-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(12): 907-909
doi:10.5923/j.ajmms.20211112.12
Received: Dec. 1, 2021; Accepted: Dec. 13, 2021; Published: Dec. 24, 2021

Pregnancy Disease - Patomorphology of Preeclampsia
Eshbaev Erkin1, Isroilov Rajabboy1, Allaberganov Dilshod1, Qurbonov Abduburkhan2, Boboev Khamza1, Kholieva Nigora1
1Department of Pathological Anatomy, Tashkent Medical Academy, Tashkent, Uzbekistan
2Department of Histology and Medical Biology, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Eshbaev Erkin, Department of Pathological Anatomy, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this scientific article, pregnancy-related disease - pathomorphological changes in the liver specific to preeclampsia were studied. As material, the livers of 18 women who died of preeclampsia in the last 10 years were studied at the macroscopic and microscopic levels. The main role in the pathogenesis of preeclampsia is diffuse vascular spasm and hypertension. Vasospasm leads to hypoxia, decreased anticoagulants, hypercoagulability, and disseminated intravascular coagulation syndrome (DICS). As a result, the microcirculation in the liver is disrupted, the permeability of the microtubule wall is increased, the outflow of blood fluid and plasma proteins into the tissue, leading to the development of dystrophic and necrobiotic changes in tumor and parenchymal cells. The results of morphological examination show that under the influence of preeclampsia in the liver is initially detected circulatory, ie dilatation and fullness of all blood vessels, a large number of background fluids. Another characteristic pathomorphological feature of preeclampsia was the central necrosis of the liver fragments. In the periportal area of the liver, specific capillary infarction foci and accumulation of fibrin protein in the sinusoidal peripheral cavity were detected.
Keywords: Pregnancy, Preeclampsia, Liver, Morphology, Histology
Cite this paper: Eshbaev Erkin, Isroilov Rajabboy, Allaberganov Dilshod, Qurbonov Abduburkhan, Boboev Khamza, Kholieva Nigora, Pregnancy Disease - Patomorphology of Preeclampsia, American Journal of Medicine and Medical Sciences, Vol. 11 No. 12, 2021, pp. 907-909. doi: 10.5923/j.ajmms.20211112.12.
1. Introduction
- Preeclampsia is a disease that develops in the third trimester of pregnancy, as a complication of pregnancy, with tissue tumors, proteinuria, arterial hypertension, and persistent dysfunction of vital organs. There are mild, moderate, and severe degrees of preeclampsia [1,2,3]. In moderate and severe forms, of course, the morphofunctional status of the liver is impaired, resulting in a sharp rise in liver enzymes, decreased platelet count, impaired blood clotting system, impaired blood circulation in liver tissue, hemorrhage, acute dystrophic and necrotic changes in the liver parenchyma [4].The main role in the pathogenesis of preeclampsia is diffuse vascular spasm and hypertension. Vascular spasm occurs as a result of damage to the endothelium, which is confirmed by an increase in the amount of fibronectin in the blood and glycoprotein from subendothelial tissue. As a result of vascular spasm, endothelin is released into the blood, which activates renin-angiotensin and increases the release of aldesterone and adrenaline into the blood [5,6]. Vasospasm leads to hypoxia, decreased anticoagulants, hypercoagulability, and DICS. As a result, the microcirculation in the internal organs, often in the liver, is disrupted, the permeability of the microvascular wall is increased, blood fluid and plasma proteins are released into the tissue, leading to the development of dystrophic and necrobiotic changes in tumor and parenchymal cells.
2. Materials and Methods
- During the last 10 years, 2011-2020, the Republican Center for Pathological Anatomy of the Ministry of Health of the Republic of Uzbekistan conducted autopsy examinations of 18 women who died of moderate and severe preeclampsia, macroscopic and microscopic examination. Liver pieces were solidified in 10% neutralized formalin for 48 h and washed in running water. It was dehydrated in increasing concentrations of alcohol, paraffin with wax was added, and bricks were prepared. Histological sections were stained by hematoxylin-eosin, van-Gizon, and Periodic Acid - Schiff (PAS)-reaction methods. The drugs were examined under a light microscope and images were taken from the desired areas.
3. Results and Discussion
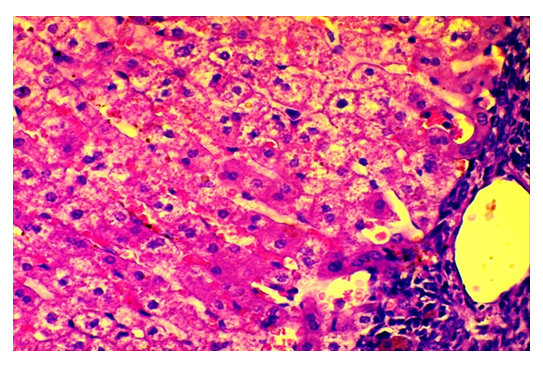
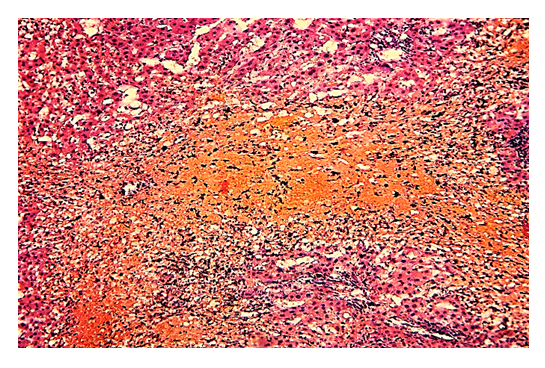
- Microscopic examination of liver tissue in preeclampsia showed that the strongest pathomorphological changes occurred in the blood vessels, i.e., the central vein and sinusoids dilated paralyzedly, the histostructure was disrupted, and numerous small focal hemorrhages occurred in the liver parenchyma. Hemorrhagic foci are observed to appear around the disse cavity, at the site of necrosis, and between hepatocytes (Fig. 1). Macrophages and lymphoid cells are found in and around the foci of hemorrhage. Hepatocytes are found to be disordered in most areas, disrupting their columnar location. It is observed that the tissue of the portal tract is enlarged due to strong swelling and inflammatory infiltrate, the connective tissue fibers in it are homogenized by fibrinoid swelling.
 | Figure 1. 29 age, died of severe preeclampsia. All the blood vessels in the liver dilated, and numerous foci of hemorrhage appeared. Paint: G-E. Zoom: 10x10 |
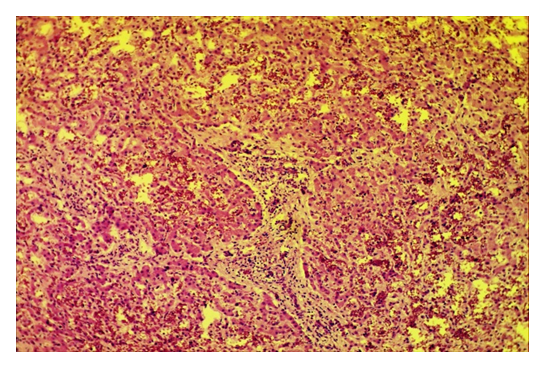
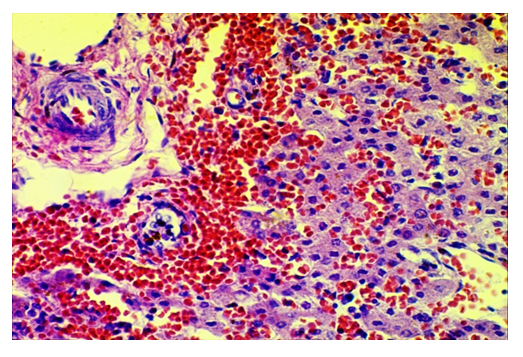 | Figure 2. 29 age, died of severe preeclampsia. Massive periportal area, diapedesis blood transfusion into the disse cavity, lymphoid cells appeared in the interstitial tissue. Paint: G-E. Zoom: 10x40 |
 | Figure 3. 32 age, who died of severe preeclampsia. Massive necrosis foci appeared in the centrolobular areas of the liver parenchyma. Paint: G-E. Zoom: 10x10 |
4. Conclusions
- We studied those who died during pregnancy, childbirth, and the postpartum period by autopsy as maternal mortality as a result of clinical-morphological analysis into 3 groups according to the origin of the disease. 1-group. Liver diseases developed in connection with pregnancy. 2-group. Liver disease associated with pregnancy. 3-group. Pregnancy developed against the background of chronic diseases of the liver.Pregnancy-related liver diseases include: preeclampsia, pregnancy cholestasis, acute fatty liver disease. The main role in the pathogenesis of preeclampsia is diffuse vascular spasm and hypertension. Vasospasm leads to hypoxia, decreased anticoagulants, hypercoagulability, and DICS. As a result, the microcirculation in the internal organs, often in the liver, is disrupted, the permeability of the microvascular wall is increased, blood fluid and plasma proteins are released into the tissue, leading to the development of dystrophic and necrobiotic changes in tumor and parenchymal cells. The results of morphological examination show that under the influence of preeclampsia in the liver is initially detected circulatory, ie dilatation and fullness of all blood vessels, a large number of background fluids. Another characteristic pathomorphological feature of preeclampsia was the central necrosis of the liver fragments. In the periportal area of the liver, specific capillary infarction foci and accumulation of fibrin protein in the sinusoidal peripheral cavity were detected.According to the literature, pathomorphological changes characteristic of preeclampsia, the appearance of infarcts in the periportal area of the liver fragments, necrosis in the center of the fragment, hemorrhage in the entire area. In our material, these changes were not always and not observed in all cases. The occurrence of infarction was detected in 62.6%, centralobular necrosis - in 86.4%, bleeding in almost all cases.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML