-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(12): 861-865
doi:10.5923/j.ajmms.20211112.04
Received: Nov. 6, 2021; Accepted: Dec. 3, 2021; Published: Dec. 15, 2021

Characteristics of the Genotypical Applicability of Patients with an Peptic Ulcer and Features of Pharmacotherapy
Klichova F. K., Musaeva D. M.
Bukhara State Medical Institute Named after Abu Ali Ibn Sino, Bukhara, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article examines the influence of the CYP2C19 gene genotype on the effectiveness of pharmacotherapy with proton pump inhibitors in a patient with peptic ulcer disease.
Keywords: Genotype, CYP2C19 gene, Proton pump inhibitors, Peptic ulcer disease, Pharmacotherapy
Cite this paper: Klichova F. K., Musaeva D. M., Characteristics of the Genotypical Applicability of Patients with an Peptic Ulcer and Features of Pharmacotherapy, American Journal of Medicine and Medical Sciences, Vol. 11 No. 12, 2021, pp. 861-865. doi: 10.5923/j.ajmms.20211112.04.
Article Outline
1. Introduction
- Peptic ulcer disease (PUD) is a chronic recurrent disease that occurs with alternating periods of exacerbation and remission, the leading manifestation of which is the formation of a defect (ulcer) in the wall of the stomach and duodenum [1,2].Analysis of statistical data for the Republic of Uzbekistan showed that 56.6% of patients with gastrointestinal tract disease accounted for the adult population, 34.5% for children under the age of 14, 8.9% of all patients with gastrointestinal tract disease.Today, according to WHO data, 10-15% of the population of developed countries suffers from peptic ulcer disease [3,4].Several risk factors for PUD have been identified, including the use of non-steroidal anti-inflammatory drugs (NSAIDs), Helicobacter pylori (H. pylori) infection, alcohol abuse, smoking, and physical stress [5].Currently, peptic ulcer disease is considered a multifactorial disease that does not have a specific etiological factor as the main cause of pathology. At the same time, most scientists dealing with peptic ulcer disease agree with that, the acid-peptic factor occupies a central place in ulcerogenesis of this disease [6]. Over the past 25-35 years, there has been a steady development and formation of a new paradigm of ulcerogenesis that peptic ulcer disease is a local infectious process, where the causative agent is H. pylori, which firstly identified in 1983 by Australian scientists B. Marshall and J. Warren. However, if in the first years of the study of H. pylori it was claimed that the infection rate of patients with gastroduodenal ulcers was more than 90%, then later this index decreased to 80%, and then to 50 or less values [7].A number of scientific studies are being carried out in the world in order to achieve high efficiency in the pharmacotherapy of this disease. In recent years, most of attention has been paid to pharmacogenetic parameters that ensure the effectiveness of treatment.Despite the successes achieved, the situation regarding the control of this disease remains difficult. In this regard, there is an urgent need to recognize this problem as an extremely important and priority and to create an appropriate state national program, the implementation of which would allow determining the health of the nation for many years to come [8,9].Currently, Uzbekistan is implementing a number of measures to prevent and eliminate various diseases, taking into account the genetic parameters of patients. The action strategy for the five priority areas of development of the Republic of Uzbekistan in 2017-2021 defines such aims as "... the introduction of a set of measures to improve and strengthen public health, reduce morbidity, prevent genetic diseases and increase life expectancy..." [10]. Solving these tasks contributes to the prevention and diagnosis of various diseases, increasing the degree of medical care, improving the use of modern technologies to identify genetic indicators of patients, reducing the degree of morbidity.Actuality of research. Peptic ulcer (PUD) and duodenal ulcer (DU) have been and continue to be one of the urgent problems of modern medicine. The relevance of the current state of this problem is due to its widespread prevalence among the population of the whole world. In addition, the prospects for the further development of UD, due to the continued increase in the frequency and prevalence of this disease, its severe and often progressive course, complications leading to premature disability and death of patients, which necessitates the improvement of treatment methods [11,12].There are certain difficulties in choosing the optimal drugs for the treatment of PUD. They are based on a large representation of dosage forms and individual drugs offered for the treatment of PUD on the market. At the same time, issues related to the use of specific pharmacotherapeutic regimens require special attention. It should be noted that the need to optimize the use of medicines in the field of healthcare and strict individualization of the treatment of the disease in each individual patient is currently being actively discussed.The pathogenesis of ulcer is traditionally described as an imbalance between the factors of “aggression "and the factors of" protection "of the mucous membrane of the stomach and duodenum, which occurs against the background of chronic Helicobacter pylori gastritis [13]. H. pylori clearly requires eradication if the patient has chronic gastritis, ulcer or duodenal ulcer, MALToma, or if he has had a gastric resection for treatment cancer. In addition, H. pylori eradication may be recommended to reduce the risk of gastric cancer.Treating H. pylori infection is not an easy task because there are no regimens that guarantee 100% effectiveness. Scientists are showing increased interest in this topic. In the mid-1990s. the effectiveness of therapy reached 90%. Today, in many regions of the world, this figure rarely exceeds 60%.In accordance with the Maastricht Agreement, the criterion for the effectiveness of eradication schemes is considered to be a degree of eradication of at least 80%. If initially standard triple eradication therapy met the requirements, then over time (less than five years) its effectiveness decreased to 65–75%. Insufficient effectiveness of standard eradication regimens and the lack of studies devoted to increasing the effectiveness of pharmacotherapy of ulcer, taking into account the patient's genetic characteristics, served as the basis for this study. Therefore, it seems relevant to determine genetic markers for predicting the effectiveness and safety of the therapy [14]. All schemes of combined eradication therapy in accordance with the Maastricht IV consensus, along with antibiotics, include as first-line drugs - proton pump inhibitors (PPIs).Recently, there has been an increase in the frequency of the absence of H. pilory eradication against the background of the use of combined eradication therapy up to 30%, which is associated not only with an increase in resistance to antibacterial drugs, but also with the role of the CYP2C19 genetic polymorphism in the effectiveness of PPIs [15,16]. The metabolism of drugs of the PPI group is carried out mainly by the enzyme CYP2C19 of the cytochrome P450 superfamily [17]. The CYP2C19 gene is a member of the IIC subfamily of the cytochrome P-450 genes, which is involved in the metabolism of a number of drugs: proton pump inhibitors (omeprazole, pantorazole, lansoprazole, rabeprazole, and esomeprazole), antidepressants (tricyclic antidepressants - amitripramine seizure of serotonin - citalopram, MAO inhibitor - moclobemide), antiepileptic drugs (diazepam, phenytoin, phenobarbital, clonazepam), non-steroidal anti-inflammatory drugs (diclofenac, indomethacin), anticoagulants (warfarin, thiotropyridine drugs including) antiplatelet drugs (including) antiplatelet agents (antiplatelet drugs) voriconazole), b-blockers (propranolol), antineoplastic (cyclophosphamide), some hormones (eg progesterone) and other drugs [18].The CYP2C19 genetic polymorphism determines three major metabolizer phenotypes (drug users): extensive, slow, and fast. Extensive metabolizers are individuals with a normal PPI metabolic rate. As a rule, they are homozygous for the "wild" allele of the corresponding enzyme gene.Slow metabolizers (sometimes zero), as a rule, homozygotes (with an autosomal recessive type of inheritance) or heterozygotes (with an autosomal dominant type of inheritance) for the polymorphic "slow" allele of the corresponding enzyme gene, are characterized by a reduced PPI metabolic rate In such individuals, enzyme synthesis an inactive ("defective") enzyme is absent or synthesized, as a result of which the drug accumulates in high concentrations, which leads to the appearance of undesirable side reactions. Hence, it is clear that for slow metabolizers, the dose of the drug must be lower or another drug is prescribed. Fast (or overactive) metabolizers, as a rule, are homozygotes (with an autosomal dominant mode of inheritance) for the polymorphic “fast” allele of the corresponding enzyme gene, and are characterized by an increased PPI metabolic rate. The rapid metabolism of the drug does not allow at standard doses to reach its therapeutic concentration in the blood; therefore, the dose of the drug for fast metabolizers should be higher than for normal metabolizers [19].The implementation of genetic research has now ceased to be an object of purely fundamental science. Understanding the genetic factors underlying the individual response to a drug gives clinicians hope for the possibility of personalizing therapy, minimizing the risk of side effects and achieving high efficacy of the pharmacotherapy used. The principles of PUD pharmacotherapy can be standard, but the treatment of the disease cannot be the same for all patients, it must be personalized. This approach is based on the genetic characteristics of the patient [20].The main factor underlying genetic differences between people is multiple allelism due to polymorphic markers [21]. Therefore, the individualization of pharmacotherapy, which pharmacogenetics deals with, comes down, first of all, to the identification of polymorphic markers associated with changes in the body's response to drugs, the development of methods for genotyping patients (identification of allelic variants of polymorphic markers) and the introduction of this methodology into practical medicine.The lack of clear criteria for the choice of rational pharmacotherapy, allowing to provide a sufficiently individual approach to the treatment of ulcer, determines the relevance and the need for further research in this direction.Therefore, the study of individual genetic differences, leading to differences in the body's response to one or another drug from the PPI group in modern therapy of ulcer, is of paramount importance for optimizing the pharmacotherapy of the disease, which was the reason for this study.
2. Materials and Research Methods
- A comprehensive examination of 120 patients with peptic ulcer disease who were hospitalized and monitored at the Bukhara regional hospital was carried out. The control group consisted of 50 healthy people with no history of pathology from the digestive tract, living in the Bukhara region, corresponding in gender and age to the examined group of patients with peptic ulcer disease.The age of patients with peptic ulcer disease ranged from 18 to 75 years. The initial stage of our work was the selection and optimization of the operation of the oligoprimer system for the detection of the rs4244285 polymorphism of the CYP2 C 19 gene by the polymorphic marker G681A. The nucleotide sequences of the detection of polymorphism rs4244285 gene CYP2 With 19 were selected using the program «Oligo v.6.31» (Molecular Biology Insights Inc., USA) and synthesized in LLC "Syntol" and NPF "Liteh" (Moscow).The rest of the components were purchased from the world's leading manufacturers - “Serva” (Germany), “Sigma” (USA),”Helikon” NPF Litekh, “Sibenzim” (Russia), etc.Adaptation of primer systems for standard PCR analysis was carried out using PCR analyzers “Applied Biosystems 2720” (USA) and Rotor-Gene 6000 (Corbett Australia). For amplification, a 25 μL reaction mixture was used, which contained 2.5 μL of 1 OxTaq buffer (67 mMtris-HCl (pH 8.8), 16.6 mM (NH4) 2SO4>, 2.5 mM MgCl2, 0.01% Tween-20), 0.1 μg of genomic DNA, dNTP mixture (dATP, dGTP, dCTP, dTTP at 200 μM each), 1 unit. Termusaquaticus DNA polymerase (manufactured by “Sileks”, Moscow) and 5-10 pM locus-specific oligonucleotide primers. Temperature-time parameters were changed depending on the pairs of oligoprimers.For the detection of rs4244285 of the CYP2 C 19 gene, preliminary denaturation is 940C (1 min. 1 cycle), 35 amplification cycles: 930C (10 sec) - denaturation, 640C (10 sec) - primer annealing, 720C (20 sec) - elongation, and final synthesis 720C (1 min. 1-cycle), 10 min storage.Polymorphic regions of the CYP2 C 19 gene were identified using the PCR-SSP method. The specificity and the number of amplified fragments were checked by agarose gel electrophoresis.The results were statistically processed.
3. Results and Discussion
- Individual variability of drug response is one of the main problems in modern clinical practice. Genetic variability of genes encoding these enzymes, the patient's genotype play an important role in the manifestation of individual sensitivity to drugs.It is known that one of the variants of the studied CYP2C19 * 2 gene (rs 4244285) consists in the substitution of guanine (G) for adenine (A) in position 681 (681 G- A) in exon 5. Using a modified detection method, we studied polymorphism G 681 A gene C UR2S19 which has options genotype A / A, GG, G / A. In the study group, the genotype of patients with the CYP2 C 19 gene with PUD, living in the Bukhara region, was determined. It should be noted that, in the structure of the studied group of patients with PUD, it was revealed that carriers of the "wild type" allele CYP2C19 GG accounted for more than 67% (Fig. 1), carriers of the heterozygous CYP2C19 G / A allele accounted for 30%, carriers of the homozygous CYP2C19 A allele. / A accounted for 2.5%. Thus, the frequency of occurrence of allele G corresponded to 82%, while the frequency of occurrence of allele A was about 17% of patients with PUD.
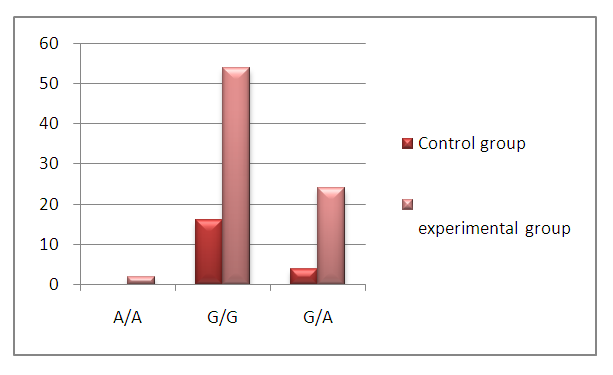 | Figure 1. Frequency of distribution of genotypes of the C UR2C19 gene in patients with ulcer |
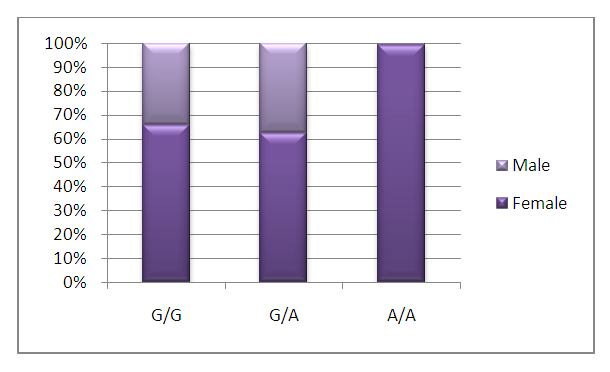 | Figure 2. Gender division of genotypes of the CYP2C19 gene |
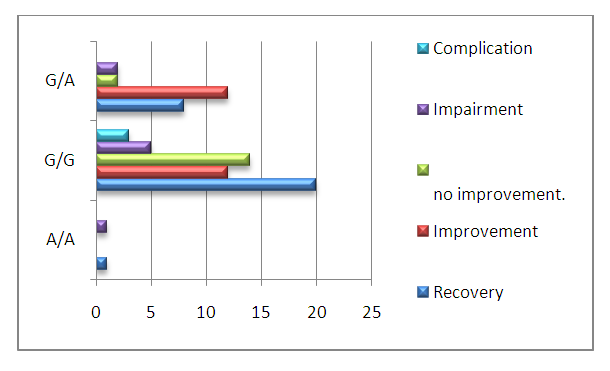 | Figure 3. Results of PUD treatment and their relationship with the frequency of distribution of CYP2C19 gene genotypes in PUD |
4. Conclusions
- Thus, statistical studies show that up to 60% of the variability in response to pharmacotherapy is due to genetic variation between individuals. The genetic affiliation of the organism has a huge impact on the effectiveness and safety of the applied pharmacotherapy.The GG genotype for the polymorphic marker G 681 A of the CYP2C19 gene is found in the greatest number among patients with PUD living in the Bukhara region and corresponds to the extensive type of PPI metabolism. It should be especially noted that this genotype is found 2 times more in women of this region. The use of genetic information in clinical medicine will allow the development of drug protocols and surveillance methods to reduce the risk of adverse reactions and maximize the effectiveness of treatment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML