-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(1): 6-11
doi:10.5923/j.ajmms.20221201.02
Received: Dec. 6, 2021; Accepted: Jan. 7, 2022; Published: Jan. 13, 2022

Serum Lipids, Lipid Ratio Pattern among Stroke Patients in a Nigerian Tertiary Care Hospital
Olufisayo Gabriel Ayoade1, Timothy Ekwere2, Franklin O. Dike3
1Department of Chemical Pathology, University of Uyo/ University of Uyo Teaching Hospital, Uyo, Akwa Ibom State, Nigeria
2Department of Haematology, University of Uyo/ University of Uyo Teaching Hospital, Uyo, Akwa Ibom State, Nigeria
3Department Internal Medicine, Neurology Unit, University of Uyo/ University of Uyo Teaching Hospital, Uyo, Akwa Ibom State, Nigeria
Correspondence to: Olufisayo Gabriel Ayoade, Department of Chemical Pathology, University of Uyo/ University of Uyo Teaching Hospital, Uyo, Akwa Ibom State, Nigeria.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: The impact of cerebrovascular accident (CVA) has been on the rise especially in developing countries. Abnormalities in lipids and lipoprotein ratios are an important factor in development of stroke despite the varied reports on evaluation of relationship between dyslipidemia and the risk of stroke. The aim of the study is to evaluate the pattern of dyslipidemia vis-à-vis serum lipoproteins and lipoprotein ratios among Stroke patients and to determine some of its correlates in patients attending tertiary hospital in South-South Nigeria. Methods: This is a prospective case-control study. A total of 61 participants consisting of 41 stroke patients (cases) and 20 healthy persons (controls) were consecutively recruited into the study in Neurology unit of University of Uyo Teaching Hospital (UUTH) over a period of 6 months. Fasting lipids, total cholesterol (TC), triglycerides, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) were estimated. Results: The TC, LDL-C, HDL-C and Non-HDL-C levels were significantly higher in stroke cases than in controls. Among stroke cases, elevated LDL-C was the most frequent abnormality in absolute lipid values, found in 78.0% of stroke cases. This was significantly higher (p=0.001) than the percentage amongst the controls (30.0%). Among stroke cases and controls, abnormalities in lipid ratios were significantly higher among stroke cases than in controls (p<0.001). Conclusion: The most common dyslipidemia among stroke patients is elevated LDL-C which is an atherogenic lipoprotein implicated in atherosclerosis. The pattern of dyslipidemia among the stroke patient also includes raised TC and low HDL levels with elevated LDL-C/HDL-C ratio.
Keywords: Stroke, Lipoprotein ratios, Lipids, Cardiovascular disease
Cite this paper: Olufisayo Gabriel Ayoade, Timothy Ekwere, Franklin O. Dike, Serum Lipids, Lipid Ratio Pattern among Stroke Patients in a Nigerian Tertiary Care Hospital, American Journal of Medicine and Medical Sciences, Vol. 12 No. 1, 2022, pp. 6-11. doi: 10.5923/j.ajmms.20221201.02.
Article Outline
1. Introduction
- Stroke (Cerebrovascular accident) is defined as a rapidly developed global or focal neurological deficit lasting more than 24 hours or leading to death with no apparent cause other than vascular origin [1]. It is recognized to be one of the major causes of mortality and long-term severe disability with significant socio-economic burden especially in post-stroke care worldwide [2]. There has been an in increase in the global burden of Cerebrovascular accident (CVA), as the impact is worse in many developing countries. World Health Organization (WHO) has projected that 80% of stroke cases will occur in these countries by year 2030 [3]. Sub-Sahara Africa seems to bear the largest burden of stroke as the prevalence and case fatality is higher due to marked cases of hypertension and other risk factors like dyslipidemia among the general population [4-5].In Nigeria, even though there has been lack of community-based data on the prevalence, hospital-based studies show that stroke accounts for 0.9 to 4.0% of patient’s hospitalization, up to 45% of neurological admissions. It also accounts for 3.7% of emergency medical admission and it is the eighth leading cause of death [6-7]. CVA can be classified as ischemic or hemorrhagic with the former being predominant (88%) and the latter accounts for 12% which can either be subarachnoid (9%) or intracerebral (3%) [8]. The modifiable risk factors which commonly predispose to stroke include Dyslipidemia, Hypertension, Cardiac diseases especially atrial fibrillation and diabetes mellitus (DM) amongst others. Effective primary prevention of stroke by early identification of risk factors is key as over 80% of the global stroke burden is attributed to few factors that improve significantly with interventions [9].Dyslipidemia is an important factor in the development of stroke playing an essential role in the initiation and progression of atherosclerosis. [10]. Studies evaluating the relationship between lipid biomarkers and the risk of stroke have reported varied associations. [11-12] The discrepancies reported is very much base on the studied population differences and in varying methods utilized in the process [12].Plasma lipids and lipoproteins levels have consistently been associated with cardiovascular diseases including myocardial infarction and stroke. Despite ample evidence suggesting that increased levels of total cholesterol (TC) and low levels of high-density lipoprotein cholesterol (HDLc) are strong and important risk factors for coronary heart disease, many observational studies have yielded inconsistent results for lipid profile and stroke. [12-13] The predictive role of serum lipid level in the occurrence of stroke still remains unclear despite several empirical evidences that support the use of lipid lowering agent such as statins as a means of reducing cardiovascular disease risk [14].Traditional lipid parameters, represented by increased concentrations of total cholesterol (TC), triglycerides (TGs), low-density lipoprotein cholesterol (LDL-C), and decreased high-density lipoprotein cholesterol (HDL-C), have been identified as risk factors and predictors of cardiovascular disease, including stroke [15]. The assessment of lipid ratios such as TC/HDL-C, TG/HDL-C, and LDL-C/HDL-C is recognized as a better predictor of vascular risk compared to traditional lipid parameters [15,16].This study sought to examine the plasma lipoproteins and lipoprotein ratios in patient with stroke and its association with other risk factors. Stroke, not only has it been on increase in many developing nations but it is the leading cause of morbidity and mortality in the world. There has been mixed and inconsistent reports on the plasma lipid levels in stroke patients as it affects other risk factors especially in Nigeria. The obvious inadequate knowledge necessitates more research in this area. This study has the potential to provide valuable information on the predictive role of lipids in occurrence of stroke.
2. Materials and Methods
- Study Design: This was a prospective case-control study designed to achieve the set objectives of the study. Study Population: Adult Patients diagnosed with stroke in line with the WHO clinical definition of stroke and confirmed by computer tomography scan (CT-scan) of the brain were recruited consecutively into the study over a 6 months period (March-August 2019). Age and sex matched healthy individuals were used as controls for the study. A total of 61 participants consisting of 41 stroke patients (cases) and 20 healthy persons (controls) were consecutively recruited into the study.Sample Collection/ Analytical Procedure: After informed consent were taken, 5 mls of blood was drawn from each participant after an overnight fast of 8-10 hours. It was collected in plain tube, allowed to clot and separated through centrifugation (1500× g for 30 minutes). It was then stored at -20°C until assay was run. The assays were run in 3 batches, the duration storage of each batch of samples is between 6-8 weeks. Biochemical Analysis The lipid profile (Total Cholesterol, Triglycerides, High density Lipoprotein-Cholesterol) was assayed using the enzymatic method, cholesterol oxidase phenol 4-aminoantipyrine peroxidase (CHOD-PAP) on Automated Chemistry Analyzer (Selectra ProM, ELITech Group. Holland). LDL was calculated using the Friedewald formula. Inclusion Criteria: Newly diagnosed adult patients with stroke in line with WHO definition and confirmed by CT-scan of the brain and who gave oral and signed informed consent were recruited into the study during the study period (March –August 2019). Exclusion Criteria: Patients less than 18 years of age, patients whose diagnosis were not confirmed by CT- scan and those who did not give informed consent were excluded from the study. Data Collection: Data was collected in a profoma designed for the study. This include; age, sex, blood pressure, plasma fibrinogen level, co-morbid risk factors including hypertension, diabetes mellitus, obesity and chronic cigarette smoking.Data Analysis: Data was analysed using SPSS for windows version 20. The results were presented in simple tables. Descriptive and inferential statistics such as t-test were used as appropriate. The level of significance was set at p< 0.05. Ethical Consideration: Ethical approval was obtained from the Health Research Ethics Committee of the Hospital before the commencement of this study. Also, all participants in this study signed a written informed consent before being recruited in the study.
3. Results
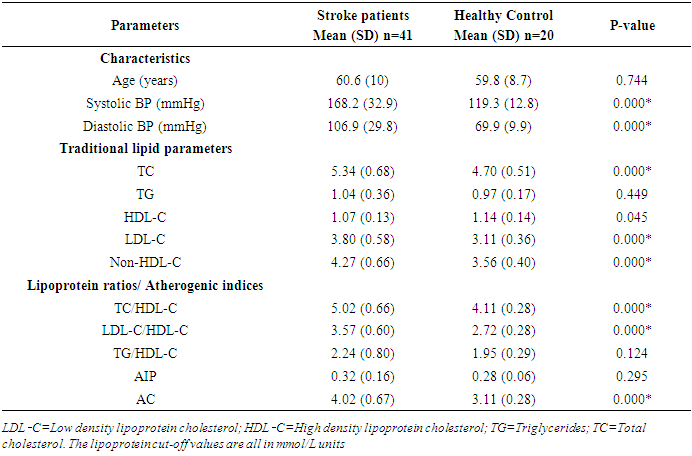
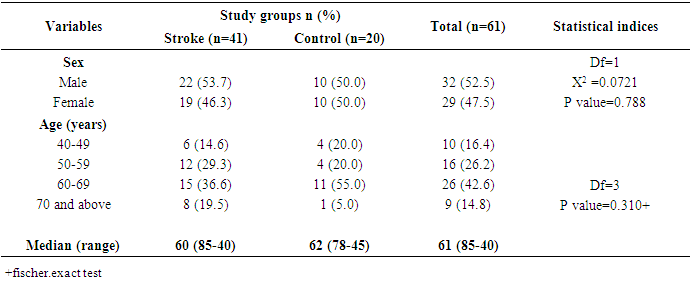
- A total of Forty-one (41) stroke patients and twenty (20) age and sex matched controls were recruited for this study within the study duration. The male to female ratio in both arm of the study was 1:1. The mean age range of both the subjects and controls were 60.6 years and 59.8 years respectively with no statistical difference between the 2 groups. (Table 1) The mean systolic and diastolic blood pressure between the subjects and controls were 168.2±32.9 / 119.2±12.8 and 106.9± 29.8 / 94.7± 94.7 respectively. (p = 0.0001 both cases).
|
|
|
4. Discussion
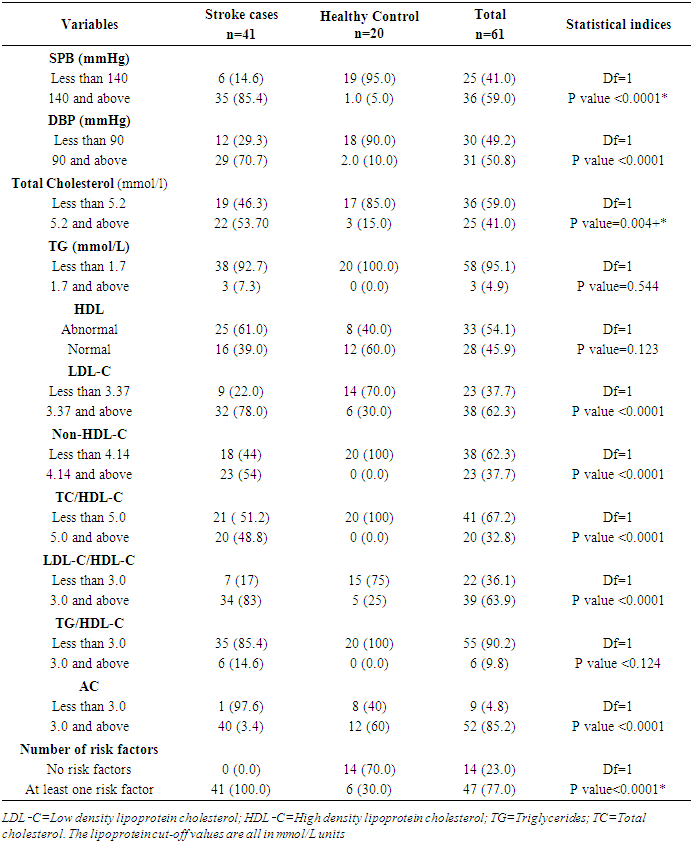
- Several observational studies have shown conflicting findings regarding the association of dyslipidemia with cerebrovascular accident and there is lack of sufficient data on the prevalence and pattern of dyslipidemias among stroke patients in Nigeria. [17-18] This study was designed to determine the pattern of dyslipidemia among stroke patients and its association with risk factors of stroke. Our results showed a high prevalence of dyslipidemia with higher TC, LDL-C and non-HDL-C values, i.e., more than the respective cut-off values, with about 78% of the patients fulfilling at least 1 criterion for dyslipidemia according to the NCEP ATP III guideline for the detection, evaluation, and management of dyslipidemia [19]. This is consistent with reported rates of dyslipidemia among stroke patients in Spain, which has ranged between 60-80% [20].The male to female ratio was almost similar to other studies in South-western Nigeria [17,21]. higher incidence of stroke among male may be attributed to high prevalence of smoking among men and the consumption of more fatty food. In addition, the hormonal effects of estrogen also have a protective effect against stroke in females. Although a study from Oxford shire, showed that males are more affected than females by genetic factors, the family history are more likely to be found in females than in males [22].Regarding the age distribution of stroke patients in the study, the mean age was 60.6 years (±10.7) which is similar to a result of a study by Olamoyegun etal, that showed a mean age of 69 years [20]. The majority, 23 (56.5%) patients, were above the age of 60 years. Again, this result is almost similar to the previous study conducted in Ibadan, south west Nigeria that found 58% of patients were above the age of 60 years [23]. These results indicate that the incidence of stroke is higher for those who are above 60 years old.The most common dyslipidemia pattern in our study is hypercholesterolemia and reduced HDL-C. The lipid profile of stroke patients was studied and it was found that there were 22 (53.7%) patients with total cholesterol level≥5.2 mmol/L and the mean total cholesterol was 5.34 mmol/L (±0.68), while elevated LDL-C occurs in 78% of stroke patients compared to 30% in healthy controls. This finding is in agreement with similar studies around the world that has demonstrated hypercholesterolemia among stroke patients and as there has been significant correlation between cholesterol level and the risk of stroke [24,25].This study also recorded low HDL-C among stroke patients statistically significant compared to the healthy controls. This is similar to findings from Olamoyegun etal [17]. Several studies showed similar findings and suggested that lower levels of HDL are associated with increased risk of stroke, while high levels of HDL are considered as a slight protective indicator against stroke [25,26]. On the other hand, a study conducted in Hawaii, showed no clear relationship between low levels of HDL and the risk of having stroke [27].We found out that there is no statistical difference in TG in stroke patients and healthy controls. TG level was normal in 92.7% of stroke patient with mean of 1.04±0.36. These results are similar to several studies that showed the TG level ranging from 1.12 to 1.54 mmol/l among stroke patients [28-29]. This indicate that the relationship between elevated TG levels and the risk of stroke is still lacking, and this is in agreement with previous studies showed that no clear relationship between elevated TG levels and risk of stroke [29-31].Lipid ratios have been demonstrated by several published studies to be better predictors of vascular risk than traditional lipid parameters. More than 80% of the stroke cases in our study has abnormal LDL-C/HDL-C ratio with mean of 3.57±0.60, statistically higher than in healthy controls with mean of 2.72±0.28. In their study of some stroke patients in northern Nigeria, Glew and his colleagues observed that despite normal lipid values both control and stroke patients, the LDL/HDL ratio distinguished the stroke patients from the control, and has shown to have more predictive power in assessing dyslipidemia in stroke patients [32].The main limitation of our study was the fact that it was hospital-based study, making it difficult to generalize our findings to reflect the whole country. Also, it was a cross-sectional study, and thus cannot be used to predict some of the causal relationships indicated. More prospective studies with larger sample sizes are therefore suggested.
5. Conclusions
- The prevalence of dyslipidemia in our study population is high and increases with age. The most common dyslipidemia among stroke patients is elevated LDL-C which is an atherogenic lipoprotein implicated in atherosclerosis. The pattern of dyslipidemia among the stroke patient also includes raised TC and low HDL levels with elevated LDL-C/HDL-C ratio. Determination of lipoprotein ratios should complement the other investigations in evaluation of patient with Stroke.
ACKNOWLEDGEMENTS
- We are thankful to the resident doctors of department of Chemical Pathology, Haematology and Neurology unit, Internal Medicine for their assistance.
Statement of Ethics
- The authors had the approval from the University of Uyo Teaching Hospital Institution Health Research Ethical Committee.
Disclosure Statement
- The authors have no conflicts of interest to disclose.
Funding Sources
- The authors did not receive funding from any source.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML