-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(12): 882-886
doi:10.5923/j.ajmms.20211112.08
Received: Nov. 22, 2021; Accepted: Dec. 6, 2021; Published: Dec. 15, 2021

Technical Aspects of Laparoscopic Prosthetic Hernioplasty
Sayinaev Farrukh Karomatovich1, Kurbaniyazov Zafar Babajanovich1, Rakhmanov Kosim Erdanovich1, Davlatov Salim Sulaymonovich2
1Samarkand State Medical Institute, Republic of Uzbekistan, Samarkand
2Bukhara State Medical Institute, Republic of Uzbekistan, Bukhara
Correspondence to: Davlatov Salim Sulaymonovich, Bukhara State Medical Institute, Republic of Uzbekistan, Bukhara.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The problem of treating patients with ventral hernias currently remains not fully understood and is very relevant. The aim of the study is to improve the quality of treatment of ventral hernias by improving the tactical and technical aspects and optimizing endovideosurgery in hernioplasty. The article presents the data of a clinical examination of 117 patients with ventral hernias who were operated on in the surgical department of the 1st clinic of the Samarkand State Medical Institute for the period from 2016 to 2020. Depending on the choice of treatment tactics, the patients were divided into two groups. The first group, the comparison group, consisted of 65 (55.5%) patients who underwent open hernia repair. The second group, the main group, consisted of 52 (44.5%) patients who were initially planned for laparoscopic prosthetic hernioplasty. The use of the proposed modified Undo Close needle made it possible to technically optimize the stage of fixing the prosthesis to the anterior abdominal wall by simplifying the stitching of tissues in a direction parallel to the horizontal plane in intracorporeal conditions.
Keywords: Ventral hernia, Alloplasty, Pneumoperitoneum, Endovideosurgery
Cite this paper: Sayinaev Farrukh Karomatovich, Kurbaniyazov Zafar Babajanovich, Rakhmanov Kosim Erdanovich, Davlatov Salim Sulaymonovich, Technical Aspects of Laparoscopic Prosthetic Hernioplasty, American Journal of Medicine and Medical Sciences, Vol. 11 No. 12, 2021, pp. 882-886. doi: 10.5923/j.ajmms.20211112.08.
Article Outline
1. Relevance
- The problem of treating patients with ventral hernias currently remains not fully understood and is very relevant. Despite a significant number of works devoted to the surgical treatment of ventral hernias, the solution of the problem of preventing recurrence of the disease in the treatment of patients with hernias of the anterior abdominal wall remains very relevant [3,7,14].The literature indicates that the trend in the treatment of ventral hernias and the prevention of recurrence are based on the restoration of the strength of the anterior abdominal wall, physical rehabilitation in the postoperative period and the implementation of the cosmetic effect [1,4,5,9,11,13]. Given this, the choice of the method of surgery until now is an urgent problem. The modern concept dictates the need to close the hernial defect by combined methods using mesh implants, which ensures the restoration of the function of the anterior abdominal wall [2,6,8,10,12].
2. The Aim of the Study
- To improve the quality of treatment of ventral hernias by improving the tactical and technical aspects and optimizing endovideosurgery in hernioplasty.
3. Materials and Methods of Research
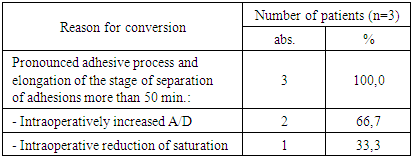
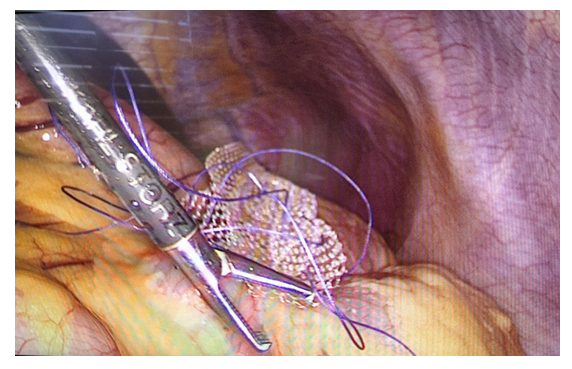
- The study is based on a clinical examination of 117 patients with ventral hernias who were operated in the surgical department of the 1st clinic of the Samarkand State Medical Institute for the period from 2016 to 2020. All patients were operated on as planned. Depending on the choice of treatment tactics, the patients were divided into two groups. The first group, the comparison group, consisted of 65 (55.5%) patients who underwent herniation by the open method. The second group, the main group, consisted of 52 (44.5%) patients who were scheduled for laparoscopic prosthetic hernioplasty.In the main group, 49 (94.2%) laparoscopic prosthetic hernioplasty was performed. Of these, 37 (75.5%) patients (subgroup 1) used standard mesh polypropylene implants, and 12 (24.5%) patients (subgroup 2) used composite mesh implants "Physiomesh" or "Prosid" (Ethicon).In the main group of patients, several stages of standard endovideosurgical hernioplasty were improved: the sites of working trocars were standardized; the dimensions of the implant along the perimeter were 5 cm larger than the size of the hernial defect; the implant was fixed to the anterior abdominal wall using an Endo Close needle modified by us.Surgical intervention was performed according to the standard procedure.Stage I - introduction of the first trocar. Depending on the primary or postoperative hernia, the introduction of the first trocar was carried out in two ways:1. Patients with primary ventral hernia used the standard method with the introduction of a Veresh needle (Fig. 1), the pneumoperitoneum was inflated to a pressure of 12-14 mm Hg, after removing the needle, a trocar was injected into the abdominal cavity. Usually, entry into the free abdominal cavity was carried out using a special optical trocar "Visiport™" (Covidien), then the abdominal cavity was audited;2. With the probability of adhesions, patients with postoperative ventral hernias used the Hassen technique, i.e. the abdominal wall was opened in layers with a 2-4 cm long incision, the adhesions were separated around the wound under visual control and a trocar with an obturator was inserted through the incision, the wound was sealed.
 | Figure 1. Insertion of the Veresh needle and the imposition of a pneumoperitoneum |
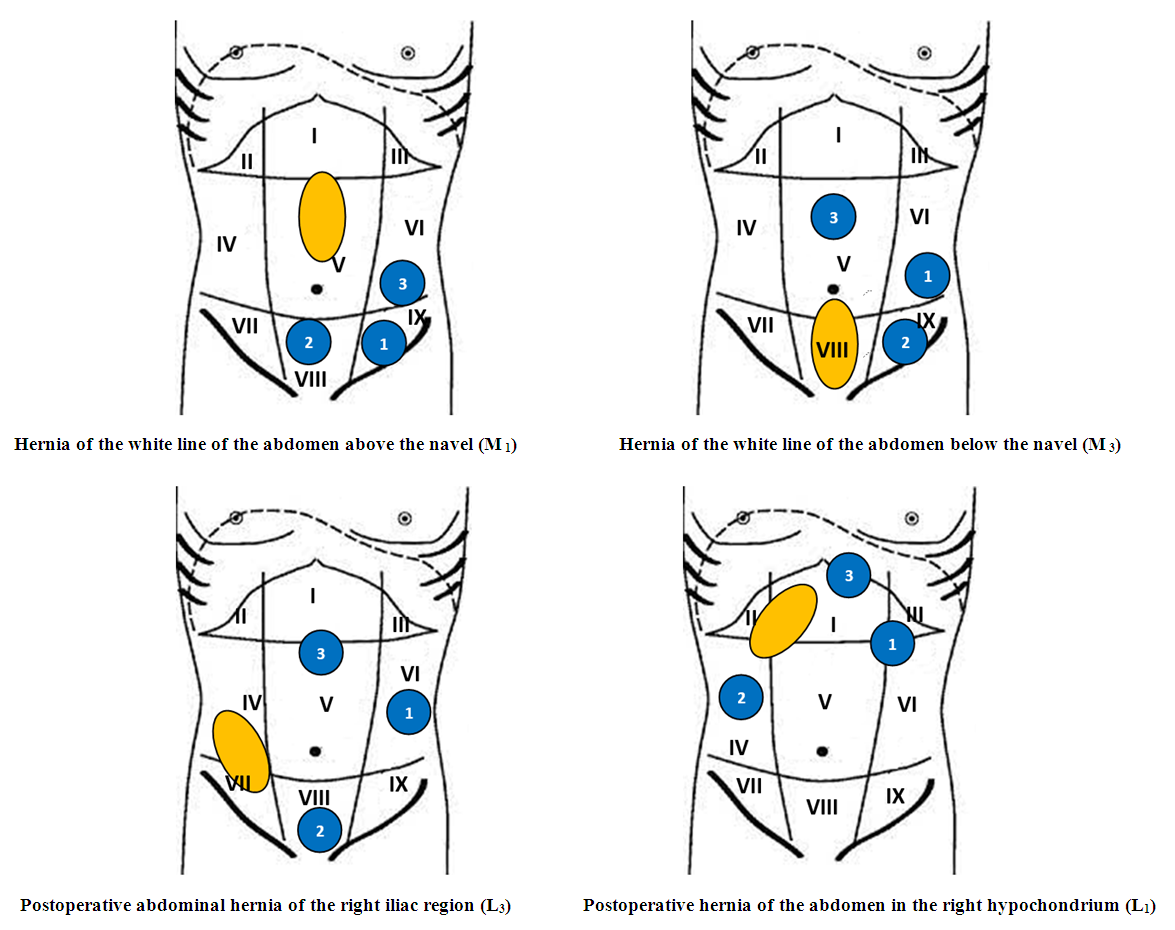 | Figure 2. Scheme of trocar insertion points in the most typical localization of ventral hernias |
 | Figure 3. A type of mesh polypropylene implant whose perimeter dimensions are 5 cm larger than the size of the hernial defect |
 | Figure 4. Unfolding into a rolled-up mesh implant |
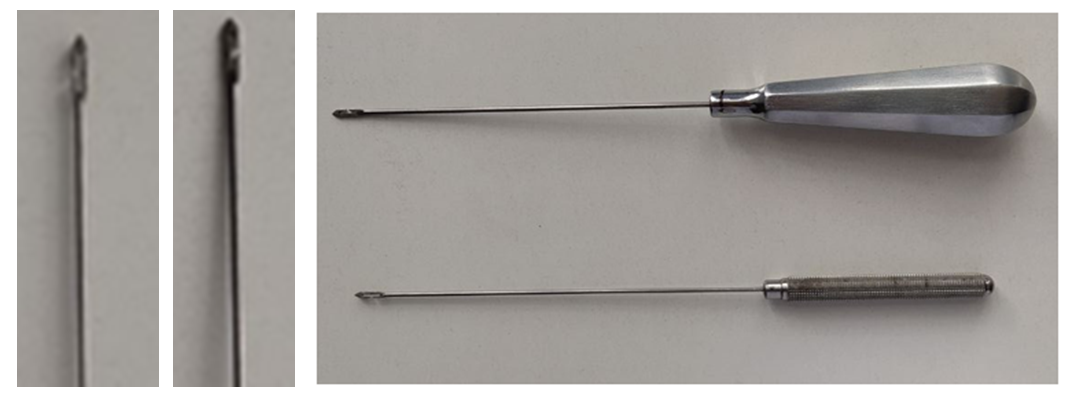 | Figure 5. Modified Endo Close needle for suturing the implant to the anterior abdominal wall |
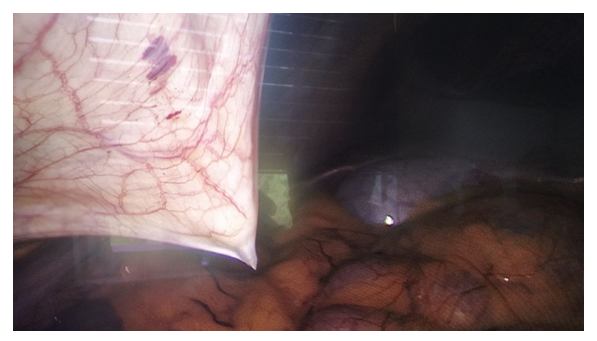 | Figure 6. Puncture of the needle from the abdominal cavity visually under the control of endovideolaparoscopy |
 | Figure 7. View of the suture threads removed from the side of the abdominal wall |
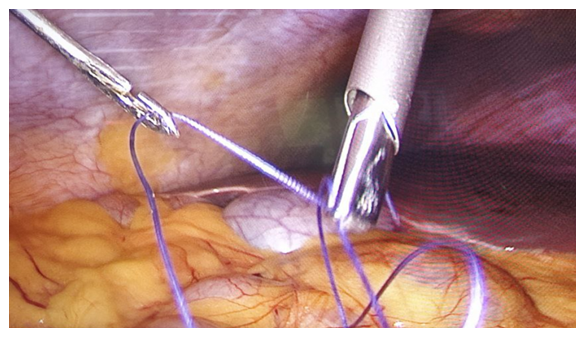 | Figure 8. Peritonization of a standard mesh implant using a modified Endo Close needle |
4. The Results of the Study
- Improving the choice of tactics for surgical treatment of ventral hernias, techniques for performing laparoscopic prosthetic hernioplasty and other innovations developed and implemented within the framework of this study could not but affect the immediate results of management of this category of patients.In the early years, i.e. during the development of laparoscopic technology for performing prosthetics hernioplasty took quite a long time (to 71.6 ± 0.7 min), however, with increasing experience of surgeons and the development of technology, the surgery significantly decreased to 51.4 ± 0.6 min (T-criterion = 6,74, P<0.001) (Fig. 9).
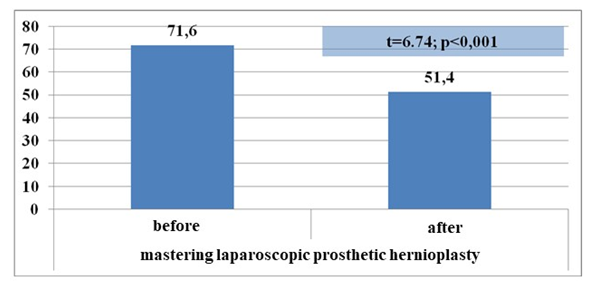 | Figure 9. The time of the operation during the development of endovideosurgical surgery (min.) |
|
5. Conclusions
- The use of the proposed modified Undo Close needle made it possible to technically optimize the stage of fixing the prosthesis to the anterior abdominal wall by simplifying the stitching of tissues in a direction parallel to the horizontal plane in intracorporeal conditions.The improvement of technical aspects allowed: due to the differentiated introduction of the first trocar, such complications as perforation of the wall of the hollow organ were eliminated; due to the standardization of the maintenance of working trocars, the technique of the operation was simplified; due to the fixation of the implant with an offset from the hernial gate by 5-6 cm, the recurrence of hernia in the long-term postoperative period was minimized; due to the use of a modified needle, it was possible to eliminate technical difficulties in fixing the prosthesis and in peritonizing standard non-composite mesh implants with a reduction in this stage of the operation from 27.4 ± 0.5 to 12.6 ± 0.7 minutes (P <0.001).Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML