-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(1): 12-17
doi:10.5923/j.ajmms.20221201.03
Received: Dec. 16, 2021; Accepted: Jan. 7, 2022; Published: Jan. 13, 2022

Acute Pancreatitis: New Perspectives on Treatment
Khakimov M. Sh., Asatullaev J. R., Fayzullaev B. B., Mukhammadiev M. Kh., Asanov B. P., Radjabov A. I.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Examination and treatment results of 432 patients with various forms of pancreatic necrosis were analyzed in the article. 244 patients were performed traditional treatment. 188 patients were treated according to our developments. The conducted studies allowed us to specify the timing of the onset of the sequestration phase. The authors divided the initiated form of pancreatic necrosis into infiltrative and sequestered, according to which adjustments were made to the therapeutic tactics of pancreatic necrosis. The classification of the disease has been improved on the base of the conducted studies. The conducted studies have significantly reduced the proportion of surgical treatment of pancreatic necrosis from 25.0% to 12.2% and mortality - from 12.3% to 6.9%.
Keywords: Sequestration phase, Infected pancreatic necrosis, Classification
Cite this paper: Khakimov M. Sh., Asatullaev J. R., Fayzullaev B. B., Mukhammadiev M. Kh., Asanov B. P., Radjabov A. I., Acute Pancreatitis: New Perspectives on Treatment, American Journal of Medicine and Medical Sciences, Vol. 12 No. 1, 2022, pp. 12-17. doi: 10.5923/j.ajmms.20221201.03.
1. Introduction
- The treatment of destructive forms of acute pancreatitis (AP) is one of the most difficult problems in urgent abdominal surgery and is still the subject of lively discussions. Despite the achievements of modern medicine and accumulated practical experience in pancreatology, many problems associated with adequate therapeutic tactics for AP and its complications remain unresolved. In particular, this concerns issues related to the classification of the disease, processes occurring in the pancreas [1-3].The classification of AP is one of the most controversial issues in emergency surgery. In spite of the widespread popularity of the international classification of AP Atlanta-92 and its repeated additions, it does not suit a number of practical surgeons in the existing version. the Russian Society of Surgeons proposed the classification of AP in 2014, which is based on a multi-system approach, consisting of the assessment of morphological and functional changes in pancreas and retroperitoneal tissue, taking into account the emerging local and systemic complications [1].The lack of consideration of the phase of AP course and clearly formulated protocols for various clinical situations where the reason for the development of the classification, which was based on the work of V. I. Filin "Phases and clinical forms of acute pancreatitis. Therapeutic tactics was chosen depending on the clinical phases of AP, which was mainly determined empirically based on the duration of the disease. In the enzymatic and reactive phases, conservative measures were preferred, whereas in the sequestration phase, surgery was the main method of treatment. These phases were characterized by certain morphological changes in the pancreatic parenchyma, however, the fact of the diagnosis of the phase was not confirmed by any instrumental method of research, which in most cases caused an imperial approach to the treatment of this pathology [4].However, the fact of the diagnostics phase was not confirmed by any instrumental method of investigation. It should be noted that the diagnosis of infected pancreanecrosis (IP), which, according to the existing standards of treatment of this pathology, is an absolute indication for surgical treatment. But in practice in some clinical situations it has shown its shortcomings in choosing the optimal treatment tactics. The presented data indicate the expediency of conducting studies devoted to more in-depth study of the processes occurring in pancreas and the development of treatment methods that reduce the number of early and late complications of pancreanecrosis.
2. Material and Methods
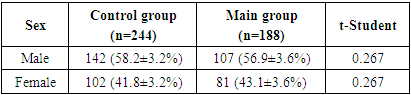
- The study is based on the analysis of examination and treatment results of 432 patients with various forms of pancreatic necrosis, who were divided into two groups: the control group (244 patients) and the main group (188 patients). Such a division was associated with tactical approaches to the treatment of this disease. Traditional treatment tactics was used in the control group, while improved therapeutic and diagnostic approaches were used in the main group.The sex ratio in both clinical groups was dominated by men, which was obviously due to the peculiarity of the causes of pancreatic necrosis (Tab. 1).
|
|
3. Results
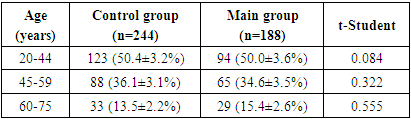
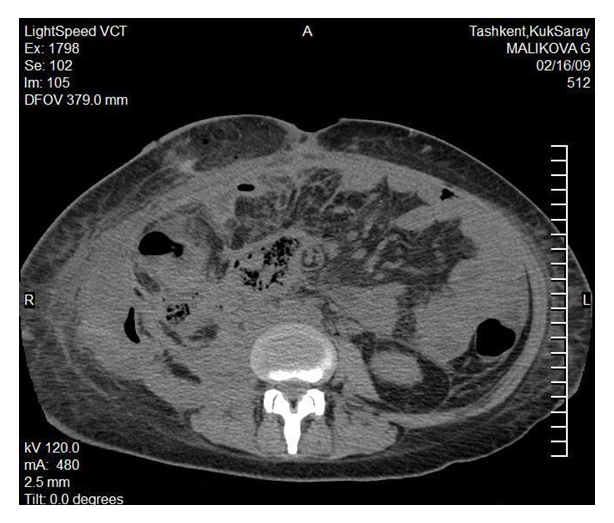
- Treatment results of sterile pancreanecrosis (SP) in the control group. Treatment was started with conservative therapy in all patients of the control group with SP (215 observations). Open surgical interventions were performed in 32 cases at the inefficiency of the therapeutic measures carried out. The treatment duration ranged from 2 days (at a fulminate course of the disease and a fatal outcome) to 14 days (at a favorable outcome against the background of conservative therapy) and 87 days (with a favorable outcome against the background of surgical treatment), averaging 32.1 ± 6.4 days. In the treatment of SP in 30.7% (66 patients) of observations, the development of complications of the underlying disease was noted; 32 patients (14.9%) underwent open surgery. In the postoperative period, the frequency of early surgical complications was 7.9% (17 cases), and it required surgical intervention in 1.9% (4 patients) of observations. In the long-term period, 27 (12.6%) patients had various complications, which required additional surgical interventions in 14 (6.5%) cases. There was a lethal outcome in 21 (9.8%) cases: 16 (7.4%) patients died from systemic complications of AP, 5 (2.3%) - from the development of surgical complications.Treatment results of infected pancreanecrosis (IP) in the control group. At IP all 29 patients were performed surgical interventions. The duration of inpatient treatment ranged from 3 days (at a fatal outcome) to 74 days (at a favorable outcome against the background of surgical treatment), averaging 40.9± 9.2 days. The frequency of early postoperative complications was 48.3%, late complications - 20.7%. The mortality rate made up 31.0% (9 cases). 6 (20.6%) patients died from systemic complications of AP, 3 (10.4%) – from the development of surgical complications.Summarizing the overall treatment results of patients with AP in the control group, it should be noted that 25.0% of patients were operated on, and the total mortality was 12.3%.We carried out a critical analysis of the causes of unsatisfactory treatment results, which allowed us to identify a number of points in the treatment of AP, which, in our opinion, require improvement:1. We faced the problem of treating SP. According to the existing treatment standards, the main method of cure for this form is conservative therapy. If conservative therapy is ineffective, surgical interventions should be performed only in the sequestration phase, which, according to Filin V.I., occurs 14 days after the disease. In our observations, 33 from 215 patients underwent surgical interventions. Only in 7 from them we revealed sequestered areas of the pancreas. In other cases, during the surgery an infiltrative process was detected in the pancreas and surrounding tissues, which not only minimized the effect of the intervention, but also contributed to the deterioration of the general condition as a result of surgical aggression. It made us conduct research to determine the optimal timing of the onset of the sequestration phase.2. In our opinion, IP requires improvement of therapeutic tactics. According to the existing principles of treatment, when verifying the infection of the inflammation focus in the pancreas, it is necessary to perform surgical interventions aimed at sanitizing the focus and removing necrotic tissues. Along with non-invasive research methods (ultrasound, MSCT), IP is diagnosed on the basis of fine-needle aspiration biopsy data. In 14 from 29 patients with IP, the diagnosis was determined on the basis of data from puncture studies. An infiltrative conglomerate was detected intraoperatively in 8 of them; no purulent foci were detected in the sequestration zone. Performing surgical intervention in similar situations only aggravated the general condition of patients. Despite the fact that in the existing standards, IP is an absolute indication for surgical intervention, the above clinical situations prompted us to think about the allocation of the morphological form of IP, when it is advisable to temporarily refrain from active tactics. This idea also required its own detailed study and a certain fragment of our scientific research was devoted to it.3. Attempts to solve the above two points of the research carried out contributed to the emergence of the question of the feasibility of improving the classification of AP. Given the lack of a unified classification, which reflects morphological changes in the pancreas at AP, the phases of the disease, the prevalence of the pathological process in retroperitoneal tissue, as well as the nature of the clinical course, we decided to systematize the AP classification.We conducted the following studies:I. We have conducted studies to determine the timing of the onset of the sequestration phase at AP. The results of 209 tomograms of patients of the control group in the treatment dynamics were studied. The analysis of the MSCT data showed that the sequestration process began in the period of more than 30 days and reached its maximum on the 40-50th day from the moment of the disease. Sequestration processes on tomograms are visualized as structureless alternating zones with low and high density of the "black dots" type, which are not increased at intravenous contrast. Morphological studies have confirmed the fact of late onset of sequestration processes at acute destructive pancreatitis. At SP in case of inefficiency of conservative therapy, surgical intervention is advisable to be performed in the sequestration phase, which, as our studies have shown, occurs in terms of more than 30 days (Fig. 1).
 | Figure 1. MSCT pattern of sequestration processes at pancreatic necrosis |
 | Figure 2. The process of infiltration in the pancreatic parenchyma |
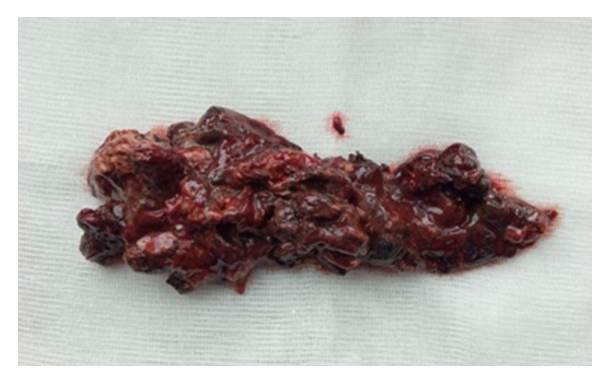 | Figure 3. Removed pancreatic sequesters |
4. Discussion
- In our observations, at the traditional treatment of pancreatic necrosis, in 25.0% of cases, patients were performed surgical treatment. The total mortality rate was 12.3%. The treatment results of patients with AP obtained by us are quite correlated with the data of Bagnenko S.F. (2014), Dyuzheva T.G. (2018), Weissman S. (2020), which indicate that the frequency of postoperative complications ranges from 14.7% to 29.5%, with a total mortality exceeding 15% [4-6]. It should be noted that the frequency of postoperative complications is associated with tactical approaches to the treatment of AP. These authors are supporters of active and expectant tactics, the main treatment principle of which was observed in our standards of treating patients with AP. Analysis of traditional treatment results of pancreatic necrosis revealed a number of shortcomings, one of which was the technical difficulty of surgical intervention in the early stages of the disease due to the pronounced infiltrative process. It should be noted that problems with the technical implementation of surgical interventions in the early stages of the disease were pointed out by Sitkin S.I. (2015), Bokarev M.I. (2013), Karimov Sh.I. (2005) [2,7-8]. It dictated the need to find ways to solve this problem.In a critical analysis of the clinical results obtained by us, it was indicated that there were no sequestration processes in infected pancreatic necrosis. A number of authors (Pushkarev V.P., 2015; Sabo A., 2015) faced this problem in their researches. They saw the solution to this problem in performing resection methods of operations, but this was possible only with limited lesion of the pancreas [9-10].Another problematic point is the shortcomings of existing classifications. In his publications Darwin V.V. (2014) pointed out the lack of the Atlanta-92 classification, arguing it by the fact that it does not reflect the clinical phases of the disease [11]. At the same time, Brekhov E.I. (2015) reported on the dependence of the nature of the therapy carried out depending on the phase of the disease [12]. Prudkov M.I. (2014) in his research pointed out the ways of the spread of the pathological process through the retroperitoneal tissue and recommended optimal surgical approaches to them [4]. However, all these studies are scattered. Our studies have significantly reduced the share of surgical treatment of pancreatic necrosis from 25.0% to 12.2% and mortality - from 12.3% to 6.9%.Analyzing the literature data and comparing them with the results obtained by us, we would like to note that Kulikov D.V. (2019), Shabunin A.V. (2015), Baron T.H. (2020), Koonce S.L. (2014) achieved approximate success in their research. In their studies they indicated the frequency of surgical interventions at SP from 11.5% to 31.3% and mortality from 5.8% to 13.4% [3,13-14]. The results obtained by us are quite correlated with the results of many researchers, and in some indicators they are even ahead of the results of our colleagues.
5. Conclusions
- Thus, we conducted studies that allowed us to expand our views on some fundamental issues related to the concept of pathological processes occurring in the pancreas at AP. The sequestration phase which was an indication for performing surgical intervention, required determining the timing and indisputable facts indicating the beginning of this process. It was reflected in the results of our research. A revolutionary discovery was the fact that IP was divided into infiltrative and sequestered forms, as well as proof of the need for conservative treatment in the absence of signs of sequestration, even if there was a fact of infection of the pathological focus. No less important is the fact of improving the AP classification, which allowed to assess the clinical situation in more detail and to increase the understanding of the clinical features of the disease course. In general, the conducted studies allowed to improve tactical approaches in the complex treatment of pancreatic necrosis, which ultimately contributed to improving the clinical results of such a heavy contingent of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML