-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(2): 148-151
doi:10.5923/j.ajmms.20221202.19
Received: Jan. 22, 2022; Accepted: Feb. 13, 2022; Published: Feb. 15, 2022

Comparative Evaluation of Conservative and Surgical Methods of Treatment of Patients with Hernias of the Lumbosacral Spine and the Search for Effective Methods of Rehabilitation
Ernazarov Alimardon Zhumakulovich1, Mavlyanova Zilola Farhadovna2, Burkhanova Gulnoza Lutfilloevna3
1Resident Doctor of the Rehabilitation Hospital of the Samarkand Region
2Head of the Department of Medical Rehabilitation, Sports Medicine and Traditional Medicine of the Samarkand State Medical Institute, Candidate of Medical Sciences
3Assistant of the Department of Medical Rehabilitation, Sports Medicine and Traditional Medicine, Samarkand State Medical Institute
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Improving the methods of treatment of patients with lumbosacral hernias based on the study and comparative evaluation of conservative and surgical methods with their subsequent rehabilitation. The spine is designed for loads. It supports and stabilizes the body in a standing position, providing complete freedom of movement. When lifting weights, uncomfortable body position, strong and stressful loads, he takes on the main effort. The load is especially pronounced when lifting heavy objects on outstretched arms. The strongest load and, accordingly, wear, falls precisely on the lumbar region. When age-related or pathological changes begin in the body, tissues change their structure and can no longer fully perform the functions of depreciation. Under the influence of force, they can be deformed, crumble, which disrupts the functions of the spine and can disrupt the functioning of the whole organism.
Keywords: Surgical treatment, Lumbar disc herniation, Meta-analysis, Non-surgical treatment, Structural view
Cite this paper: Ernazarov Alimardon Zhumakulovich, Mavlyanova Zilola Farhadovna, Burkhanova Gulnoza Lutfilloevna, Comparative Evaluation of Conservative and Surgical Methods of Treatment of Patients with Hernias of the Lumbosacral Spine and the Search for Effective Methods of Rehabilitation, American Journal of Medicine and Medical Sciences, Vol. 12 No. 2, 2022, pp. 148-151. doi: 10.5923/j.ajmms.20221202.19.
Article Outline
1. Introduction
- At the very beginning of the development of the pathological process, the patient does not feel serious pain, the symptoms are few. The more the tissues protrude, the more the patient feels it.Pain is the main symptom of a herniated disc. At first, not sharp, it can be aching, pass when changing the position of the body. The more serious the stage of the process, the stronger the pain. Backaches appear, it is painful for the patient to turn the body, the sensations intensify during physical exertion. spinal syndrome. Constant pain causes spasms of the muscles of the lower back. The patient cannot move fully, is forced to tilt the body in order to remove part of the load and reduce pain.Damage and death of the nerve roots due to constant compression. The compression that occurs due to the protrusion of tissues constantly affects the nerve fibers. From this, the blood flow, their functions are disturbed, and later death occurs altogether. The appearances of such a process are: weakness, decreased tone, loss of sensitivity, the appearance of body asymmetry, decreased sensitivity and skin tone.A total of 19 articles reviewed by 2272 participants met the joining criteria. Compared with non-surgical treatment, surgical treatment was more effective in reducing pain (short-term: mean difference = -0.94, 95% confidence interval = -1.87 to -0.00; interval: o ' mean difference = -1.59, 95% CI range = -2.24 to -9.94), improved function (interval: mean difference = -7.84, 95% confidence interval = - 14.00 to -1.68; long-term: mean difference = -12.21, 95% CI = -23.90 to -0.52) and quality of life. Physical function (short-term: mean difference = 6.25, 95% confidence interval = 0.43-12.08) and body pain (short-term: mean difference = 5.42, 95% confidence interval = 0.40-10, 45) Out of 36 items consisting of a short-term health check were also used. There was no significant difference in adverse events (mean difference = 0.82, 95% confidence interval = 0.28–2.38).With an athlete’s hernia, the posterior wall of the inguinal canal (transverse fascia) is weakened. In some athletes, rupture of the external oblique muscle aponeurosis is also observed. However, the most common finding in 85% of athletes with this syndrome is weakness in the posterior wall of the inguinal canal [16,20,21]. This pathology may not be observed in all cases; therefore, other pathologies such as enlargement of the outer ring, rupture of articular tendons, and divergence of inguinal ligaments should not be ignored. Clinical examination is important in the interpretation of conditions and pathologies such as osteitis pubis, rupture of the pubis ramus, bursitis, displacement of the pineal gland, acetabular injury, acetabular compression of the femur, and early osteoarthritis [22]. The examination should examine not only the pathology of the hip joint, but also potential damage to the rectus abdominis tendon or adductor long muscle. Pain in the lower and lateral parts of the inguinal ligament may indicate pathology of the hip joint or long joint muscle injury, and pain over the inguinal ligament may indicate pain associated with the athlete’s hernia.Several studies have compared the effectiveness of surgical and conservative treatment of patients with ischia-associated hernia of the lumbar spine, but methodological aspects limit the interpretation of their results. Follow-up cohort studies usually differ in important key prognostic variables in the treatment group, and their results are more prone to confounding. [12-14] Randomized controlled trials (RCTs) are less prone to confounding results. However, when comparing surgery with conservative treatment, the majority of patients randomly assigned to conservative treatment received surgery after randomization or after the initial period of conservative treatment (26–54%). operations, mainly in selected patients. In addition, some investigators question whether patients who wish to participate in surgical RCTs in connection with conservative treatment are typically patient representatives. seen in clinical practice.Features of a hernia are determined by its location. In this zone, the nerve roots are infringed and a characteristic clinical picture occurs. The nerve pinched during the formation of the lumbar protrusion of the spine runs along the inner surface of the leg from the thigh to the ankle. The pain is not necessarily localized along the entire length, it can be reflected in the leg, foot, buttock, outer side of the thigh. The lower back can also hurt at one point. With the development of the situation, the pain can move lower - to the lower leg, heel and toes. In intensity, it can be a constant aching pain or backache that occurs during movement.Basically, pain becomes more intense with prolonged walking, standing, turning the body, bending over. It also hurts to lift a leg, do a series of exercises, and also ride in vehicles on rough roads. At the beginning of the development of a hernia, pain can be relieved by lying down, bending one leg at the chest. This will help relieve tension and pressure on the nerve endings. In a more complex situation, this method will not help. Movements are constrained, their amplitude is greatly reduced, the leg gets tired. Basically, the patient feels compression of the spinal cord as tingling, burning, numbness. It dulls the pain. The main symptom that the specialist will pay attention to during examination is muscle tension on the lateral side of the back, painful when pressed.Athletic hernia is a pain syndrome in the lower abdomen. The reason it is called a sports hernia is because it was originally seen in athletes. However, it can also develop in people who do not exercise. In the last 4 decades, chronic apex pain in athletes has sometimes been described as an athlete's pelvic or groin disease - Gilmore's cola, and this is a recent hernia, groin disease, or whatever leads to chronic groin pain. athletic pub4algia [1]. There is no consensus on this situation, especially in terms of terminology (sports pubalgia, sports hernia, sports hernia, Gilmore's hernia, pubic-inguinal pain syndrome-PIPS, athlete's pelvis, player's pelvic injury complex, hockey player's syndrome, sports hernia); but the difficulty of diagnosis and treatment is accepted [2-4]. All these terminological differences define a well-understood complex of diseases, and general surgeons usually consider it a syndrome that does not require surgical intervention. Therefore, an insufficient number of clinical studies have been conducted [2]. The literature data presented so far on the etiology, pathogenesis, diagnosis and treatment of hernias in athletes are confusing. Many athletes, amateurs or professionals, are more likely to suffer from athlete betting than non-athletes [5]. Chronic groin pain often develops in athletes who twist and hit while running [6]. It is not uncommon for proximal thigh muscles or lower abdominal muscles to be seen in specially or heavily loaded sports branches. A "painful waist" is common in athletes who play football, rugby, Aussie football, cricket, skiing, long-distance or hurdling, and hockey. They are rare in sports such as basketball, tennis, cycling, and swimming because they are not associated with pivoting movements that lead to increased pelvic and joint pain [7,8]. Activity-limiting abdominal and groin pain accounts for 10–13% of all injuries per year among players [9,10]. This review aims to provide up-to-date information on chronic lower abdominal and groin pain, complexity and lack of consensus on treatment, as well as our own clinical experience and practice. Figure 1.
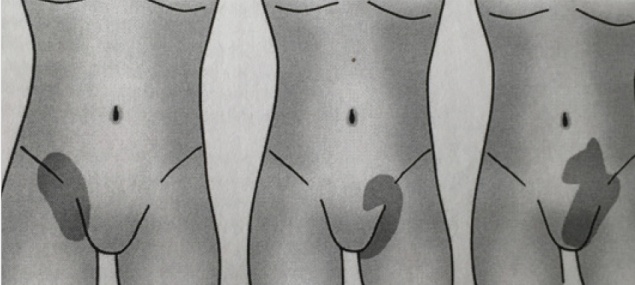 | Figure 1. Pain zones in sportsman’s hernia |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML