Botirov Farhod Kodirovich1, Mavlyanova Zilola Farhadovna2, Ravshanova Maftuna Zohidjonovna3
1Chief Physician of the Rehabilitation Hospital of the Samarkand Region
2Head of the Department of Medical Rehabilitation, Sports Medicine and Traditional Medicine of the Samarkand State Medical Institute, Candidate of Medical Sciences
3Assistant of the Department of Medical Rehabilitation, Sports Medicine and Traditional Medicine of the Samarkand State Medical Institute
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Increased prevalence of osteoarthritis of the knee (OA) and its impact on associated functional limitations, clinically and the need for scientific tools is growing. in the early stages of development. Traditional radiographic images remain the “gold standard” for the diagnosis of OA in the knee, but there is no sensitivity to detect the disease early. Development of evidence-based methods for organizing the provision of staged care, early diagnosis of osteoarthritis of the knee joints by studying the incidence, determining risk factors and regional characteristics in the Samarkand region.
Keywords:
Medical and social aspects, Diagnostic features, Immunological parameters, Osteoarthritis, Risk factors, Osteoarthritis of the knee
Cite this paper: Botirov Farhod Kodirovich, Mavlyanova Zilola Farhadovna, Ravshanova Maftuna Zohidjonovna, Organizational and Methodological Foundations for the Provision of Specialized Orthopedic (Therapeutic and Diagnostic) Care to Patients with Osteoarthritis of the Knee Joints with the Study of Regional Epidemiological Features, American Journal of Medicine and Medical Sciences, Vol. 12 No. 2, 2022, pp. 129-132. doi: 10.5923/j.ajmms.20221202.13.
1. Introduction
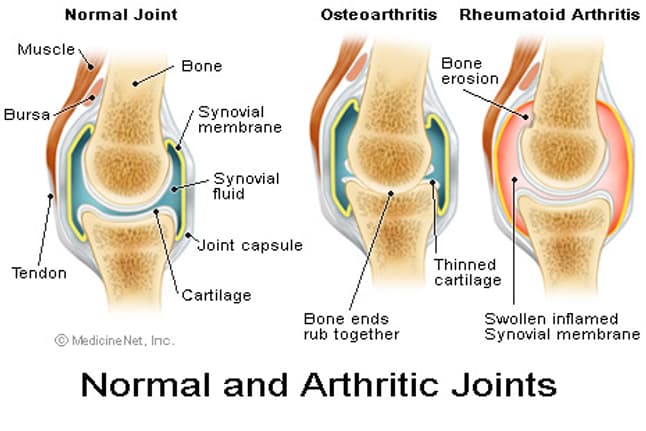
Osteoarthritis is more common in the elderly. Repeated use of your joints can damage the cartilage, leading to pain and swelling. Water accumulates in the cartilage and its proteins are broken down. It may begin to break down or take small tears. In severe cases, you can drop all the cartilage between the bones of the joint so that they rub against each other, making the joint difficult to use and painful. Cartilage damage can also cause bone growth (spurs) to form around your joints. Osteoarthritis sometimes occurs in more than one member of a family, indicating that the gene change has been passed from parent to child. In rare cases, these conditions are caused by problems with collagen, a hard protein found in your connective tissue.Classification systems have been developed that reliably determine the presence and severity of X-ray signs of knee. However, they are based on the presence or size of osteophytes and the degree of narrowing of the joint cavity assessed by human learners.Osteoarthritis (OA) is the most common joint disease in the United States. Symptomatic OA in the knee occurs in 10% of men and 13% of women aged 60 years and older. Due to the aging and obesity epidemic of the population, the number of people with symptomatic OA may increase. OA has a multifactorial etiology and can be considered as the result of an interaction of systemic and local factors. Old age, female gender, overweight and obesity, knee injury, recurrent joint use, bone density, muscle weakness, and arthritis are particularly stressful in the development of osteoarthritis of the joints. plays an important role in gins. Changing these factors reduces the risk of osteoarthritis and prevents subsequent pain and disability. The prevalence of symptomatic OA of the knee among adults 60 and older is approximately 10% in men and 13% in women. Due to the aging population and the obesity epidemic, the number of people with symptomatic OA may increase. Pain in OA is a major symptom and an important pre-disability factor in the decision to seek medical attention. Because of the prevalence and frequent disability that accompanies diseases of large joints such as the knee and hip, OA makes it more difficult to climb and walk stairs than other diseases. OA is also the most common cause of hip and knee arthroplasty. 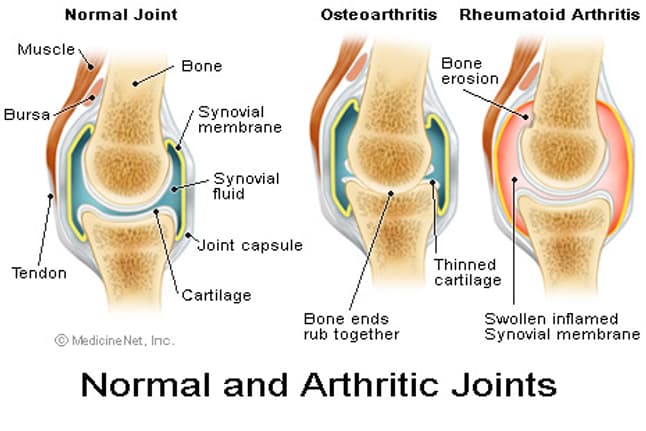 | Figure |
This rapid growth in the prevalence of an already prevalent disease indicates that OAs will become increasingly prevalent in the health and health care systems in the future. Epidemiological principles can be used to characterize the prevalence of OA in a population and to study risk factors for the development of OA. its origin and development. For epidemiological purposes, OA can be detected pathologically, radiologically, or clinically. Radiological OA has long been the standard of reference, and several methods have been developed to detect radiological disease. The most common method of radiographic identification is the Kellgren-Lawrence (K / L) radiographic classification scheme and atlas, which has been in use for more than forty years. This general joint scoring system evaluates OA on five levels from 0 to 4, indicating the presence of a specific osteophyte (≥2 degrees) in the OA and more severe levels in the joint space. narrowing, sclerosis, cysts, and an approximate sequence of deformities. Osteophytes and narrowing of the joint space to study the development of the disease or a measure of the width of the joint space in the knees and thighs directly between the bones as well as other radiographic measures such as semi-quantitative examination of individual radiological features such as direct measurement. epidemiological studies and clinical trials of disease-altering therapy. More sensitive imaging techniques using magnetic resonance imaging (MRI) can see multiple structures in the joint and are currently studying their role in detecting OA and the effects of interventions that change potentially faster than conventional radiographs. usefulness is being evaluated.. The study of OA in people with joint symptoms may be more clinically relevant because not all people with radiological OA have clinical disease, and not all people with joint symptoms have radiological OA. will not occur (12). Each set of clinical and radiological criteria may lead to slightly different groups of subjects with OA.OA is a degenerative joint disease involving the cartilage and many surrounding tissues. In addition to damage and loss of articular cartilage, remodeling of the submandibular bone, osteophyte formation, loosening of the ligaments, weakening of the periarticular muscles, and in some cases synovial inflammation are observed. 1 These changes can occur as a result of imbalances. between the breakdown and regeneration of joint tissue. Primary symptoms of OA include joint pain, stiffness, and limited mobility. The development of the disease is usually slow, but can eventually lead to joint failure along with pain and disability.OA can be defined as radiological, clinical, or subjective. There have been many attempts to accurately diagnose and evaluate radiological disease in OA, and it is the most widely evaluated in studies using the Kellgren and Lawrence (K&L) scores. The overall severity ranges from 0 to 4 and is associated with an approximate sequence of osteophytes, joint space loss, sclerosis, and cysts. 2 The World Health Organization (WHO) Adopted as a standard for epidemiological studies on OA. Cross-sectional imaging methods, such as magnetic resonance imaging (MRI), can show joint structures in more detail and continue evaluation to determine if they provide a tool to determine the definition of OA.Clinical OA is determined by features in the anamnesis and examination. It always requires the presence of joint pain in addition to other features. Some of the most well-known standards for the diagnosis of clinical OA are the criteria of the American College of Rheumatology (ACR). They are designed for number 3, knee 4, and arm. 5 Subjective OA relies on an assessment of whether the patient has the disease. Interestingly, individuals with early painful OA may be free of radiographic changes, and conversely, those with severe radiological changes may be completely asymptomatic. There is a correlation between the severity of radiographic disease and symptoms; but the association is not strong.The explanation for this poor compliance is, firstly, that some structures within the joint described on radiography do not have nociceptive innervation, and secondly, the sensation of pain may be more complex than responding to structural changes, e.g., other factors. psychological aspects also play an important role. The diagnosis of symptomatic radiographic OA is designed to take into account both structural changes and pain or discomfort in the joints.Osteoarthritis (OA) is the most common type of arthritis and is a serious health problem. Treatment of OA includes nonsteroidal anti-inflammatory drugs (NSAIDs), physiotherapy, and finally arthroplasty. The challenge in the clinical treatment of patients with OA is to predict the variable rate of the disease and which patients need intervention. Therefore, there is an important need for an algorithm that can classify patients with OA according to their level of developmental risk. short term. In addition, such an algorithm can be used to classify subjects to participate in clinical trials to develop additional treatment modalities. Statistical models have been developed in the OA literature to predict the rate and development of structural changes with the development of portable OA, but their use may be difficult due to the introduction of radiographic or genetic biomarkers, which require specialized equipment or personnel for assessment.Another potential biomarker for the systemic development of knee OA is the medial-lateral bone density ratio of the tibial plateau. This ratio can be obtained using two-way energy-absorbing X-ray (DXA) scanners, which are currently available for clinical imaging in many institutions. M: L BMD ratio can serve as a useful component of the prediction tool as it provides measurement of the bone below the knee and the measurement can be semi-automated. DXA studies of periarticular bone have shown that knee joints with localized OA have more BMD than those without knee joints. This difference is usually standardized as the approximate BMD ratio between the two sections. The use of this internal reference allows easy management of individual BMD changes [and the relationship is clear, with change factors ranging from 1 to 7%. M: L BMD ratio predicts knee OA severity and is strongly associated with joint space narrowing (JSN), osteophytes, and multiple sclerosis. X: X-ray sclerosis, measured for the M: L BMD ratio and the joint location of the area, suggests that both of these measurements may reflect a similar process. However, the M: L BMD ratio appears to be a more sensitive indicator of this process because it needs to be removed. radiographs that detect sclerosis on radiographs only partially weaken its contact with OA. In addition, the M: L BMD ratio is associated with subchondral pathologies such as bone marrow injury (associated with the development of OA). Two small longitudinal studies have shown that knee drop is associated with a decrease in the M: L BMD ratio, which also responds to changes in knee load.The algorithm for the treatment of patients with OA has its own characteristics. If in the vast majority of diseases, including non-rheumatic ones, the rehabilitation stage is preceded by outpatient or inpatient treatment, then in OA the algorithm looks different: rehabilitation - outpatient (less often - inpatient) treatment - rehabilitation. The use of pharmacotherapy in patients with OA is recommended only if rehabilitation measures are ineffective. Training and social support. Methods for teaching patients with OA do not differ from those for other diseases. For this purpose, special methodological manuals for patients are usually published, and video materials are prepared. In a popular presentation, patients receive information about the structure and function of the joints, the essence of the disease, modern and promising methods of treatment and prevention. These materials, aimed not only at the patient, but also at his relatives, can be distributed individually (attending physicians, social workers), as well as in self-help groups, which are usually created at large specialized clinics. Patient education programs such as the Arthritis Self-Help Course help patients reduce joint pain, maintain the function of affected joints, reduce doctor visits, and improve quality of life. A comparative meta-analysis of controlled studies of the effectiveness of training programs and the results of placebo-controlled studies of the effectiveness of NSAIDs showed that the former are only slightly inferior to the latter in terms of their effect on pain in OA. The involvement of spouses increases the effectiveness of work with patients. J. Goeppinger and co-authors (1995) noted that self-help programs distributed by mail helped patients - joint pain decreased, feelings of helplessness and depression disappeared. An important part of the work within the framework of educational programs is the creation of a positive optimistic attitude in patients towards their disease due to the fact that in the minds of most patients, joint diseases are associated with the inevitability of disability and a wheelchair. Despite the fact that the activities of the club are focused on the general contingent of rheumatological patients, the majority of those attending meetings are patients with joint diseases, in particular OA. Rheumatologists, physical therapy methodologists, physiotherapists, doctors of related specialties (orthopedists, etc.) give lectures at monthly meetings of club members. The presentations focus on simple ways of self-help that patients can use at home.Osteoarthritis (OA) is a debilitating and costly disease for all societies worldwide [1]. As people live longer and the population ages rapidly, these costs are constantly rising and OA is becoming an important issue that cannot be ignored. One way to reduce these costs is to detect OA early and, most importantly, predict it. To do this, it is necessary to develop new automated diagnostic and prognostic methods that will help medical professionals make decisions. Methods allow to identify patients on the path of development of OA. For these people, treatment for OA (eg, exercise, nutritional supplements, and lifestyle changes) can be started in a timely manner, reducing the impact of OA on quality of life and slowing down its progression [2]. Patients also benefit from participation in clinical trials of disease-modifying osteoarthritis (DMOAD) drugs such as strontium ranelate and bisphosphonates. Strontium ranelate has been found to reduce cartilage and bone pathology, while bisphosphonates prevent bone remodeling and maintain its structural integrity.The latest imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT), are commonly used in medical examinations. Classical radiological methods, although more than 100 years old, are inexpensive, fast, easy to use, and provide valuable information about changes in human bones. Current OA scoring is mainly based on joint atlas joint narrowing (JSN) and visual osteophyte classification such as the Osteoarthritis Research Society International (OARSI) atlas [6] or the Kellgren-Lawrence (KL) scoring scheme [7]. Individual assessment is time consuming, prone to high levels of internal and interval assessments, and is not sensitive enough to detect changes in the joints in the early stages of OA. For example, radiography has shown that approximately 11-13% of cartilage volume can be lost until primary JSN is observed, and a cartilage defect appears before radiographic OA or knee pain.A promising solution to this problem is the application of fractal analysis to textured radiographic images of trabecular bone (TB). The reasons for this are: (1) changes in tuberculosis in the early stages of OA. tuberculosis has a fractal character, i.e., it is similar on a number of scales (iii) selected TB tissue images on 2D radiographs are directly related to the 3D bone structure [8], and (iv) OA changes have been detected on TB tissue images using fractal techniques. In this study, we focus on OA in the knee and hand joints, as these are the joints most affected by the disease.
References
| [1] | Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000. |
| [2] | Hadler NM. Knee pain is the malady--not osteoarthritis. Ann Intern Med. 1992. |
| [3] | Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994. |
| [4] | DeFrances CJ, Podgornik MN. 2004 National Hospital Discharge Survey. Adv Data. 2006. |
| [5] | Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008. |
| [6] | D’Ambrosia RD. Epidemiology of osteoarthritis. Orthopedics. 2005. |
| [7] | Otte P. Gelenkerhaltung - Gefährdung - -Destruktion. Teil 1: Osteochondrale Strukturen. Nürnberg: Novartis; 2000. |
| [8] | Kellgren JH, Lawrence JS. Radiological assessment of osteoarthritis. Ann Rheum Dis. 1957. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML