-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(2): 96-103
doi:10.5923/j.ajmms.20221202.06
Received: Jan. 14, 2022; Accepted: Jan. 30, 2022; Published: Feb. 15, 2022

Assessment of the Effectiveness and Safety of Different Surgical Methods for the Treatment of Benign Prostate Hyperplasia by Adaptation of the Clavien-Dindo Classification
Sh. I. Giyasov1, 2, R. R. Gafarov3, Sh. T. Mukhtarov1, 2
1State Institution "Republican Specialized Scientific and Practical Medical Center of Urology", Uzbekistan
2Tashkent Medical Academy
3Samarkand State Medical Institute
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Benign prostatic hyperplasia (BPH) is a urological pathology in which surgery is the most effective treatment method and a very large number of methods of surgical interventions have been proposed. For example, in the United States of America, about 100,000 procedures are performed annually [1]. Historically, for a long time, the only effective method of treating BPH was open prostatectomy (adenomectomy) (OPE). Suprapubic or transvesical open prostatectomy was first performed in 1894 by Eugene Fuller and became widespread after the publication of the works of Peter Freyer (1900) [2]. According to the recommendations of the European Association of Urology (EAU) from 2020, open prostatectomy is the most invasive, and at the same time, the most effective method of treating BPH with a long-term effect.
Keywords: BPH, Complications, Systematization, Clavien-Dindo classification
Cite this paper: Sh. I. Giyasov, R. R. Gafarov, Sh. T. Mukhtarov, Assessment of the Effectiveness and Safety of Different Surgical Methods for the Treatment of Benign Prostate Hyperplasia by Adaptation of the Clavien-Dindo Classification, American Journal of Medicine and Medical Sciences, Vol. 12 No. 2, 2022, pp. 96-103. doi: 10.5923/j.ajmms.20221202.06.
1. Introduction
- After the introduction of endoscopic transurethral resection of BPH (TURP), this technique has remained the "gold standard" for surgical treatment of BPH for the last 40 years. It leads to a significant improvement in the quality of urination and the patient's life [3]. Nevertheless, TURP can also be accompanied by various complications, the most formidable among which are bleeding and TURP syndrome. The number and severity of these complications is in direct proportion to the volume of the gland, with an increase in which the morbidity also grows.Constant existing need to improve BPH surgery is the starting point for the progress of new technologies and, accordingly, the development of new methods of surgical treatment. The desire to combine the radical nature of the OPE with the minimally invasiveness of endourological interventions has opened a wide way for various options for endoscopic enucleation of the prostate (EEP). In 1998, a fundamentally new HoLEP (Holmium Laser Enucleation of the Prostate) technique appeared.An important landmark in the development of the HoLEP procedure was the creation and use of a morcellator in 1996. It is due to morcellation - the removal of large tissue fragments by means of their preliminary grinding in the bladder through a small diameter canal that it became possible to create that full-fledged holmium laser enucleation [4], which some authors call the new "gold standard" of BPH surgical treatment [5].It should be noted that today there is a transition from traditional operations for BPH in those centers where the appropriate level of technological and staffing to transurethral endoscopic interventions is possible. Thus, in accordance with the Recommendations of the European Association of Urology (EAU) from 2021 [6], OPE should be offered to patients with prostate volume >80 ml and moderate to severe low urinary tract symptoms (LUTS) if there is no possibility of performing bipolar transurethral enucleation of the prostate or holmium laser enucleation of the prostate.Nevertheless, in a number of countries, in those centers where there is no necessary equipment, or endourological techniques are at the stage of development, open adenomectomy remains a popular and necessary option for the surgical treatment of BPH. In addition, open surgery may be necessary in any urological center when BPH is combined with other urological pathology of the lower urinary tract, for example, with stones or bladder diverticulum [7,8].Practicing urologists know that complications of various severity may develop after any surgical intervention. Until now, among the medical community, including urologists, there is no consensus on how to identify complications and assess their severity correctly. This makes it difficult to make reliable and reproducible comparisons of different treatments at the same center, within a center in dynamics with passage of time; identical methods of treatment between centers using similar or different approaches. Therefore, a standardized classification of complications is needed, offering a common platform for interaction between urologists.In Uzbekistan, in recent years, high-tech, minimally invasive endoscopic methods of surgical treatment of BPH are being actively introduced in various state medical centers, private clinics, along with the traditional OPE. The simultaneous existence and use in practice of various methods of surgical treatment of the same disease, both in our Republic and in many other countries, proves the complexity, and still unresolved, optimal surgical method for treatment of this disease. This, in turn, depends on various reasons, one of which is the lack of an objective assessment of the quality of surgical methods.When performing both open and minimally invasive interventions for BPH, even by experienced surgeons, complications of both mild and severe severity are often observed. Severe complications can be life-threatening, and mild ones, exhausting the patient and disrupting his quality of life for a long time, even after getting rid of IVO (infravesical obstruction). All this must be recorded and monitored. Therefore, it is important to introduce a unified system for assessing the quality of interventions, which should be accepted by the urological community.The purpose of this study was an adaptation of the Clavien-Dindo classification to assessments of postoperative complications of surgical treatment of BPH and an assessment of the efficacy and safety of various surgical methods for treating BPH by systematizing postoperative complications.The Clavien-Dindo classification for systematizing postoperative complications is applicable to all types of surgical interventions, since, by its logic, it is universal [9,10]. But it is applicable to various methods of surgical treatment only after its adaptation, taking into account the specifics of the method.To achieve this goal, we set the following tasks:- to create criteria for the normal (standard) and complicated course of the postoperative period of surgical treatment of BPH and to adapt the Clavien-Dindo classification to the assessment of complications.- to study the nature, frequency and causes of postoperative complications of open adenomectomy, transurethral resection and holmium laser enucleation of BPH.- to systematize postoperative complications according to the adapted Clavien-Dindo classification for an objective assessment of the effectiveness and safety of various types of surgical treatment of BPH.
2. Material and Methods
- In accordance with the task, we retrospectively studied the case histories of 150 patients operated on for BPH. All patients were divided into three groups depending on the method of surgical treatment of prostatic hyperplasia. The first group consisted of 40 (26.7%) patients who underwent HoLEP (the period of mastering the new method). The second group consisted of 50 (33.3%) patients who underwent monopolar TURP (mTURP). The third group consisted of 60 (40%) patients who underwent open transvesical adenomectomy of the prostate (OPE), while hemostasis was carried out by tamponing the adenoma bed.Patients of the first group were operated on in the Republican Specialized Scientific and Practical Medical Center of Urology in Tashkent (RSSPMCU), the second and third groups - in the Samarkand branch of the Republican Research Centre Of Emergency Medicine (SB RRCEM). All operations were performed by experienced surgeons with many years of experience in this field, but HoLEP operations are the first results of the implementation phase of this technique.To adapt the classification to the assessment of postoperative complications of BPH surgical treatment and subsequently to systematize complications, we used the improved Clavien-Dindo classification of surgical complications [11]. To assess correctly the preoperative physical status of the patient, the classification of the American Society of Anesthesiologists (ASA - American Society of Anesthesiologists physical status classification system) [12].The results obtained in the course of the study were statistically processed. Mathematical analysis of the data obtained was carried out on a personal computer using the IBM IPSS Statistics 22 program, using Student's and Fisher's criteria. Differences were considered statistically significant at p <0.05.
3. Results
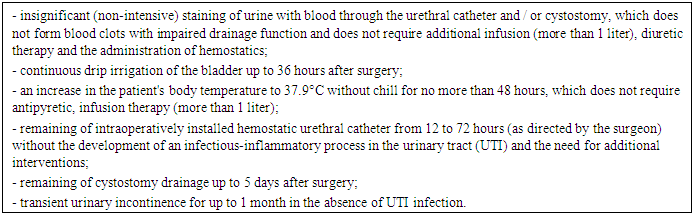
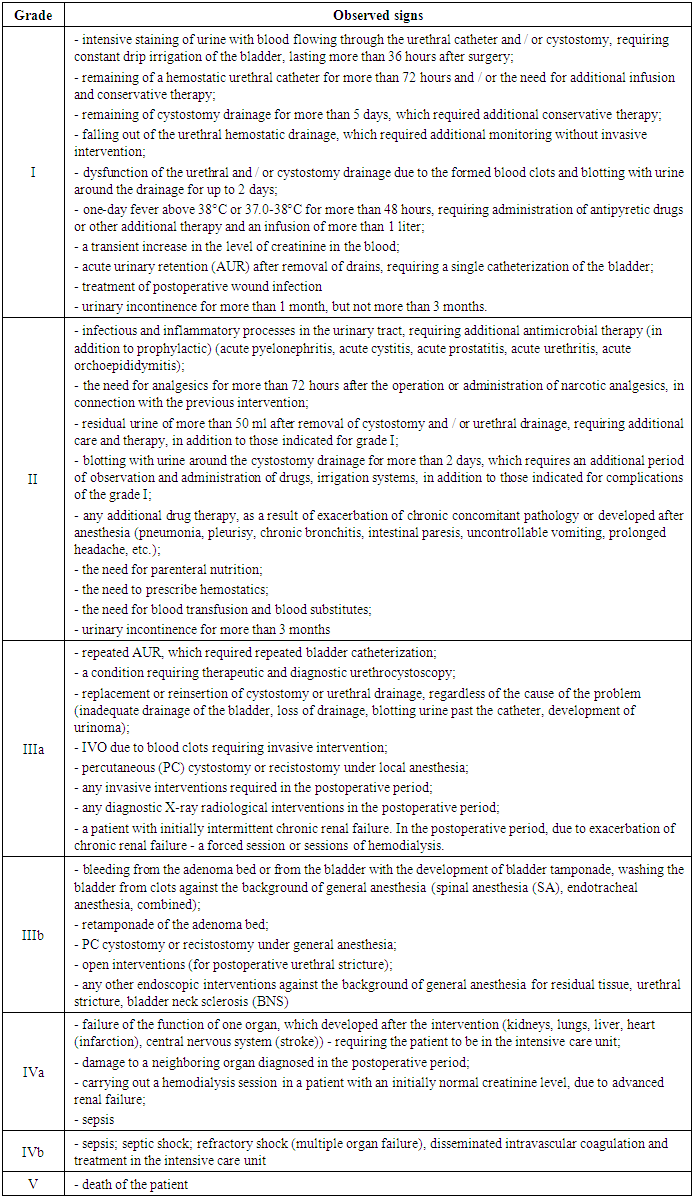
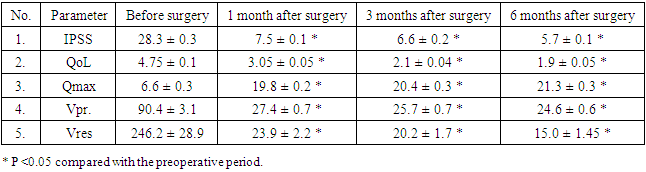
- We considered it necessary to create a unified standard for the postoperative course of surgical treatment of BPH as the first step to unify this classification. In our opinion, the created unified standard (normal course) of the postoperative period both for OPAE and for minimally invasive methods of surgical treatment of BPH will make it possible to assess objectively the quality of surgical intervention for BPH and reveal the disadvantages of one or another treatment method.Based on the many years of experience of our clinics in the treatment of BPH and postoperative management of patients, we have created criteria for the standard (normal), i.e. uncomplicated postoperative period, Table 1.
|
|
|
|
|
4. Discussion
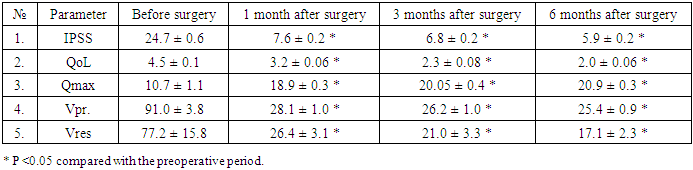
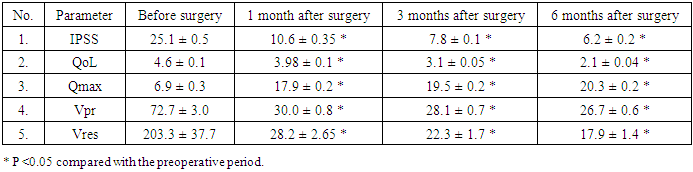
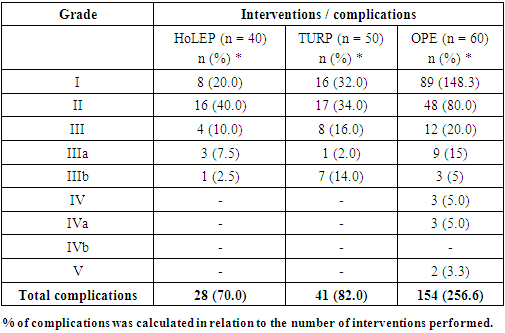
- After the publication of work on the systematization of complications [11], the Clavien-Dindo classification began to be used also in urology to assess postoperative complications, and in recent years it became popular due to its versatility. The reason for this is that the systematization of complications objectively shows the advantages of one method and the disadvantages of another, makes it possible to compare the quality of interventions of different surgeons, the results and effectiveness of treatment in different centers.There are data on the use of the classification system to assess the postoperative complications of radical retropubic, laparoscopic and robot-assisted prostatectomies [13,14,15], radical cystectomies [16,17], renal surgery [18,19]. In 2019 Sagen E. et al. [20], and in 2020 - Mbaeri T. et al. [21] applied a grading system to assess complications of transurethral resection of the prostate (TURP). In 2020 Yalçın S. et al. published data on the use of the Clavien system to assess complications of HoLEP [22].But on the other hand, the assessment of a particular postoperative complication differs among doctors, in different departments and centers due to some subjectivity in assessing complications, especially if it is performed directly by the surgeon who performed the operation. In order to assess the nature of complications, as well as to distribute them in relation to their severity according to the logic proposed by the authors of the classification, we must clearly distinguish between the normal and complicated course of the postoperative period. In the literature available to us regarding the surgical treatment of BPH, we did not find an analysis of this problem, which would clearly indicate the criteria for the normal and complicated course of the postoperative period in the treatment of BPH. Before, the criteria for the standard course of the postoperative period in relation to endoscopic treatment of nephrolithiasis were determined by the team of our Urology Center [23,24]. A number of authors who used the Clavien-Dindo classification in their work to assess postoperative complications in the treatment of BPH did not focus on this [19-22,25]. As a result, due to the lack of criteria for a standard postoperative course in the surgical treatment of BPH, the authors systematized complications in different centers in their own way. Some researchers considered some mild complications as a complication according to the classification logic, while others, the similar changes in the postoperative period, regarded as a normal postoperative course. Therefore, comparison of treatment results in one center turns out to be correct, but is not correct between centers.To eliminate such limitations with regard to surgical interventions performed for BPH, in particular for operations such as OPE, TURP and HoLEP, we made an attempt to adapt the Clavien-Dindo classification system to the above interventions, having previously determined which postoperative phenomenon is considered to be the norm and where the complication takes place. Some scientists may be of the opinion that the standard of the postoperative course for OPAE should differ from that for modern endoscopic methods of treatment, due to its trauma and peculiarities of postoperative management. However, this is an erroneous opinion, leading to the confusion of specialists in this matter. Surgical treatment of BPH, regardless of what method it will be carried out, pursues a single ultimate goal - getting rid of the patient from IVO by eliminating BPH. Therefore, treatment outcomes should be assessed by a single system for assessing the quality of interventions, regardless of which method or volume of intervention was used to achieve the goal.Comparison of complications obtained after systematization with literature data, where complications are given without systematization, do not always turn out to be correct, since with systematization, the detection rate of complications is always higher. According to Rassweiler J. et al. [26] as the technological and instrumental support of transurethral resection improved, the need for blood transfusion decreased to 0.4% versus the previous 7.1% (our indicator was 4%), the frequency of TUR syndrome is practically 0 (previously 1.1%) (we have 0), clotting obstruction is 2% (previously 5%) (we have 6%), urinary tract infection (BMI) - 1.7% (8.2%), (we have 8%). Retention of urine is 3% against the previous 9% (we have 4%). Late complications include urethral strictures 2.2-9.8% (we have 4%), sclerosis of the bladder neck 0.3-9.2% (we have 4%). Mortality after TURP is 0.0-0.025% (we have 0).When comparing TURP and HoLEP techniques in a meta-analysis, Ahyai SA et al. [27] revealed the following features: in none of the cases when performing HoLEP blood transfusion was required, while after TURP the frequency of blood transfusion was 2.2% (we have 4% and 2.5%); the time of catheterization after HoLEP varied from 17.7 to 31 hours, and after TURP - from 43.4 to 57.8 hours (we also have less than 3 days after both methods); the duration of hospitalization after laser enucleation averaged 2-3 days, and after TURP - 3-6 days [28], this indicator among our patients was 4.95 and 4.0.In a prospective multicenter study of Bozzini G. et al. [29], which compared ThuLEP and HoLEP with a 12-month follow-up period, there were no significant differences in treatment efficacy.In a retrospective study comparing the techniques of OPE and ThuFLEP (Thulium fiber laser enucleation of the prostate), it was found that OPE is characterized by a large number of complications, a long hospital stay and a late return to daily activity [30], which we also confirmed in our study. OPE is characterized by high morbidity and a large number of postoperative complications. The mortality rate for European countries is about 0.25%. The overall percentage of complications in the late 90s ranged from 12.5-23.02%, by the second decade of the 21st century it was 17.3% [5,31-34].An interesting fact is that our analysis of the effectiveness of treatment for all three methods of surgery based on IPSS, QoL, Qmax, Vpr. and Vres parameters (Tables 3,4,5) demonstrated that all indicators were significantly different compared to the initial parameters and all methods of surgical treatment can be regarded as effective, with a relative difference in the timing of improvement in IPSS scores and the quality of life of patients, which occurred 1-2 months later after TURP. But, only after systematization of postoperative complications with the help of the adapted classification, it was possible to reveal the real picture of the features of the postoperative period of each method of treatment.
5. Conclusions
- 1. Postoperative values of IPSS, QoL, Qmax, PVR indicators after OPE show more marked positive dynamics as early as 1 month after the intervention, which is practically comparable to that after HoLEP. Similar results after TURP are achieved only 3 months after the intervention due to the severity of dysuria, which affects the IPSS and QoL scores.2. OPE is characterized by a significantly longer hospitalization period compared to TURP and HoLEP (8,6±0,3 versus 3,3±0,2 versus 3,8±0,2, respectively), longer residence time of the urethral catheter (8.4±0.3 versus 2.9±0.1 versus 2,2±0,1) and more prolonged hematuria (3.8±0.3 versus 1.35±0.6 versus 1.2±0.08), more severe complications, significantly more often requiring additional interventions.3. In terms of trauma, frequency of blood transfusions and length of hospital stay, the results of TURP are comparable to HoLEP. The terms of restoration of the quality of life of patients with urodynamic parameters in the first three months after TURP are worse than after HoLEP. Fibrosclerotic changes in the urethra and bladder neck with the development of IVO once again, requiring repeated surgical interventions, are also significantly more often observed.4. Systematization of the postoperative complications of HoLEP, TURP and OPE according to the adapted Clavien-Dindo classification makes it possible to assess objectively the quality of interventions separately and determine their safety in a comparative aspect.
References
| [1] | Huang SW, Tsai CY, Tseng CS, Shih MC, Yeh YC, Chien KL, Pu YS, Tu YK. Comparative efficacy and safety of new surgical treatments for benign prostatic hyperplasia: systematic review and network meta-analysis. BMJ. 2019 Nov 14; 367: l5919. doi: 10.1136/bmj.l5919. PMID: 31727627; PMCID: PMC7223639. |
| [2] | Freyer PG. A new method of performing prostatectomy. Lancet: 1900; 1: 774. |
| [3] | Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, Lack N, Stief CG; Urology Section of the Bavarian Working Group for Quality Assurance. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008 Jul; 180 (1): 246-9. doi: 10.1016/j.juro.2008.03.058. Epub 2008 May 21. PMID: 18499179. |
| [4] | Gilling, PJ, & Fraundorfer, MR (1998). Holmium laser prostatectomy: a technique in evolution. Current opinion in urology, 8 (1), 11-15. |
| [5] | Michalak J, Tzou D, Funk J. HoLEP: the gold standard for the surgical management of BPH in the 21 (st) Century. Am J Clin Exp Urol. 2015 Apr 25; 3 (1): 36-42. PMID: 26069886; PMCID: PMC4446381. |
| [6] | EAU Guidelines. Edn. presented at the EAU Annual Congress Milan 2021. ISBN 978-94-92671-13-4. |
| [7] | Enikeev D, Okhunov Z, Rapoport L, Taratkin M, Enikeev M, Snurnitsyna O, Capretz T, Inoyatov J, Glybochko P. Novel Thulium Fiber Laser for Enucleation of Prostate: A Retrospective Comparison with Open Simple Prostatectomy. J Endourol. 2019 Jan; 33 (1): 16-21. doi: 10.1089/end.2018.0791. PMID: 30489154. |
| [8] | Peshekhonov KS, Shpilenia ES, Komyakov BK, Burlaka OO, Sargsyan MS Endoscopic treatment of prostatic hyperplasia in elderly patients: a comparative analysis of resection and enucleation technique. Urology Herald. 2020; 8 (1): 25-38. (In Russ.). https://doi.org/10.21886/2308-6424-2020-8-1-25-38... |
| [9] | Dindo D., Demartines N., Clavien PA Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery. 2004; 240: 205-13. DOI: 10.1097/01.sla.0000133083.54934.ae. |
| [10] | Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien- Dindo classification of surgical complications: five-year experience. Ann Surg. 2009 Aug; 250 (2): 187-96. doi: 10.1097/SLA.0b013e3181b13ca2. PMID: 19638912. |
| [11] | Dindo D., Demartines N., Clavien PA Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery. 2004; 240: 205-13. DOI: 10.1097/01.sla.0000133083.54934.ae. |
| [12] | De Cassai A, Boscolo A, Tonetti T, Ban I, Ori C. Assignment of ASA-physical status relates to anesthesiologists' experience: a survey-based national-study. Korean J Anesthesiol. 2019 Feb; 72 (1): 53-59. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML