were younger than 30 years of age, while patients were healthy and engaged in effective work in various social spheres.For a long time, all patients, on average, 2.5 years, were treated by therapists with an incorrect diagnosis of diseases of the non-invasive and unsuccessful cardiovascular system, repeatedly, on average, 3-4 times, hospitalized in the Cardiological, therapeutic, neurological and surgical departments. Patients had an average of 3-4 false positives indicating functional or organic pathology of the cardiovascular system. Cardioneurosis diagnoses have been ranked as the leading in 19.3% of cases, but they are combined with other misdiagnosed diagnoses mentioned above. At the time of the examination, somatisized psychopathological syndromes of nonpsychotic level (asthenic, ipohondric, somato-vegetative) were predominant in the group of 49 patients.
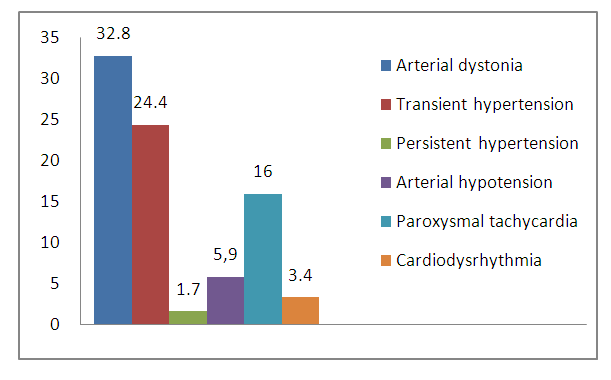 | Graph 1 |
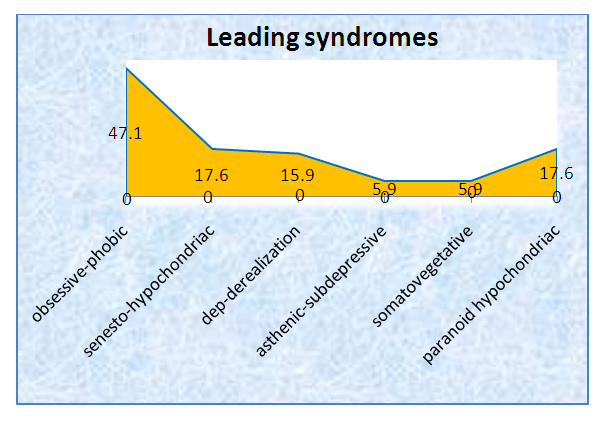 | Graph 2 |
6. Conclusions
- 1. Timely detection and treatment of dysthymia can prevent its spread and social degradation.2. In dysthymia, the typical component of the depressive triad is atypical and is most often observed with apato-adynamic symptoms (37,2%), less often with dysphoria (25,3%), with panic (22,2%), less often with sad mood symptoms.3. Taking into account the clinical phenomenological features of a special age, the following variants of Syndrome dysthymia were identified: asthenic variant, dysmorphobic variant, dysthymia, psychopathymic, psychostenic, depersonalization, senesto – ipohondric variants, accompanied by alienation of somatosesophageal inclinations.4. In the clinical picture of dysthymia is characteristic of unfinished polymorphism, fragmentation, variability of psychopathological symptoms, tri unclear formation of Triad, vegeto vascular disorders.5. In the status of patients with dysthymia, the leading ipohondrial-containing obsessive syndromes prevailed: obsessive-phobic (47.1%), senesto-ipohondric (17.6%), depersonalizacine-derealization (15.9%), asthenic subdepressive (5.9%), somato-vegetative subdepressive (5.9%). Only in 17.6% of cases paranoid-ipoxondric syndrome was observed in the upper depths of the disease coccyx.6. The clinical and social prognosis of dysthymia, primarily the dynamics of the pathological process, the tendency to maintain its activity or, conversely, the stability of recurrence, was determined.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML