-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(1): 57-61
doi:10.5923/j.ajmms.20221201.11
Received: Jan. 1, 2022; Accepted: Jan. 17, 2022; Published: Jan. 27, 2022

Effectiveness of the Infusion Medical Drug "Reoambrasol" in Experimental Methemoglobinemia
Larisa Ivanovna Shevchenko1, Dildora Zabixullayevna Khakimova2, Jamoliddin Djololovich Khuzhakhmedov3, Khamid Yakubovich Karimov1
1Department of Molecular Medicine and Cellular Technologies, Republican Specialized Scientific-Practical Medical Center of Hematology MoH RUz, Tashkent, Republic of Uzbekistan
2Clinic, Tashkent Medical Academy MoH RUz, Tashkent, Republic of Uzbekistan
3«GenoTexnologiya» Molecular Genetics Laboratory, Tashkent, Republic of Uzbekistan
Correspondence to: Dildora Zabixullayevna Khakimova, Clinic, Tashkent Medical Academy MoH RUz, Tashkent, Republic of Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

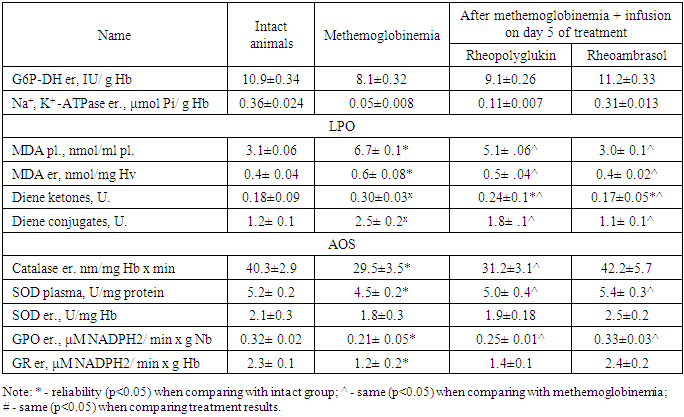
Experimental toxic methemoglobinemia was performed on 100 male rats weighing 190-220 grams by daily injection of sodium nitrite at a dose of 50 mg/kg for 30 days. In the blood of rat were studied content of methemoglobin (metHb), the level of total hemoglobin, the activity of Na+, K+ -ATPase, glucose-6-phosphate dehydrogenase (G6P-DH), the blood content of lipid peroxidation products (MDA, diene ketones, diene conjugates), as well as the activity of antioxidant system enzymes (catalase (CT), superoxide dismutase (SOD), glutathione peroxidase (GPO), glutathione reductase (GR)). The results showed that in nitrite methemoglobinemia metHb content in the blood of experimental animals already increased in the first hours after the start of the experiment. Corrective action of “Rheoambrasol” on the activity of peroxidation and the activity of antioxidant protection enzymes under conditions of methemoglobinemia caused by prolonged nitrite intoxication was established. The use of “Rheoambrasol” at methemoglobinemia has a distinct restorative activity on G6P-DH and enzyme Na+, K+ -ATPase, thereby showing membrane-stabilizing effect.
Keywords: Experimental toxic methemoglobinemia, Methemoglobin, Glucose-6-phosphate dehydrogenase, Lipid peroxidation, Antioxidant system
Cite this paper: Larisa Ivanovna Shevchenko, Dildora Zabixullayevna Khakimova, Jamoliddin Djololovich Khuzhakhmedov, Khamid Yakubovich Karimov, Effectiveness of the Infusion Medical Drug "Reoambrasol" in Experimental Methemoglobinemia, American Journal of Medicine and Medical Sciences, Vol. 12 No. 1, 2022, pp. 57-61. doi: 10.5923/j.ajmms.20221201.11.
Article Outline
1. Introduction
- Penetration into the body of various cytotoxic xenobiotics, which includes sodium nitrite, leads to hypoxia, disruption of oxidative and energy homeostasis [6,11]. Already in the body sodium nitrite promotes the formation of methemoglobin by direct action on hemoglobin, and by damaging the biological systems responsible for the recovery of methemoglobin, or both ways simultaneously [1,2,7]. Its action on the body based on the oxidation of hemic iron from divalent to trivalent (Fe2+ to Fe3+) and disruption of respiratory enzymes, which causes the development of mixed type hypoxia and disturbance of functional properties of red blood cells. Regardless of the type of hypoxia, the characteristic disorders are based on the activation of free-radical processes which in methemoglobinemia lead to prolonged suppression of membrane-associated and adenosine triphosphate (ATP)-dependent enzyme activity - Na+, K+ -ATP-ase. (Filippova O.N. et al. 2005) [5].To restore these consequences of methemoglobinemia, we propose a new drug "Rheoambrasol", which has antihypoxic, antioxidant action, able to restore cell metabolism in conditions of hypoxia [13].
2. Main Body
2.1. The Purpose of Our Research
- The purpose of this work is to study the effect of the new drug «Rheoambrasol»» on the activity of lipid peroxidation, antioxidant protection and Na+, K+ -ATPase, in nitrite methemoglobinemia.
2.2. Material and Methods of Study
- The experiments were carried out on the basis of vivarium of the Interuniversity research laboratory of the Tashkent Medical Academy (TMA). 100 male rats weighing 190-220 grams were involved in the experiment.. Toxic methemoglobinemia in rats was created by daily injection of sodium nitrite at a dose of 50 mg/kg for 30 days [6]. The severity of the animals' condition during the experiment was determined according to the criteria proposed by Ivanitskaya N.F. (1976).During the staging of the methemoglobinemia model, methemoglobin (metHb) content was determined after sodium nitrite injection after 1.5 hours, on the 3rd, 15th, and 30th days. Was started methemoglobinemia, on the 30th day after treatment.Were treated animals for 5 days with blood substitutes: the new blood substitute "Rheoambrasol" in the experimental group and the preparation "Rheopolyglukin" in the comparison group. Were administered blood substituteS infusion drugs at a dose of 10 ml/kg.Were divided animals into the following groups: Group I - pre-methemoglobinema (intact) (n=15); Group II (control) - with methemoglobinemia without treatment;Group III (comparison) - with «Rheopolyglukin» infusion on the 30th day after sodium nitrite injection;IIIa) subgroup - 1 hour after treatment n=13;IIIb) subgroup - on the 5th day after treatment, n=12;Group IV (main, experimental) - with «Rheoambrasol» infusion on the 30th day after sodium nitrite injection;IVa) subgroup - 1 hour after treatment, n=14;IVb) subgroup - on the 5th day after treatment, n=14.Laboratory studies were carried out on the basis of "Laboratory of blood substitutes" of the Republican Specialized Scientific-Practical Medical Center of Hematology (RSSPMCH).In all animals the level of metHb was determined by spectrophotometry according to Volchkov A.B. et al. (2002), by a single measurement of the optical density (OD) of the blood solution followed by calculation of metHb content according to the formula [17].The level of total hemoglobin was determined by the hemoglobin cyanide method using HUMAN kits (Germany), according to the instructions provided with the kit. Reaction results were measured on a BA88A semi-automatic biochemical analyzer (Mindray, China).ATPase activity was studied according to the method of A.M. Kazzenov and co-authors [8]. erythrocytes were washed 3 times with 0.145 mM NaCl, 10mM Tris-HCl buffer (pH 7.4) and treated with 1% tween 20 in 0.25 M sucrose on Tris-HCl buffer (volume 1:1, exposure: 60 min at 20°C). Na+, K+ -ATPase activity was calculated from the growth of inorganic phosphorus (Fn, sensitivity 0.01 μM) in the incubation medium and calculated from the difference between ATPase activity without and in the presence of inhibitor - 1 mM ouabain. The activity was expressed in μmol Fn per ml of cells (taking into account hematocrit of prepared erythrocyte suspension). The following reagents were used: EDTA, ATP, and ouabain (Sigma) and other reagents (Russia). The activity of Na+, K+ -ATPase, in blood was determined in μmol Pi/g Hb.The activity of erythrocyte glucose-6-phosphate dehydrogenase (G6P-DH) was determined according to a common method [18].The content of lipid peroxidation products (MDA, diene ketones, diene conjugates) was determined according to the method of G.R. Titeeva and N.N. Korovina [15] using TBK-AGAT kit ("Agat-Med", Russia). Products were calculated using molar extinction coefficient and expressed in nmol/mg. Diene conjugates and diene ketones were determined in hexane extracts of blood serum (1996) [3].The activity of catalase (CT) in blood was determined by the method of M.A. Korolyuk et al. (1998) [9,10], the principle of which is based on the ability of H2O2 to form a stable colored complex with molybdenum salts. Measurements were performed at a wavelength of 410 nm. An enzymatic unit (U) was the amount of enzyme necessary to convert 1 µmol of substrate in 1 min at 25°С.Superoxide dismutase (SOD) activity was determined according to the method of V.G. Mkhitryan et al. (1978) [12]. The activity was calculated by the percentage of inhibition (Т%) of tetrazolium blue reduction in alkaline medium. The unit of SOD activity (U) was taken to be the amount of the enzyme required for the 50% inhibition of nitroblue tetrazolium reduction in the non-enzymatic system of phenazine methanesulfate and NADN. The activity of the enzyme was expressed in units/min x mg of protein. Superoxide dismutase (SOD) activity in erythrocytes was expressed in units/min x mg Hb [4]. Purified SOD preparation (ICN Biomedicals, USA) was used as a standard [14].The activity of glutathione peroxidase (GPO) was determined by the accumulation of oxidized glutathione (GSSG) as a result of lipoperoxide decomposition. The activity of the enzyme was expressed in units/min x mg Hb per min. Activity of erythrocyte glutathione reductase (GR) was determined in reaction medium of phosphate buffer at wavelength 340 nm and by the decrease of NADPH*H and expressed in µM NADPH2/min x g Hb (Vlasova S.N. et al., 1990) [16].Measurements were performed on a ”UNICO2800” spectrophotometer (United products and instruments, Inc., USA).The results were statistically processed using Student's t-test. Differences were considered statistically significant when the p-criterion value was less than or equal to 0.05.
2.3. Results of the Study
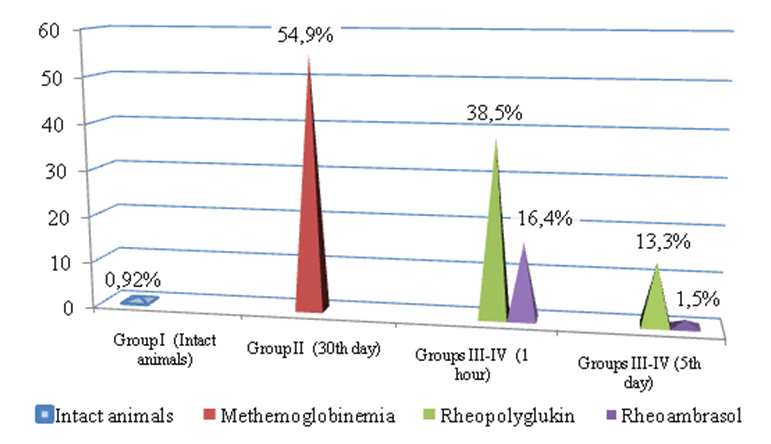
- The results of the study showed that during nitrite methemoglobinemia, the content of metHb in the blood of experimental animals already increased in the first hours after the beginning of the experiment. Figure 1 shows data on the amount of methemoglobin in the blood during nitrite methemoglobinemia and after the application of blood substitutes (Fig. 1).
3. Conclusions
- Corrective effect of «Rheoambrasol» on the activity of peroxidation and the activity of antioxidant protection enzymes under conditions of methemoglobinemia caused by prolonged nitrite intoxication was established.The use of «Rheoambrasol» at methemoglobinemia has a distinct restorative activity on G6P-DH and enzyme Na+, K+ -ATPase, thereby exhibiting membrane stabilizing effect.
References
| [1] | Abrasheva M.V., Andreyeva A.I., Vinogradova O.Ye., Viktorovich N.N. Erythrocyte hemoglobin: types, meanings, alternative and additional functions. Mezhdunarodnyy zhurnal prikladnykh i fundamental'nykh issledovaniy, 2021; 7: 7-11. |
| [2] | Aleksandrova E.V., Belenkiy S.A., Shvets V.N., Krisanova N.V., Makoed O.B., Shkoda A.S. Chromoproteins: structure, properties and functions. Hemoglobin metabolism and its disturbances; 2015: 1-75. |
| [3] | Andreyeva L.I, Kozhemyakin L.A., Kishkun A.A. Modification of the method for determining lipid peroxides in the test with thiobarbituric acid. Laboratornoye delo. 1988; 11: 41–43. |
| [4] | Brusov O. S., Gerasimov A. M., Panchenko L. F. Effect of natural inhibitors of free radical reactions on adrenalin autoxidation // Bulletin of Experimental Biology and Medicine. – 1976. – Т. 81. – №. 1. – С. 39-41. |
| [5] | Filippova O.N., Shperling I.A., Ryazantseva N.V., Rogov O.A., Akimova V.V., Bas V.V. Na+, K+ -ATPase activity in erythrocytes in hemolytic anemia. Fundamental'nyye issledovaniya, 2005; 5: 116-116. |
| [6] | Igbayev R.K. Experimental correction of prooxidant-antioxidant equilibrium under conditions of hypoxia and toxic methemoglobinemia: thesis. … PhD med. nauk – Ufa-2006, Bashkirskiy gosudarstvennyy meditsinskiy universitet: 1-164. |
| [7] | Katabami K., Hayakawa M., Gando S. Severe methemoglobinemia due to sodium nitrite poisoning. Case reports in emergency medicine, 2016: 1-3. |
| [8] | Kazennov A.M., Maslova M.N., Shalabodov A.D. Study of Na+, K+ -ATPase activity in mammalian erythrocytes. Biokhimiya. 1984; 49(7): 1080-1094. |
| [9] | Korolyuk M.A. Ivanova L.K., Mayorova I.G., Tokareva V.A. Method for determining the activity of catalase. Laboratornoye delo. 1988; 4: 44-47. |
| [10] | Korolyuk M.A., Ivanova L.I., Mayorova I.G., Tokarev V. Ye. Method for determining the activity of catalase. Klinicheskaya laboratornaya diagnostika, 1988; 1:16-19. |
| [11] | Kozayeva E.G. Influence of experimental nitrite and nitrate intoxication on renal function in rats.: avtoref. thesis. .. PhD. med. nauk. – Vladikavkaz – 2011 GOU VPO «Severo-Osetinskaya gosudarstvennaya meditsinskaya akademiya» Min. Zdrav. i Sots. razvitiya RF: 1-22. |
| [12] | Mkhitaryan V.G., Badalyan G. Ye. Influence of peroxidized and non-peroxidized unsaturated fatty acids on superoxide dismutase activity. Էքսպերիմենտալ և կլինիկական բժշկության հանդես. 1978; 18(6): 7-12. |
| [13] | Shevchenko L.I., Karimov Kh. Ya., Rakhmanberdiyeva R.K., Sagdullayev SH. SH. Polyfunctional blood substitute of hemodynamic action. Patent IAP 06029 ot 28. 10. 2015. Rasmiy akhborotnoma, 2019; 11(223): 59-59. |
| [14] | Tietz W.B Clinical guide to laboratory tests. 4-th ed. Ed. Wu A.N.B. USA, Sounders Company, 2006: 1-1798. |
| [15] | Titeyeva G.R., Korovina N.N. Lipid peroxidation: norm and pathology. Tsentral'no-Aziatskiy med. zhurnal, 1996; 4: 78-84. |
| [16] | Vlasova S.N. The activity of glutathione-dependent erythrocyte enzymes in chronic liver diseases in children. Lab. Delo 1990; (8): 19-22. |
| [17] | Volchkov A.B. Yerykalov M.YU. Lyubimova L.V. Method for determining the concentration of methemoglobin in the blood / Pat. 2186397. Rossiyskaya federatsiya, MPK7 G 01 N 33/72, G 01 N 33/49.; zayavitel' i patentoobladatel' Volchkov A. B. № 2000114327/14; zayavl. 05.06.2000; opubl. 27.07. 2002: 1-5. |
| [18] | Zakharin Yu.L. Metod opredeleniya glyukozo-6-fosfatdegidrogenazy i 6-fosfoglyukonatdegidrogenazy. V: Laboratornoye delo. 1967; 6: 327-330. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML