Gulbakhor Ilkhomjonovna Mamadalieva 1, Nodira Khakimovna Ruzieva 2
1Obstetrician Gynecologist in Private Clinics "New Medical Service" and "IHLOS Med», Independent Applicant in Doctoral Studies at TashPMI, Tashkent, Uzbekistan
2Associate Professor of the Department of Obstetrics and Gynecology, Pediatric Gynecology at the Tashkent Pediatric Medical Institute, Doctor of Medical Sciences, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Benign cervical diseases (BMD) are morphofunctional pathologies of the cervical mucosa (CM) in which the normoplasia of the epithelium is preserved. Cervical dysplasia includes cervical cylindrical epithelia ectopy, cervical erosion, ectropion, cervical leukoplakia and dysplasia, and cervical intraepithelial neoplasia with low and high grade squamous intraepithelial lesions (CIN I and II). BMD accounts for 25-45% in the structure of gynecological diseases. Screening studies of BMD as a potential risk factor for precancerous cervical and cervical cancer are extremely necessary in terms of health of each individual woman and the female population as a whole, and therefore the composition of the population and the birth rate in it. We examined 120 women who were on outpatient treatment of DZSHM from 2020 to 2021, the age of women in the main group was from 25 to 44 years, the average age was 36.1 ± 1.42 years, in the CG (n = 20) the age of women ranged from 25 to 43 years, the average age was 35.8 ± 1.37 years. In both groups, we carried out a comprehensive examination of women, which included: study of complaints and anamnesis, examination in mirrors, bacterioscopic examination of material from the cervical canal and vagina, high-quality PCR for urogenital infections (Chlamydia trachomatis, Mycoplasma genitalium, Neisseria gonorrhoeae, Trichomonas vaginalis, HPV types 16 and 18), traditional cytological method, extended colposcopy, and biopsy for histological verification of the diagnosis. Smoking, irregular sex life, unprotected contacts and frequent change of partners, a large number of births and abortions, as well as the HPV-positive status of patients are risk factors for the occurrence and development of intraepithelial neoplasia of CM.
Keywords:
Cervical intraepithelial neoplasia, Risk factors
Cite this paper: Gulbakhor Ilkhomjonovna Mamadalieva , Nodira Khakimovna Ruzieva , Influence of Risk Factors for Development of Cervical Intraepitelial Neoplasia, American Journal of Medicine and Medical Sciences, Vol. 11 No. 12, 2021, pp. 851-855. doi: 10.5923/j.ajmms.20211112.02.
1. Introduction
Pathological processes of the cervix (CM) occupy a sufficient volume of practical activities of a gynecologist and play a significant role in the state of public health. CM pathologies are very common, especially at the age of 30-49 years and are characterized by a tendency to increase in frequency, occupy an important place in the structure of diseases of the reproductive system, they are diagnosed in every fifth woman of the reproductive and almost every tenth woman in menopause [8]. DZShM of all visits to a gynecologist make up from 35% to 80% [4].Cervical cancer is in 3rd place in terms of frequency of occurrence among tumors of the reproductive system and in 6th place among all tumors. Early diagnosis and treatment of CM diseases, given the prevalence of cervical cancer and the state of women's reproductive health, is especially important and necessary [9].The prevalence of cervical cancer in Russia in 2018 was 124 patients per 100,000 women, while 41.8% of all cases of this disease were actively diagnosed during preventive examinations [1]. In 2018, cervical cancer was diagnosed in late stages in 32.6% of new cases [1]. The prevalence of cervical cancer differs in populations and is 0.4-7.7% depending on the type [6,10,11,12]. According to Rakhmanova Zh.A. the incidence rate of cervical cancer in our country averages 7.6 per 100,000 women. The lowest rate was recorded in 2011 - 5.4 per 100,000, and the highest was recorded in 2009 and 2018 at about 8.5 per 100,000 women. The youngest woman with established cervical cancer was 21.7 years old, and the oldest was 85.2 years old, which only confirms the need for timely diagnosis of cervical cancer and reducing the influence of risk factors for CM pathology on the body of women of all ages, and especially the target group 30-50 years old [3].Many authors associate the emergence of CIN with marital status and female tobacco smoking [5,8,11]. Cervical intraepithelial neoplasia (CIN) is "a change in the epithelium of the cervix, consisting in a violation of the stratification of the middle and basal layer, without changes in the surface layer and stroma, but with a violation of layering" [7].According to the WHO classification [5], there are three degrees of CIN:1. CIN I (mild degree, I degree) - these are “minor disorders of differentiation of the epithelium with moderate proliferation of cells of the basal layer. Changes cover no more than 1/3 of the thickness of the epithelial layer, starting from the basement membrane” [5].2. CIN II (moderate, grade II) “is characterized by more pronounced changes. In this case, the lesion occupies 1/2 of the thickness of the epithelial layer, starting from the basement membrane ” [5]. 3. CIN III (severe dysplasia, III degree). "Characterized by lesions of more than 2/3 of the epithelial layer." [5].Cervical intraepithelial neoplasias of CM (Cervical Intraepithelial Neoplasia, CIN), provided early diagnosis, can be cured before cervical cancer occurs by organ-preserving methods. So, any cervical cancer is not timely diagnosed intraepithelial neoplasia of cervical cancer and lost time for its treatment and prevention of invasive cancer [2,5].These facts involuntarily suggest that the attitude of the female population to such a formidable pathology as cervical cancer is not serious which is most likely explained by the lack of knowledge of women about this pathology and the lack of active educational work at the level of primary health care, the media and the state as a whole.Purpose of the study: on the basis of the results of clinical-anamnestic and laboratory studies, to assess the influence of risk factors on the degree of squamous intraepithelial lesion of the cervix.
2. Materials and Methods
To achieve the goal of the study, we examined 120 women who were on outpatient treatment of DZSHM from 2020 to 2021, the age of women in the main group was from 25 to 44 years, the average age was 36.1 ± 1.42 years, in the CG (n = 20) the age of women ranged from 25 to 43 years, the average age was 35.8 ± 1.37 years.In both groups, we carried out a comprehensive examination of women, which included: study of complaints and anamnesis, examination in mirrors, bacterioscopic examination of material from the cervical canal and vagina, high-quality PCR for urogenital infections (Chlamydia trachomatis, Mycoplasma genitalium, Neisseria gonorrhoeae, Trichomonas vaginalis, HPV types 16 and 18), traditional cytological method, extended colposcopy, and biopsy for histological verification of the diagnosis. The identification of risk factors and the calculation of the strength of their influence was carried out after the diagnosis of CIN I or CIN II.
3. Results and Discusion
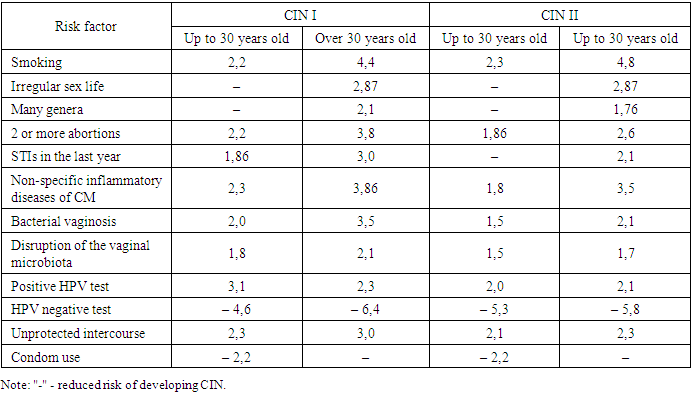
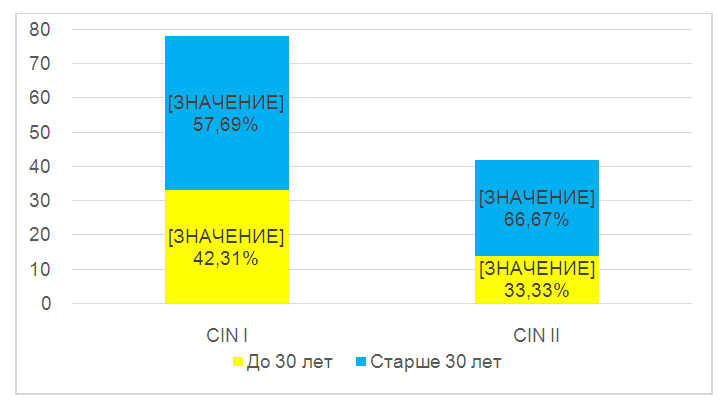
The main group at this stage of the study was divided by us into groups I and II, group I - 78 (65%) patients with confirmed CIN I, aged from 25 to 43 years, average age - 35.3 ± 1.35 years, in II the group included 42 (35%) patients with confirmed CIN II, aged from 27 to 44 years, mean age - 37.2 ± 1.42 years.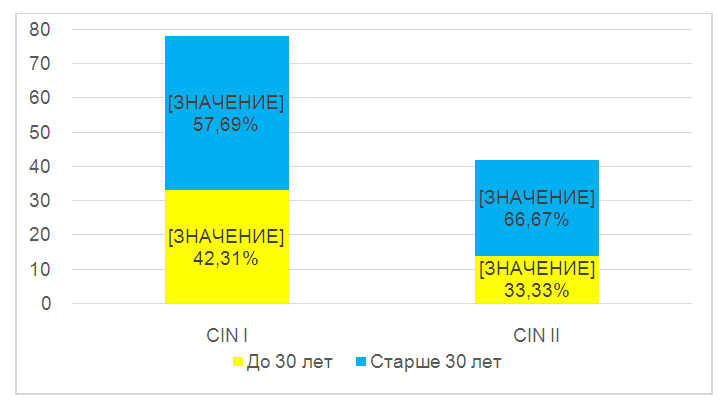 | Figure 1. The ratio of patients of both age groups in the studied subgroups |
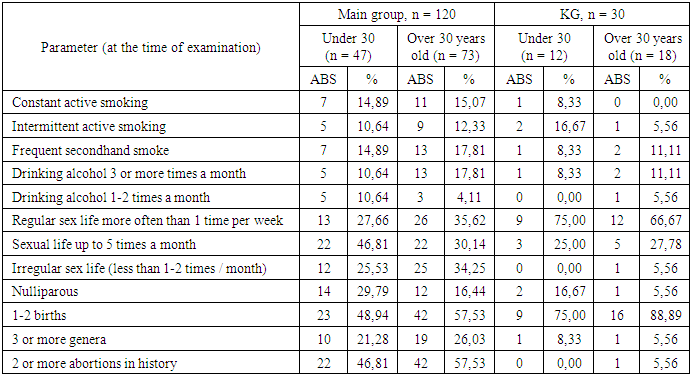
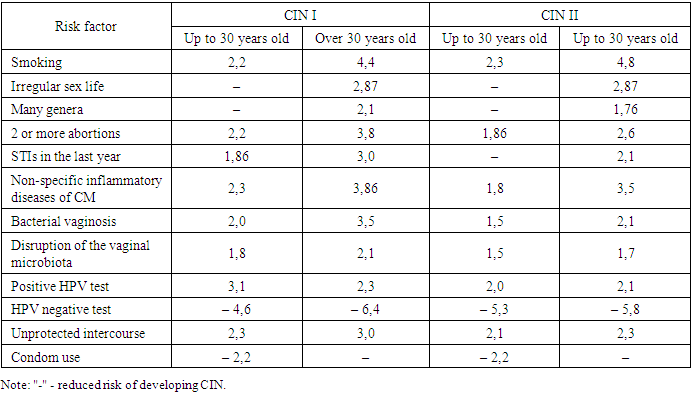
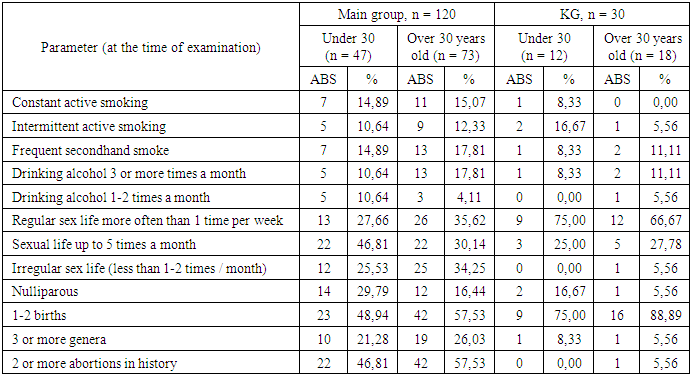
Patients who smoke (smoking ≥ 3 years, smoking ≥ 10 cigarettes per day) in our study statistically significantly more in the main groups (p <0.01), among young women under 30 (n = 7, 14.89%) and older 30 years (n = 11, 15.07%) than in the CG (n = 1, 8.33% and 0, respectively) Smoking increased the risk of CIN I by 2.2 times [95% CI 1.4-3.5], CIN II - 2.3 times [95% CI 1.3-3.7] in young women under 30, and in women over 30, the risk of CIN I increased 4.4 times [95% CI 1, 7-8.4], and CIN II - 4.8 times [95% CI 2.1-7.9]. Among the patients of the CIN I and CIN II groups of women with irregular sex life (less often 1-2 times a month), there were statistically significant (p <0.01, p <0.05) more (n = 8, 10.26% and n = 4, 9.52%, respectively) before and over 30 years old (n = 16, 20.5%; n = 9, 21.43%, respectively) than in the CG (n = 0 and n = 1, 3, 33%, respectively) in both age groups. In these women over 30 years of age, the risk of developing CIN I and CIN II was 2.87 times higher [95% CI 1.37-6.1] and 1.86 times [95% CI 1.1-3.1] respectively. At the age of less than 30 years, this factor was not a risk factor (Table 1).Table 1. Comparative characteristics of the surveyed women
 |
| |
|
74.47% of young women and 65.75% over 30 years old in the main group had regular sex life, while in the CG all 100% of young women had regular sex life, and after 30 years old - 94.4%.The risk of developing CIN I and II from a large number of births increased in women over 30 years old - for CIN I it was 2.1 [95% CI 1.2-4.1], and for CIN II - 1.76 [95% CI 1.1-3.2].Among women over 30 years old in the CG, the number of abortions was statistically significant (p <0.01) lower (n = 1, 5.56%) than in the CIN I (n = 20, 25.64%) and CIN II (n = 22, 52.38%). 2 or more abortions in anamnesis increased the risk of CIN I by 3.8 times [95% CI 1.8-7.1] and CIN II by 2.6 [95% CI 1.8-4.4] in women over 30 years of age. In the group of patients younger than 30 years in comparison with the CG, statistically significant (p <0.01) was higher in the CIN I and CIN II groups of patients with two or more abortions in the anamnesis (n = 9, 11.54% and n = 13, 30.95%, respectively), which increased the risk of CIN I by 2.2 times [95% CI 1.4-3.8] and CIN II - by 1.86 times [95% CI 1.1-3.2]...Anamnesis of the last year before the study of inflammatory diseases, nonspecific inflammatory pathologies of CM is presented in Table 2.Table 2. Anamnestic data of gynecological pathology for the last year
 |
| |
|
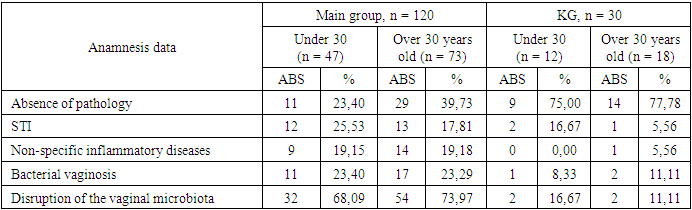
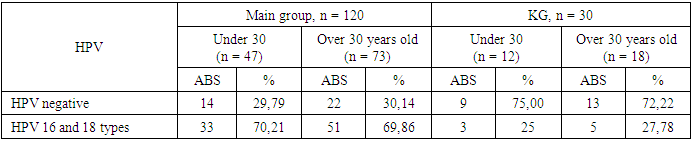
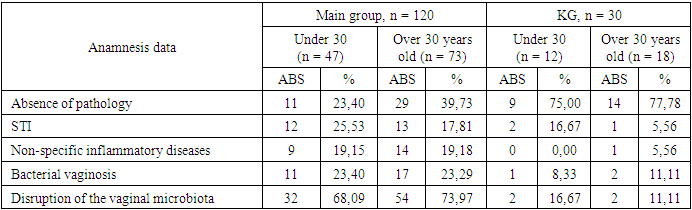
In the CG among young women, the frequency of STIs was (n = 2, 15.2%) and was statistically significantly (p <0.01) lower in comparison with groups I and II (n = 5, 6.41% and n = 7, 16.67%, respectively). In women over 30 years old in the CG, STIs were statistically significant (p <0.01) less often in (n = 1, 3.33%) than in groups I and II (n = 6, 7.69%; n = 7, 16.67%, respectively). STIs within a year increased the risk of developing CIN I in women over 30 years of age 3 times [95% CI 1.4-5.7], CIN II - 2.1 times [95% CI 1.2-3.8], in women under 30 years of age was practically no risk factor for CIN II and increased the risk of CIN I by 1.86 times [95% CI 1.3-3.1]. Nonspecific inflammatory diseases in groups I and II (n = 4, 5.13%; n = 5, 11.9%, respectively) occurred statistically significantly more often (p <0.01) than in the CG (n = 0) in patients up to 30 years, which increases the risk of CIN I by 2.3 times [95% CI 1.4-9.7] and CIN II - 1.8 times [95% CI 1.1-3.1]. In women over 30 years of age in the CG, nonspecific cervicitis was statistically significantly less frequent (n = 1, 8.33%) than in groups I and II (n = 8, 10.26% and n = 6, 14.29%, respectively), which increased the risk of CIN I by 3.86 times [95% CI 1.4-4.8], and CIN II by 3.5 times [95% CI 1.5-7.1]. The frequency of bacterial vaginosis in CG women under 30 years old was (n = 1, 3.33%) and was statistically significantly (p <0.01) lower than in groups I and II (n = 7, 8.97% and n = 4, 9.52%, respectively). In patients under 30 years of age, the risk of CIN I increased by 2 times [95% CI 1.1-3.6] and CIN II by 1.5 times [95% CI 1.2-2.7]. Bacterial vaginosis in the history of CG women over 30 was also statistically significant (p <0.01) less frequently (n = 2, 6.66%) than in groups I and II (n = 7, 8.97% and n = 10, 23.8%, respectively), their risk of CIN I increased by 3.5 [95% CI 1.7-7.6] and CIN II - by 2.1 times [95% CI 1.4-4, 2].Violation of the vaginal microbiota in CG women under 30 is statistically significant (p <0.01) less frequently (n = 2, 6.66%) than in groups I and II (n = 14, 17.95% and n = 18, 42.86%, respectively), which increased the risk of CIN I by 1.8 times [95% CI 1.4-4.1] and CIN II by 1.5 times [95% CI 1.0-2.2]. In the age group after 30 years in the CG, the violation of the vaginal microbiota was statistically significant (p <0.05) less often (n = 2, 6.66%) than in groups I and II (n = 31, 39.74% and n = 23, 54.76%, respectively), which increased the risk of CIN I by 2.1 times [95% CI 1.8-4.7] and CIN II by 1.7 times [95% CI 1.2-3, 6].It should be remembered that HPV persistence is recognized as the leading factor of CIN and cervical cancer [9,10,11]. The HPV status of the women studied is presented in Table 3.Table 3. History of HPV types 16 and 18 in the study groups (p <0.01)
 |
| |
|
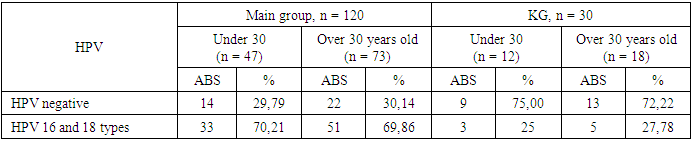
With a positive HPV test in young women under 30, the risk of developing CIN I increased by 3.1 times [95% CI 1.7-7.6] and CIN II by 2 times [95% CI 1.4-3.8 ]. In patients over 30 years of age, the presence of HPV was found statistically significantly more often (p <0.01) than in the CG (n = 3, 9.99%), the risk of developing CIN II increased 2.1 times [95% CI 1.7- 4.3], CIN I - 2.3 [95% CI 1.5-4.8].In the CG, HPV-negative women under 30 years old were statistically significant (p <0.05) more (n = 9, 75%) in comparison with the number of patients in groups I and II (n = 8, 24.24% and n = 6, 42.86% of the number of women of this age in each group, respectively). HPV negative status reduced the risk of CIN I by 4.6 times [95% CI 1.8-9.7] and CIN II by 5.3 times [95% CI 1.6-11.8]. In patients over 30 years of age in the CG, the incidence of negative HPV status is statistically significantly higher (n = 13, 72.2%) than in groups I and II (n = 10, 22.22% and n = 12, 42.86% of the number of women of this age in each group, respectively). HPV negative status reduced the risk of CIN I by 6.4 times [95% CI 1.5-16.7] and CIN II by 5.8 times [95% CI 1.9-16.9].Unprotected sex was found statistically significantly more often (p <0.01) under the age of 30 in groups I and II (n = 19, 57.58% and n = 14, 100% of the number of women of this age in each group, respectively). compared with the CG (n = 3, 25% of the number of women of this age in the group), which increased the risk of developing CIN I - by 2.3 times [95% CI 1.2-4.3] and CIN II - by 2, 1 time [95% CI 1.3-3.8]. Women over 30 years of age practiced unprotected sex statistically significantly (p <0.01) less often in the CG (n = 4, 22.22% of the number of women of this age in the group) than in groups I and II (n = 21, 46, 67% and n = 23, 82.14% of the number of women of this age in each group, respectively), which increased the risk of developing CIN I - 3 times [95% CI 1.3-7.5] and CIN II - 2 times, 3 times [95% CI 1.4-4.8].Women in the CG under 30 used condoms statistically significantly more often (p <0.01) (n = 9, 75% of the number of women of this age in the group) than in groups I and II (n = 14, 42.42% and n = 0 of the number of women of this age in each group, respectively), which reduced the risk of developing CIN I - 2.2 times (95% CI 1.4-3.5) and CIN II - 2.2 times [95% CI 1.3-4.8].Among women over 30 years old, condoms were used statistically more often (p <0.01) in the CG (n = 14, 77.8% of the number of women of this age in the group) than in groups I and II (n = 24, 53.33% and n = 5, 17.86% of the number of women of this age in each group, respectively). No risk reduction was found in subgroups over 30 years of age.Data on the strength of the influence of risk factors on the development of CIN I and CIN II are presented in Table 4.Table 4. The strength of the influence of risk factors on the development of CIN I and CIN II
 |
| |
|
In the aspect of assessing the effectiveness of reducing risk factors for patients, we conducted explanatory conversations and proved the need to minimize their impact. Thus, among women with CIN I (n = 78), 29 (37.18%) women tried to minimize the number of risk factors, and during the repeated comprehensive examination, no one had CM neoplasia, while 49 (62.82%) did not heed the recommendations doctor and practically did not change their lifestyle. Of these women, 23(46.94%) within 1 year after the primary conservative treatment and the absence of CIN I, we recorded intraepithelial neoplasia CIN I again, which required a course of complex conservative therapy of this pathology. This irrefutably proves the importance of leveling risk factors for women's health.
4. Conclusions
1. Smoking, irregular sex life, unprotected contacts and frequent change of partners, a large number of births and abortions, as well as the HPV-positive status of patients are risk factors for the occurrence and development of intraepithelial neoplasia of CM, the leveling of which depends on the patients, therefore, understanding the strength and importance of them influence is one of the guarantors of the health of CMM and women in general.2. The leveling of risk factors for cervical intraepithelial neoplasias increases the period of absence of pathology in women of any age, especially in the risk group - 30-49 years.
References
| [1] | Kaprin A.D., Starinskiy V.V., Petrova G.V. The state of cancer care for the population of Russia in 2018. - Ministry of Health of Russia. 2019. - 236s. |
| [2] | Prilepskaya V.N. Diseases of the cervix and genital infections: M: GEOTAR-Media. 2016. -- 384 s. |
| [3] | Rakhmanova Zh.A. Epidemiological features of cervical cancer // Eurasian Bulletin of Pediatrics. - 2019. - No. 3. - p. 238-244. |
| [4] | Rogovskaya S.I. Practical colposcopy. - M.: GEOTAR- Media, 2011. -- 240s. |
| [5] | Savelyeva G.M., Sukhikh G.T., Serov V.N., Radzinsky V.E. National Guide to Gynecology. M.: GEOTAR-Media, 2017. 989 p. |
| [6] | Benard V. B. et al. Population-based incidence rates of cervical intraepithelial neoplasia in the human papillomavirus vaccine era // JAMA oncology. - 2017. - T. 3. - No. 6. - S. 833-837., Doi: 10.1001 / jamaoncol.2016.3609. |
| [7] | Bornstein J, Bentley J, Bosze P, Girardi F, Haefner H et al. 2011 IFCPC colposcopic nomenclature. In preparation for publication // https://ifcpc.org/newWP/wp-content/uploads/2017/10/nomenclature7-11.pdf. |
| [8] | Mark K, Frost A, Hussey H, Lopez-Acevedo M, Burke AE. Rates of regression of cervical dysplasia between initial biopsy and excisional procedure in routine clinical practice. // Arch Gynecol Obstet. 2019. - No. 299 (3). - p. 841-846. |
| [9] | Polman NJ, Ebisch RMF, Heideman DAM, Melchers WJG, Bekkers RLM. Performance of human papillomavirus testing on self-collected versus clinician-collected samples for the detection of cervical intraepithelial neoplasia of grade 2 or worse: a randomized, paired screen-positive, non-inferiority trial. // Lancet Oncol. 2019. - No. 20 (2). - p. 229-238. |
| [10] | Polman NJ, Snijders PJF, Kenter GG, Berkhof J. HPV-based cervical screening: Rationale, expectations and future perspectives of the new Dutch screening program. // Prev Med. 2019. - No. 119. - p. 108-117. |
| [11] | Sanad A.S., Kamel H. H., Hasan M. M. Prevalence of cervical intraepithelial neoplasia (CIN) in patients attending Minia Maternity University Hospital // Archives of gynecology and obstetrics. - 2014. - T. 289. - No. 6. - p. 1211-1217., Jun., doi: 10.1007/s00404-013-3109-0. |
| [12] | Shahida S.M. et al. Prevalence of Cervical Intraepithelial Neoplasia in four Upazila of Dhaka Division // Mymensingh medical journal: MMJ. - 2019. - T. 28. - No. 3. - p. 655. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML