-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(12): 856-860
doi:10.5923/j.ajmms.20211112.03
Received: Oct. 24, 2021; Accepted: Nov. 22, 2021; Published: Dec. 15, 2021

Differentiated Approach to the Treatment of Patients with Acute Deep Vein Thrombosis of the Lower Limb
Irnazarov A. A., Rakhmanov S. U., Khasanov V. R., Matmuradov J. K.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to the study of a differentiated approach in the treatment of patients with acute deep vein thrombosis of the lower limb. The treatment analysis of 50 patients with the use of endovascular interventions was carried out. Depending on the location of thrombosis, the authors suggest an individual approach in determining access to perform minimally invasive interventions. After thrombaspiration and thrombolysis in days 1-3, the onset of complete vein recanalization, balloon angioplasty and stenting, followed by the use of oral anticoagulants, the condition of the veins, its patency, the preservation of valve function was assessed by dynamic control using ultrasound duplex scanning on the 20th day, 3 months, 6 months, 12 months after the intervention. According to the results of the study, early admission to the hospital, endovascular interventions reduce the time of the onset of complete vein recanalization, the duration of interventions and favors early activation of patients without the development of post-thrombophlebitic disease.
Keywords: Acute venous thrombosis, Deep vein thrombosis, Pulmonary thromboembolism, Venous thromboembolic complications, Thrombolysis, Thrombaspiration, Post-thrombotic disease
Cite this paper: Irnazarov A. A., Rakhmanov S. U., Khasanov V. R., Matmuradov J. K., Differentiated Approach to the Treatment of Patients with Acute Deep Vein Thrombosis of the Lower Limb, American Journal of Medicine and Medical Sciences, Vol. 11 No. 12, 2021, pp. 856-860. doi: 10.5923/j.ajmms.20211112.03.
1. Introduction
- Deep vein thrombosis (DVT) of the lower limbs and pulmonary embolism (PE) have common pathogenetic roots. They are the most common circulatory disorders and are one of the main health issues [1-3]. According to epidemiological studies, the incidence of deep vein thrombosis of the lower limbs in the general population is approximately 160 per 100,000 annually with a fatal pulmonary embolism rate of 60 per 100,000 of population [2,4-5]. Deep vein thrombosis (DVT) of the lower limbs and pulmonary embolism (PE) can be combined into the term "venous thromboembolic complications" (VTEC). Numerous publications are devoted to the important social significance of this issue, confirming the widespread prevalence of deep vein thrombosis of the lower extremities and its consequences, as well as the associated mortality, disability and economic costs spent on the treatment of such type of patients [6]. However, the true incidence of DVT remains unknown, since it is asymptomatic in the vast majority of cases [7-8]. The reliability of classical clinical symptoms depends on the nature and extent of thrombotic lesions. It is observed with common ilio-femoral thrombosis in most cases. Postthrombophlebitic syndrome is the most common late complication of DVT and is developed in 20-50% of patients with DVT of the lower limbs. In 7-10% of cases, the disease has a severe form, with the formation of trophic ulcers [9-10]. According to the results of an 8-year study by P. Prandoni et al., in 355 patients who underwent an episode of deep vein thrombosis, the overall incidence of PTD after 2 years from the moment of thrombosis made up 22.8%, after 5 years - 28% and after 8 years - 29.1% [11]. Leading experts from different countries are constantly developing and updating recommendations for practicing physicians helping them to adopt the optimal individual approach to treating such type of patients, in which evidence-based medicine data that are relevant at the time of their creation are analyzed and summarized [3]. However, there is a lack of unconditional implementation of new diagnostic algorithms in practice, recommended by experts, as well as medical and surgical approaches for effective therapy and prevention of VTEC [6].Thus, the above data indicate the need for an integrated approach in the treatment of patients with acute deep vein thrombosis, taking into account the level of thrombosis, the choice of optimal approaches for endovascular interventions, thrombaspiration and thrombolysis, prevention of complications in the early and late postoperative periods.The aim of the research was to study the safety and efficiency of catheter-aspiration thrombectomy and thrombolysis, their preventive role in the development of post-thrombotic disease.
2. Material and Methods
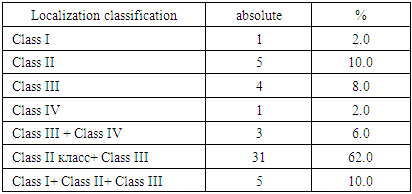
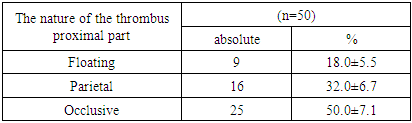
- We analyzed the results of endovascular intervention in 50 patients with DVT of the lower limbs who were inpatient treatment at the 2nd clinic of the Tashkent Medical Academy in the period from 08/01/2016 to 11/01/2019. There were 35 females and 15 males aged 20 to 70 years. Patients came 3-8 days from the onset of the disease with complaints of edema and soreness of the lower limb. Endovascular intervention was performed on days 1-3 after admission. The difference in the circumference of the lower extremities was on average: in the middle third of the leg + 3 ± 5 cm; in the middle third of the thigh + 5 ± 7 cm. The diagnostic stage began with ultrasound duplex scanning (USDS). The level of thrombosis and the nature of the thrombus were determined during USDS. The level of D-dimer in the blood was determined to clarify thrombogenicity; in controversial cases multisprial computed phlebography was performed. Before endovascular intervention, patients were prescribed antiplatelet and anticoagulant therapy. The operation was performed in an X-ray operating room using an Artiz Zee Celing apparatus from Siemens (Germany). Localization of thrombosis in all patients was determined in accordance with the LET classification (Lower Extremity thrombosis) (Tab. 1).
|
|
3. Results
- Vein thrombosis of the left lower extremity was detected in 47 (94%) of 50 patients, and in the right lower limb in 3 (6%) cases. 35 (70%) of them were females and the rest 15 (30%) were males. 27 (54%) of 50 patients with DVT of low extremities went to the clinic up to 3 days, 15 (30%) - up to 7 days, 5 (10%) - up to 10 days, 3 (6%) - up to 14 days after the onset of the disease. All patients were performed endovascular treatment. The approaches were carried out depending on the thrombosis class; with their help puncture and installation of an introducer were performed followed by mechanical thromboaspiration and installation of a cavafilter. Then thrombolysis was performed.8 (16%) from 50 (48%) patients had LET class III-IV thrombosis. The intervention was carried out through CVF. The thromboaspiration time in those patients lasted 20 minutes, the fibrinolytic dose was 1.2-1.4 million IU and the thrombolysis time reached 6-7 hours. The results of recanalization of the vein lumen depending on the duration of thrombosis were 95-100% in all patients.The level of LET class II-III thrombosis was detected in 31 (62%) patients. The intervention was performed through popliteal access. The thromboaspiration time in those patients lasted 35 minutes, the fibrinolytic dose was 2.5 million IU, and the thrombolysis time was 10 hours. The results of recanalization depended on the duration of the thrombosis. In 21 (42%) patients recanalization reached 95-100%, in 8 (16%) cases - 50-95%, in 2 (4%) patients this indicator made up 50% recanalization.In 11 (22%) patients the level of thrombosis was characterized by a combination of LET class I-II-III. In 6 of them, the level of thrombosis was up to the mouth of the PTV, the intervention was performed through the PTV access. The result of recanalization depends on the duration of thrombosis, while in 4 (8%) cases recanalization was 95-100%, in 4 (8%) patients it made up 50-95% and in 3 (6%) cases - 50%. Only 5 (10%) patients were performed two approaches: the first through PTV at the level of the lower third of the leg, the second one was carried out through CFV in order to reduce the duration of manipulation, the dose of fibrinolytic agent and the time of thrombolysis. In these patients, the thrombo-aspiration time amounted 35-50 minutes, the fibrinolytic dose made up 2.5-2.8 million IU, and the thrombolysis time reached 12-14 hours.May-Thurner syndrome was diagnosed in 31 (62.0%) patients, angioplasty and iliac vein stenting were performed in 25 (50%) of these. In 6 (12.0%) cases, for economic reasons, only iliac vein angioplasty was performed. Indicators of preservation of the degree of recanalization, depending on the timing of observation are presented in Table 3.
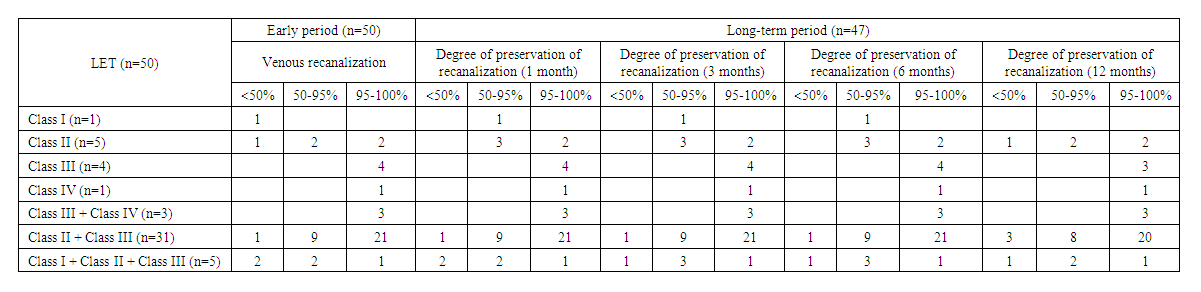 | Table 3. Indicators of retention of recanalization degree depending on the time of observation (LET classification) |
4. Discussion
- Recently, in most foreign clinics, early "destruction" of a blood clot by catheter-aspiration thrombectomy or thrombolysis has become the standard of treatment for proximal DVT. Modern endovascular technologies have shown very encouraging results: the rapid removal of the thrombus has significantly reduced the incidence of post-thrombophlebitic disease (PTD) and PE [2,3]. At the same time, some guidelines contain a low level of recommendation (2B) for the use of catheter-aspiration thrombectomy or thrombolysis, which only indicates the lack of a sufficient number of randomized controlled trials evaluating its efficiency [7]. However, the prevalence of PTD during treatment or ophmoral DVT with anticoagulants alone is significantly higher and reaches 50–82% [7].As a thrombolytic agent for performing catheter-aspiration thrombectomy or thrombolysis, various drugs were used for proximal DVT - urokinase, alteplase, streptokinase [8]. If it is necessary to transfer from a parenteral anticoagulant to a dose of rivaroxaban, apixaban or dabigatran, it must be taken when the infusion of unfractionated heparin (UFH) is stopped or within 2 hours before the planned subcutaneous administration of the next dose of anticoagulant (low molecular weight heparin or fondaparinux sodium). Observational data show that recent advances in approaches to the treatment of DVT and PE are not immediately reflected in treatment results due to some inertia of implementation into the practice. For example, in practice, there may be non-adherence to recommended drug regimens, as evidenced by the data from the RIETE register. 1441 (8.4%) from 17194 patients included in the registry from 2013 to 2016 took rivaroxaban as initial therapy and 81 patients (0.47%) took apixaban. Among 16123 patients receiving long-term anticoagulant therapy, rivaroxaban was taken by 2,403 (15%) patients and apixaban by 315 (2%) patients. The results of the analysis showed that 81.7% of patients took the recommended daily dose of the drug, and only 78% of patients followed a double therapy regimen. Patients with active cancer or with renal insufficiency took reduced doses of rivaroxaban. It is significant that in patients who took rivaroxaban at the recommended doses or outside the recommended regimen of frequency, a statistically significant higher frequency of VTEC relapses was observed. At the same time, in patients who took drugs in doses lower than recommended, there was no decrease in the frequency of bleeding [13]. Estimation of life quality together with objective research methods (clinical, laboratory, instrumental) makes it possible to obtain comprehensive information about the effect of the drug on the patient's condition and is an integral element in the examination of new drugs and their comparison with existing analogues. Since ACT is the main method of treating patients with DVT, the consideration of life quality with the use of tableted direct-acting anticoagulants (rivaroxaban, dabigatran etexilate) and heparins, followed by the administration of warfarin in real clinical practice, is a relevant and undisclosed issue [6].
5. Conclusions
- The use of catheter-aspiration thrombectomy and thrombolysis in the acute period of DWT of low limb is effective for the prevention of PE, preservation of valvular function of veins and prevention of post-thrombophlebic syndrome (PTFS). The principles of endovascular treatment of patients with acute deep vein thrombosis of the lower limbs depending on the location of the lesion were detailed.The new method of endovascular thromboaspiration and thrombolysis in acute deep vein thrombosis of the lower extremities developed by us will reduce the incidence of complications and shorten the duration of surgery in this category of patients. The developed measures to reduce complications such as bleeding, retrombosis will improve the life quality of patients in the immediate and late postoperative periods. The use of rvaraxaban according to the standard dosage made it possible to improve the postoperative state of patients with various types of bleeding. The use of catheter-aspiration thrombectomy and thrombolysis was accompanied by early activation and improvement of life quality in patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML