Kayumkhodjaev A. A., Khalmuratova M. K.
Republican Specialized Scientific and Practical Medical Center for Surgery Named after Academician V.Vakhidov, Tashkent, Uzbekistan
Correspondence to: Khalmuratova M. K., Republican Specialized Scientific and Practical Medical Center for Surgery Named after Academician V.Vakhidov, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Objective: comparative analysis of the results of plasty in head and neck post-burn defects with axial flaps using improved techniques. Methods. The study included the treatment results of 73 patients with head and neck post-burn defects with using the delto-pectoral flap (DPF), temporal flap (TF), and epaulette flaps (EF). The proposed improvements in the technical aspects of plastic surgery were evaluated in the main group - 41 patients, who underwent plastic surgery with 46 flaps. The comparison group included 32 patients who were operated on using standard plasty techniques with axial flaps on the pedicle. Medium defects (50-120 cm²) of the upper face and neck area prevailed in equal numbers. Most of the patients had a median-lateral unilateral post-burn cicatricial deformity. In terms of functional impairments, grade I (up to an angle of 90°) and II degree (up to an angle of 45°) prevailed. Results. A good functional result was noted in 46.9% of patients in the comparison group and in 67.4% of patients in the main group, satisfactory - in 43.8% in the comparison group and in 32.6% in the main group, an unsatisfactory result was also noted in 9, 4% of patients from the comparison group (p=0.044). A good aesthetic result remained in the comparison group in 34.4% of cases, in the main group - 54.3%, satisfactory - in the comparison group in 56.3%, in the main group - 45.7%. Unsatisfactory aesthetic results in the comparison group were 9.4%, while in the main group they were not observed (0.0%) (p=0.042). Conclusion. The studies made it possible to concretize the indications for plasty with axial flaps in head and neck post-burn defects. The use of the proposed methods for improving vascularization and implantation of axial flaps for plasty of post-burn head and neck defects made it possible to reduce the incidence of specific complications, to reduce the need for corrective interventions after the main stages of plasty, thereby reducing the total number of reconstructive stages of plastic surgery, as well as improving long-term functional and aesthetic results.
Keywords:
Post-burn cicatricial defects of the head and neck, Plastic microsurgery, Delto-pectoral flap, Temportemporal flap, Epaulette flap, Analysis of results
Cite this paper: Kayumkhodjaev A. A., Khalmuratova M. K., Results of Plastic Surgery with Axial Flaps in Head and Neck Post-Burn Defects, American Journal of Medicine and Medical Sciences, Vol. 11 No. 11, 2021, pp. 759-764. doi: 10.5923/j.ajmms.20211111.03.
1. Introduction
Burns are a medical and socio-economic problem, and to this day, the treatment of burns remains one of the most time-consuming and expensive procedures, as it immediately incorporates many skills in practical surgery, microbiology, anesthesiology and resuscitation [1,2]. In this area of research in the field of the pathogenesis of burn disease, its complications are of great importance in the development of modern ways of surgical treatment for extensive burn injuries, including the head, neck and upper extremities, which, in turn, can affect many specialized anatomical structures, and are critical for the quality of life and human functioning [2,3].Current trends in combustiology are aimed at surgical interventions in the early stages [3,4]. Head and neck burns can increase the tendency to form pathological scars is observed even with superficial burns, not to mention deep burns, when the forming keloid or hypertrophic scars cause a sharp deterioration in the patient's appearance, up to deformity [3,4].The relevance and great practical importance of the development of issues of surgical correction of post-burn cicatricial deformities is determined not only by the high frequency of their occurrence, but also by certain difficulties in choosing the optimal way to eliminate them [6,7]. The problem is that today there are no universal methods that could treat these patients, and the use of the entire modern arsenal of tools that is in service in reconstructive surgery sometimes does not give the desired result [7,8].The article presents the comparative results of plasty of post-burn cicatricial defects of the head and neck with axial flaps according to the improved techniques developed at the Republican Specialized Scientific and Practical Medical Center for Surgery named after academician V.Vakhidov (Tashkent, Uzbekistan).
2. Material and Methods
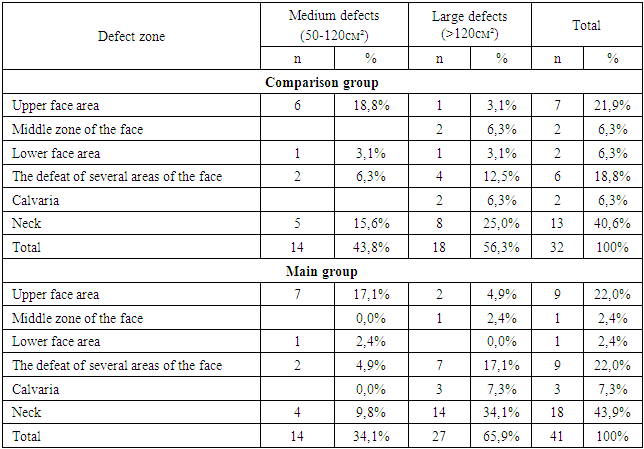
The study included the results of treatment of 73 patients with cicatricial defects of the head and neck with axial flaps: delto-pectoral flap (DPF), temporal temporal flap (TTF), and epaulette flaps (EF). The proposed improvements in some technical aspects of plastic surgery were evaluated in the main group - 41 patients, who underwent plastic surgery with 46 flaps (in 5 patients, 2 flaps were applied at the same time). The comparison group included 32 patients who were operated on according to standard methods of plasty with axial flaps on the pedicle. Each type of flap included a certain number of stages of plasty, in particular, if for EL and TTF two stages were required, then for DPF three stages are required due to the inclusion of the stage stem formation. In general, in the comparison group, DPF was applied in 12 (37.5%) patients, TTF in 7 (21.9%) and EF, in the main group in 37.0% (17 patients), 23.9% (11 patients) and 39.1% (18 patients), respectively. The distribution of patients by zones and extent of the lesion is given in table 1 and 2.Table 1. Distribution of patients by zones and nature of the defect
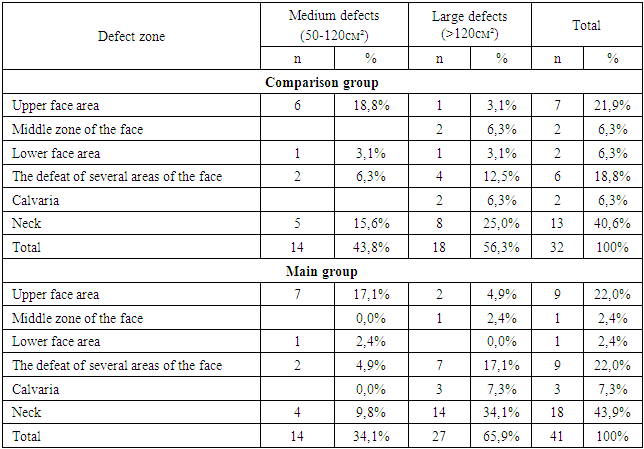 |
| |
|
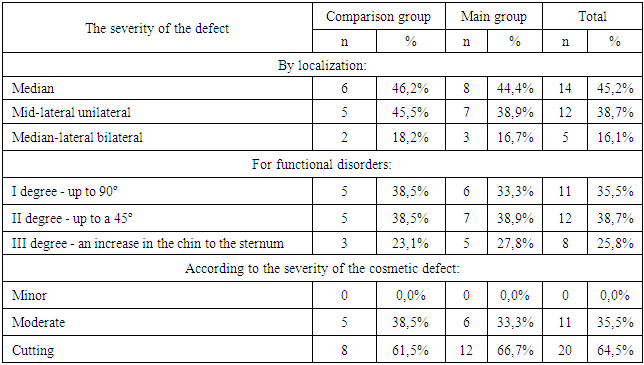
Table 2. Distribution of patients according to the classification of post-burn cicatricial deformities of the neck by A.A. Yudenich (1989)
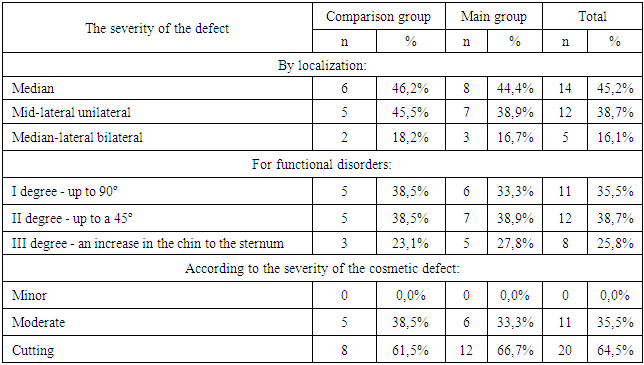 |
| |
|
In the main group, patients received treatment according to the developed indications for plasty of post-burn cicatricial defects of the head and neck area with axial flaps.DPF plastic:• medium and large deep post-burn cicatricial defects and deformities of the facial region of the head, including open defects whose bottom is exposed bone, cartilage (the listed anatomical structures, if they are devoid of periosteum, the perichondrium does not have sufficient blood supply for engraftment of a skin graft); defects with poorly vascularized surrounding tissues (the flap carries additional blood supply to the poorly vascularized recipient area due to the preserved vascular pedicle);• cicatricial defects of the underlying anatomical structures requiring reconstruction (eyelids, lips, auricle, nose, cheeks, trachea);• the use of "prefabricated" (pre-prepared) flaps for one-step reconstruction of soft tissues and underlying structures (flaps with implanted bone and cartilage grafts);• the need to create a sufficient layer of soft tissue over the bone protrusions;• open cavities (through defects) of the facial region (upper jaw, buccal region, nose region). The inner lining of the defect (mucous membrane) is formed due to the epidermis of the distal portion of the flap;• restoration of sensitivity in the reconstruction zone;• situations when future surgical interventions are planned on deep-lying structures in the area of the scar (implantation of a bone fragment, cartilage,Plastic surgery with delto-pectoral-occipital flap:• extensive post-burn cicatricial defects of the cranial vault, when there is no normal surrounding tissue for expander dermotension, there are no recipient vessels for microsurgical atuotransplantation of flaps;Plastic surgery with a temporo-temporal skin-fascial axial flap on a vascular pedicle:• with the consequences of a deep burn of the eyebrow area, when, due to a pronounced deep scarring process, it is impossible to use free skin transplantation from the scalp of the cranial vault, transplantation of "mini grafts" of hair follicles.• eyebrow defect in combination with cicatricial deformity of the periorbital region, eversion of the eyelids. A sufficient volume of the blood-supplied flap allows correcting functional disorders as well.Plastic with an epaulet (shoulder) flap:• the presence of grade II-III cicatricial contracture of the neck, combined with a cicatricial lesion of the chest, upper limb, when the movement of a large amount of plastic material (Filatov stem, delto-pectoral axial flap) is difficult;• tendency to keloidosis, which casts doubt on the success of free skin grafts or local plastic surgeries;• deep extensive post-burn scar with damage to the underlying structures (muscles, trachea, larynx);• the presence of extensive post-burn cicatricial deformities of the neck, when the patient, due to previous treatment of burn surfaces, used intact body parts for autodermoplasty.
3. Results
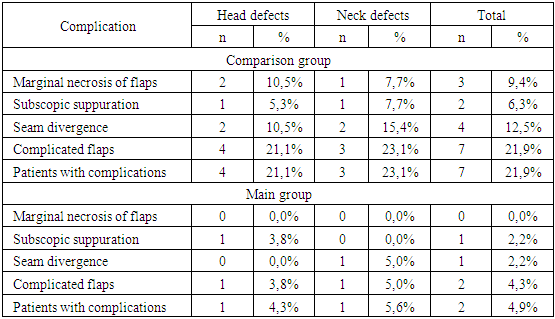
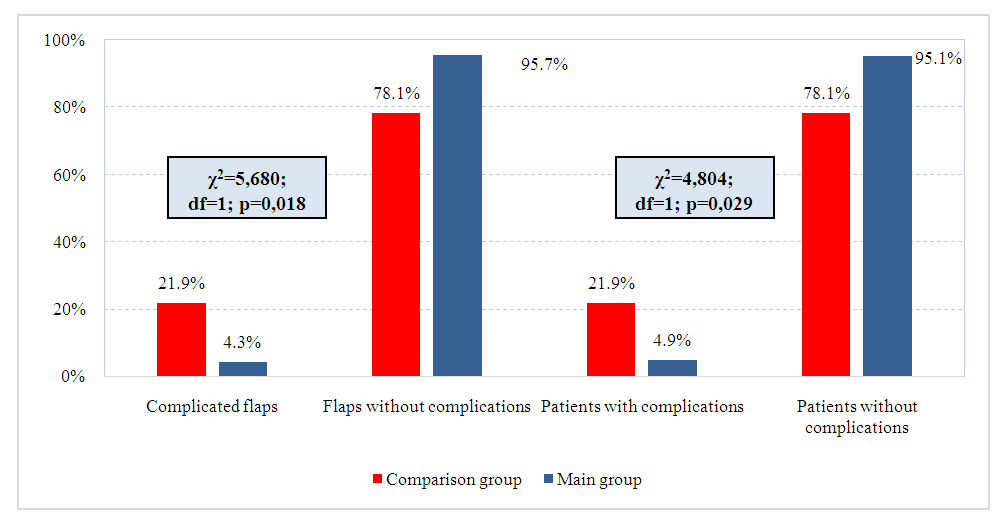
In case of head defects in the main group, sub-flap suppuration, flaps with complications and patients with complications after plastic surgery of DPF prevail in equal numbers (6.7%). In the comparison group, after TTF plasty, marginal flap necrosis (14.3%), suture divergence (14.3%) and flap complications (28.6%) develop. With neck defects in the comparison group, flaps with complications and patients with complications were observed after plastic surgery.Table 3 shows the summary rate of complications after microsurgical reconstruction of head and neck defects. Thus, in the grading group with head and neck defects, flaps with complications prevailed and patients with complications in equal numbers - 7 patients (21.9%). In the main group, flaps with complications in head and neck defects accounted for 4.3%, and patients with complications - 4.9%. No marginal flap necrosis was observed in the study group (0.0%).Table 3. Summary incidence of complications after microsurgical reconstruction of head and neck defects
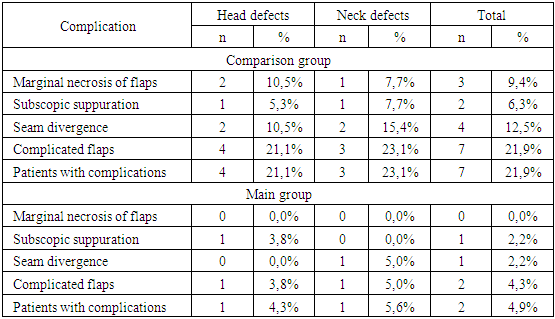 |
| |
|
As can be seen from Fig. 1, flaps without complications were observed in 78.1% of patients, in the main group - in 95.7%. Complications of flaps were observed in 21.9% of patients in the comparison group and in 4.4% in the main group. There were 7 patients with complications in the comparison group (21.9%), in the main group - 2 (4.9%). The absence of complications was observed in 78.1% of patients in the comparison group and in 95.1% of patients in the main group.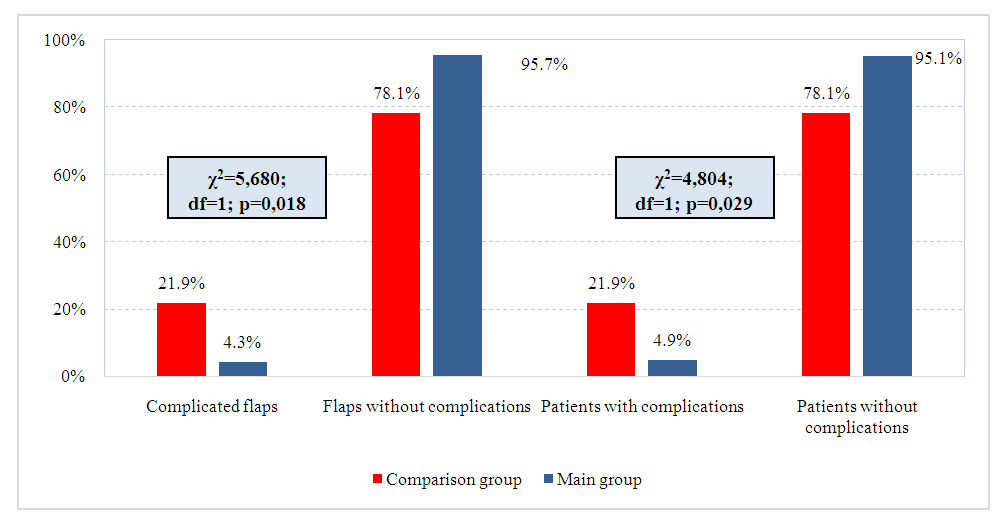 | Figure 1. Distribution of the proportion of complicated postoperative course by groups |
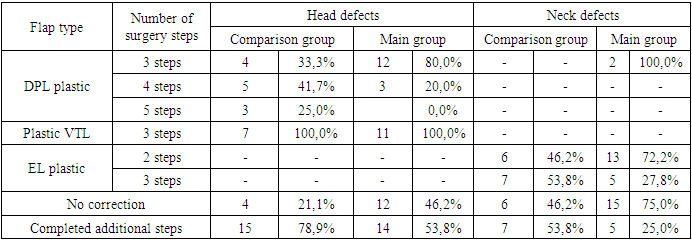
According to the table 4 shows that DPL plastic surgery for head defects is carried out in 3 stages, in the comparison group it is used in 33.3% of cases, and in the main group - 80.0%. TTF plastic surgery for head defects is also performed in 3 stages and was successfully implemented in all patients (100.0%). EF plastic surgery (2 stages) of neck defects in the comparative group was 46.2%, and in the main group - 72.2%. The results of operations without correction in the comparison group for head defects were 21.1%, and in the main group - 46.2%. For neck defects without flap correction, plastic was performed in 46.2% of patients in the comparison group, in the main group - 75.0%. Head defect plasty with additional stages: in the comparison group it was 78.9%, in the main group - 53.8%. And with neck defects in the main group - 25.0%, while in the comparison group - 53.8%.Table 4. Comparative number of performed plastic stages (from the number of flaps)
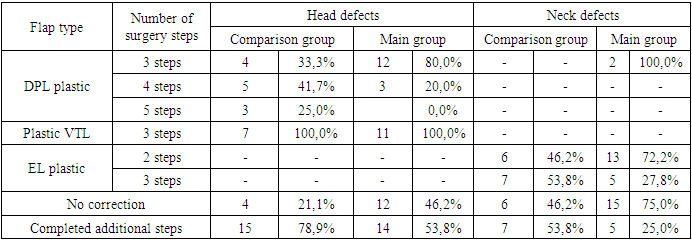 |
| |
|
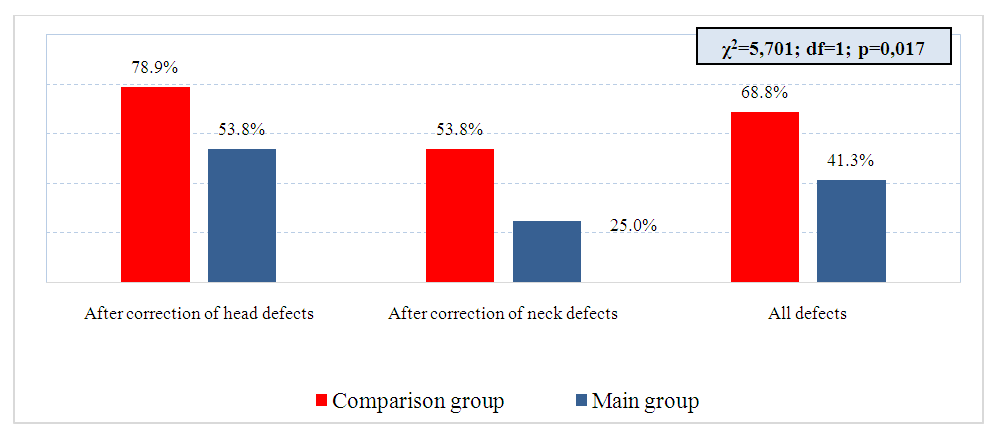
The obtained data on the distribution of patients by the frequency of corrective interventions in the long-term period, depending on the type of operation, showed that lipodermectomy with contour plastics after correction of head defects was used in the comparison group in 31.6% of cases, and in the main group - in 7.7%. Correction of defects with currying interventions was carried out using lipodermectomy with contour plastic and additional liposuction in the comparison group in 53.8% of cases, and in the main group - in 25.0%.As seen in Fig. 2, the frequency of corrective interventions in the long-term period after correction of head defects in the comparison group was 78.9%, in the main group - 53.8%; after correction of neck defects in the comparison group - 53.8%, in the main group - 25.0%. At the same time, this indicator for all defects in the comparison group is equal to 68.8%, and in the main group - 41.3%.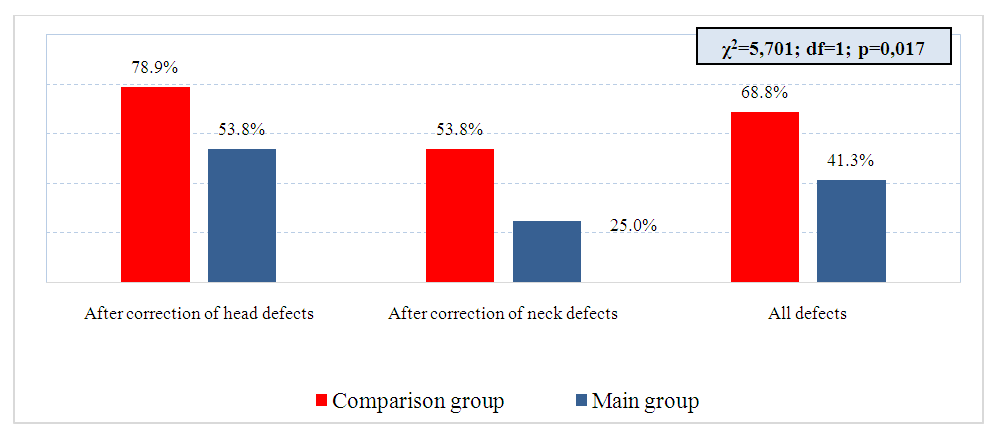 | Figure 2. Consolidated frequency of corrective interventions in the long-term period |
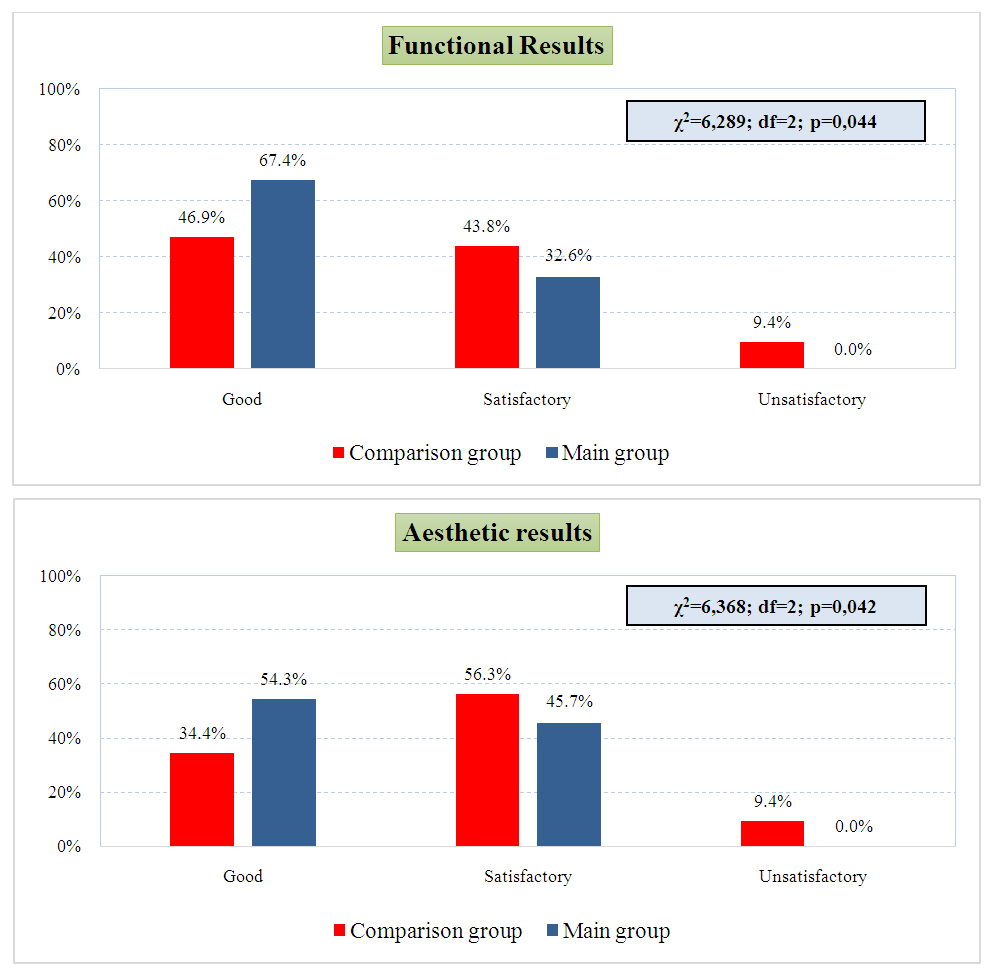
In the study groups, the correction of head defects in 2 steps was not performed (0.0%). Three-stage correction of head defects in the comparison group was used in 57.9% of cases, in the main group - 88.5%, and in 4 stages - in the main group in 11.5% of patients, in the comparative group - in 26.3%. In 5 stages, plastic was performed in the comparative group in 15.8% of patients, and in the main group - 0.0%. In the case of neck defects, 3-stage plastic surgery prevailed in the comparison group (53.8%), in the main group, two-stage plastic surgery (65.0%).Considering the correction of all defects, it was noted that in the main group and in the comparison group, 3-stage operations prevailed - 65.2% and 56.3%, respectively.Long-term results were followed in all patients. The obtained data of plastic surgery, taking into account the type of flap, showed that in the head area, plastic surgery with a delto-pectoral flap gave good results in the comparative group (41.7%), as well as in the main group - 66.7%. groups: in the main group - 81.8%, in the comparison group - 71.4%. Good functional result with neck defects was in 38.5% of patients in the comparative group, and in the main group - 61.1%.The data obtained on the aesthetic results, taking into account the type of flap, showed that in case of head defects, plastic surgery by the deltopectoral method showed good results in 53.3% of patients in the main group, but in the comparison group the indicators were slightly lower - 33.3%. Plastic surgery with a temporoparietal flap in the head area was implemented in the main group in 72.7% of cases and in the comparative group - in 42.9%. In case of neck defects, good functional results, in plastic with an epaulet flap, were in 30.8% of patients in the comparative group, and in 50.0% of the main group.The results of plasty with axial flaps, depending on the localization of the defect, showed that a good functional result of the head defect was in 73.1% of patients in the main group, and in the comparison group - in 52.6%. With neck defects, good functional results were observed in 60.0% of cases in the main group and in 38.5% in the comparison group. With head defects, a satisfactory aesthetic result prevailed in the comparison group (57.9%), and in the main group, a good aesthetic result - 61.5%. In the comparison group, a good aesthetic result after neck plastic surgery was in 30.8% of patients, in the main group - in 45.0%.In fig. 3., the summary results of plasty with axial flaps are presented.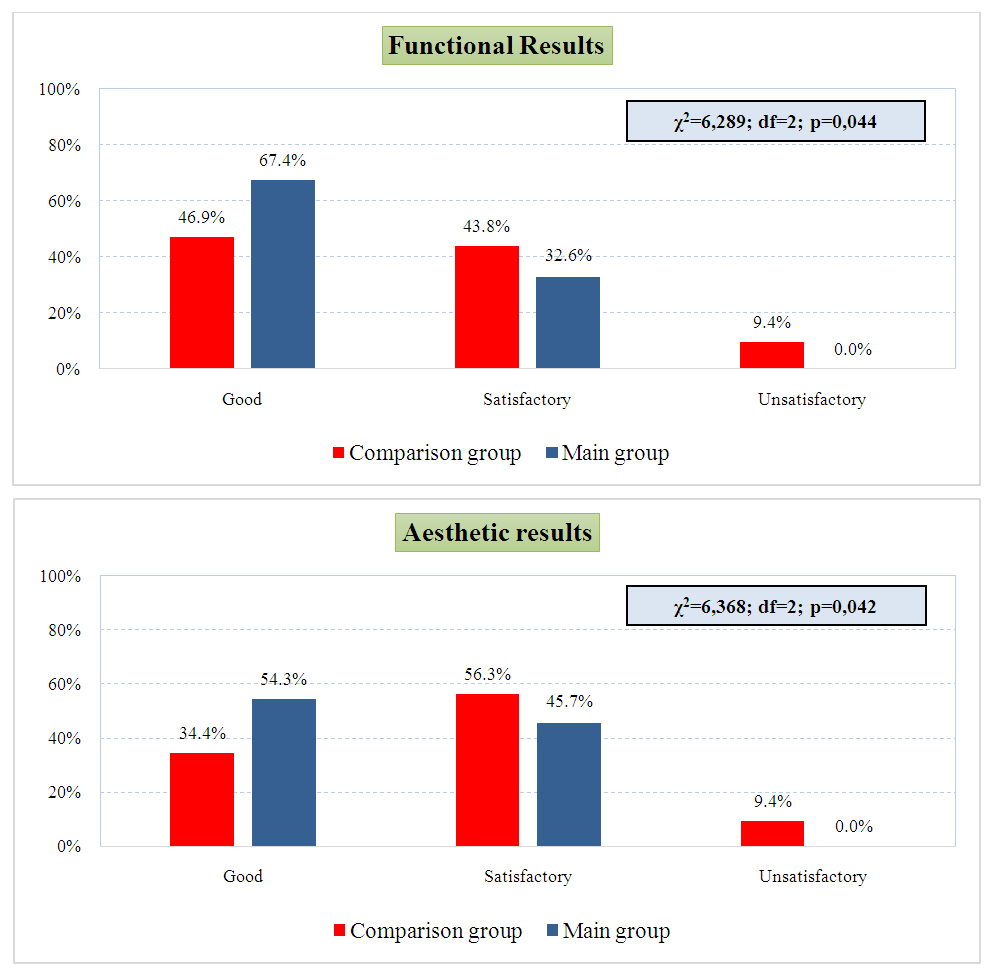 | Figure 3. Summary results of plasty with axial flaps |
Thus, a good functional result was noted in 46.9% of patients in the comparison group and in 67.4% of patients in the main group, satisfactory - in 43.8% in the comparison group and in 32.6% in the main group, an unsatisfactory result was also noted in 9.4% of patients from the comparison group and in patients from the main group, unsatisfactory results were not observed (0.0%) (χ2=6.289; df=2; p=0.044). A good aesthetic result remained in the comparison group in 34.4% of cases, in the main group - 54.3%, satisfactory - in the comparison group in 56.3%, in the main group - 45.7%. Unsatisfactory aesthetic results in the comparison group were 9.4%, while in the main group they were not observed (0.0%) (χ2=6.368; df=2; p=0.042).
4. Conclusions
The conducted studies made it possible to concretize the indications for the plasty of post-burn cicatricial defects of the head and neck with axial flaps. performing corrective interventions after the main stages of plasty, thereby reducing the total number of reconstructive plasty stages, as well as improving long-term functional and aesthetic results.
References
| [1] | Wei FC, Tay SK. Principles and techniques of microvascular surgery. In: Neligan PC, editor. Plastic Surgery. Vol. 1, Principles. 3rd ed. Elsevier; 2013. 587-621. |
| [2] | Masia J, Olivares L, Koshima I, et al. Barcelona consensus on supermicrosurgery. Journal of Reconstructive Microsurgery. 2014; 30: 53-58. |
| [3] | Eskander A, Kang SY, Teknos TN, et al. Advances in midface reconstruction: Beyond the reconstructive ladder. Current Opinion in Otolaryngology & Head and Neck Surgery. 2017; 25(5): 422-430. |
| [4] | Belal A.A., Mohamed EM, M.D.; Mohamed IH, Mohamed OK. Regional Flaps in Coverage of Facial Defects: Our Experience. Egypt, J. Plast. Reconstr. Surg. 2018; 42(1): 45-53. |
| [5] | Ray E. Head and neck reconstructive surgery. Cancer Treatment and Research. 2018; 174: 123-143. |
| [6] | Murphy BD, Farhadi J, Masia J, et al. Indications and controversies for abdominally-based complete autologus tissue breast reconstruction. Clinics in Plastic Surgery. Jan 2018; 45(1): 83-91. |
| [7] | Kania K, Chang DK, Abu-Ghname A, Reece EM, Chu CK, Maricevich M, Buchanan EP, Winocour S. Microsurgery Training in Plastic Surgery. Plast Reconstr Surg Glob Open. 2020 Jul 17; 8(7): e2898. doi: 10.1097/GOX.0000000000002898. |
| [8] | Frederick JW, Sweeny L, Carroll WR, Peters GE, Rosenthal EL. Outcomes in head and neck reconstruction by surgical site and donor site. Laryngoscope. 2013; 123(7): 1612-7. doi: 10.1002/lary.23775. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML