-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(10): 747-751
doi:10.5923/j.ajmms.20211110.18
Received: Oct. 10, 2021; Accepted: Oct. 26, 2021; Published: Oct. 30, 2021

Corrective Osteotomy of the Femur for Aseptic Necrosis of the Femoral Head after Bloodless Reduction of Congenital Dislocation in Preschool Children
Akhror Makhmutovich Djuraev1, Khojaakhmed Shaykhislamovich Alpysbaev2, Elyar Abduvalievich Tapilov3
1Doctor of Medical Sciences, Professor, Head of the Department of Pediatric Orthopedics of the Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics of the Ministry of Health of the Republic of Uzbekistan
2Candidate of Medical Sciences, Deputy Director for Medical Work, Head of the Department of Hip Pathology of the Republican Center for Pediatric Orthopedics of the Ministry of Health of the Republic of Uzbekistan
3Resident Doctor, Department of Pathology of the Hip Joint of the Republican Center for Pediatric Orthopedics of the Ministry of Health of the Republic of Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The prompt results of treatment of 72 children aged 7 to 12 years with aseptic necrosis of the femoral head after bloodless diminishment of intrinsic hip dislocation were analyzed. When treating patients, the following sorts of surgical treatment were used: extra-articular or open centering of the femoral head with intertrochanteric torsion-varizing or devarizing and rotational osteotomy of the femur with its “apophysiodesis” of the more noteworthy trochanter. In the case of acetabular dysplasia, the over interventions can be supplemented with acetabular plastic surgery. Pain and lameness vanished in all patients, internal rotation of the lower extremities when strolling, and the range of motion within the hip joint improved. Improved radiometric parameters characterizing the proportion of the acetabulum and the head of the femur and the angular values of the hip joint and proximal femur. Corrective intertrochanteric-rotational osteotomies of the femurs can be successfully used in the treatment of deformities of the PFB in aseptic necrosis of the femoral head (ANFH) in preschool children. The operation allows you to change the spatial position of the head and neck of the femur in three planes and normalize the position of the greater trochanter.
Keywords: Congenital hip dislocation, Aseptic necrosis of the femoral head, Hip joint, Deformity of the proximal femur, Surgical correction
Cite this paper: Akhror Makhmutovich Djuraev, Khojaakhmed Shaykhislamovich Alpysbaev, Elyar Abduvalievich Tapilov, Corrective Osteotomy of the Femur for Aseptic Necrosis of the Femoral Head after Bloodless Reduction of Congenital Dislocation in Preschool Children, American Journal of Medicine and Medical Sciences, Vol. 11 No. 10, 2021, pp. 747-751. doi: 10.5923/j.ajmms.20211110.18.
Article Outline
1. Introduction
- Relevance: Aseptic necrosis of the femoral head (ANFH) could be a frequent and serious complication that occurs after reduction of congenital hip dislocation in children, driving to the early improvement of dysplastic coxarthrosis and inability, the leading neurotic activating mechanism of which is ischemia of the femoral head [1, pp. 314-315; 5, pp. 218; 8, pp. 229-230]. According to the literature, the frequency of this complication with a closed decrease of hip disengagement changes from 10 to 60% [13, pp. 552-562; 18, pp. 4-12; 20]. Most experts recognize that the driving part within the pathogenesis of aseptic necrosis is the iatrogenic disturbance of blood supply in the proximal femur [4, pp. 255; 9, 35-36; 19, pp. 35-36]. Undoubtedly, repeated attempts at reduction, which end in vain regardless of the cause, in combination with prolonged immobilization in a plaster cast in the antephysiological position of the lower extremities lead to iatrogenic damage to the joint structure, cause vascular disorders, which ultimately initiates the occurrence of various deformities of the femoral head [2, pp. 22; 3, pp. 6-14; 4, 255; 6, pp. 182; 10, pp. 248; 15. pp. 54-59]. The severity of residual deformities depends on the severity of the lesion of the ossification nucleus of the epiphysis of the femoral head, at the beginning of the pathological process [16, pp. 196-202; 20]. Deformities of the proximal femur (PFB) in children after AFH are not uncommon and often require complex surgical interventions [11, pp. 249-25017; 21, pp. 302-314]. This gives the problem under study not only a medical but also a social character. Treatment of type II deformity of POBD according to Kalamchi-MacEwen: is extremely difficult, and the most difficult is the correction of multiplanar deformities, in which the main task of the intervention is to normalize all deviations, “as far as possible” [22, pp. 209-226], and the works devoted to it are isolated [19, pp. 22-28]. To normalize the relationships in the joint, the surgical method is the only one, and N. Clarke [14, pp. 434-439] saw the main task of treating deformities after aseptic necrosis in their “minimization by surgery”, and Y.I. Pozdnikin [9, pp. 35-36] considered the restoration of the shape and joint function. The presence of such a variety of methods of treatment indicates their insufficient effectiveness, the absence of justified criteria for choosing rational methods of surgical interventions. It is believed that type II deformity according to Kalamchi occurs most often and ranges from 25 to 61% [17, pp. 1962-1700; 19, pp. 22-28]. The problem of the treatment of ANFH and the consequences of impaired growth of the lateral part of the proximal femoral growth plate does not always lead to satisfactory results [7, pp. 149-1151; 11, pp. 249-250; 12, pp. 138-145; 17, pp. 1962-1700; 22, pp. 209-226].The aim of this study is to evaluate the effectiveness of using corrective intertrochanteric osteotomies of the femur in preschool children with aseptic necrosis of the femoral head.
2. Materials and Research Methods
- The immediate results of treatment of 72 children, aged from 7 to 12 years, with deformities of the proximal femur with ANFH after bloodless reduction of congenital hip dislocation were analyzed. All patients had a multiplanar deformation of the proximal end of the femur: a decrease or increase in the cervico-shaft angle of the femur, valgus deviation of the pineal gland, shortening of the femoral neck, high standing of the greater trochanter, and a negative value of the articulotrochanteric distance. During the X-ray examination of children, the X-ray of the hip joints was performed in the anteroposterior projection with the middle position of the hips and with internal rotation, as well as in the Lauenstein position. Radiographs were used to measure parameters characterizing the angular values of the hip joint and proximal femur, the angle of the vertical tilt of the depression, the angle of vertical correspondence, the acetabular angle, the cervico-diaphyseal angle, the angle of anteversion, the Alsberg angle, and the coefficient of bone coverage. For a detailed analysis of the ongoing anatomical changes, we studied the indicators characterizing the ratio of the femoral head to the greater trochanter in the frontal plane: articulo-trochanteric distance (ATD); trochanter-trochanter distance (TTD); Articulo-rotational distance (ARD) Indication for the use of corrective osteotomies was a combination of clinical and radiological data - lameness, faulty positioning of the lower extremities, significant limitation of hip abduction, weakness of the gluteal muscles, impaired relationships in the hip joint, subluxation of the femoral head, deformity of the proximal femur : plow valga (caudal position of the greater trochanter), plow vara (cranial position of the greater trochanter), plow breva, high position relative to the head of the femur (relative overgrowth of the greater trochanter), sohamagna, and not the shortening of the lower limb itself. The decision was made strictly individually: for each individual patient, the amount of the proposed correction was determined, taking into account the already occurring irreversible secondary changes (structural scoliosis, pelvic misalignment) and age. When treating patients, the following types of surgical treatment were used: extra-articular centering of the femoral head with intertrochanteric torsion-varizing or devarizing and rotational osteotomy of the femur with “apophysiodesis” of the greater trochanter. In acetabular dysplasia, correcting intertrochanteric osteotomies of the femoral bone were combined with acetabuloplasty, which should be performed simultaneously with femoral osteotomy. The results of treatment were analyzed over a period of 8 months to 3 years. Clinical outcomes were assessed by McKey.
3. The Main Findings and Results
- Clinical example No. 1. Clinical example No. 1. B-i: I.R. 2011 year of birth I / b No. 397. She was admitted to the department with complaints of lameness in the left leg, shortening of the left lower limb and limitation of abduction in the left hip joint. From the anamnesis, congenital dislocation of the right hip was diagnosed at 4 months of age. She was treated on an outpatient basis by applying a plaster cast according to Sheptun for a period of 4.5 months. After removing the plaster cast, a Vilensky splint was put on the lower limbs. 12 months after bloodless reduction, aseptic necrosis of the head of the right femur was diagnosed. In 2018, she turned to our clinic with the above complaints. Dose: Congenital dislocation of the right hip. Condition after bloodless reduction. Residual subluxation of the right thigh due to aseptic necrosis of the head. Deformity of the proximal part of the right femur of type IV according to Kalamchi: coxa vara, coxa breva et antetorsia, hypertrophy of the greater trochanter. Acetabular dysplasia.Clinically: the patient walks independently, limping on the right lower limb. Movement in the hip joints of the sagittal plane in full, extension-180°/0°/180°, flexion-120°/0°/120°, abduction-300/00/500, internal rotation-600/00/400, external rotation-30°/0°/30°. Trendelenburg's symptom is positive on the right.The main manifestation on the anteroposterior radiograph of the pelvis is the lateral inclination of the epiphysis of the femoral head, shortening of the lateral part of the femoral neck compared to the medial part. Joint stability is reduced, the head and neck of the femoral bones are shortened, the cervico-diaphyseal angle (SDA): 1200, the apex of the greater trochanter of the right femur is located closer to the upper pole of the femoral head, (ATD: 10 mm.), Shenton's line break by 1.0 see, acetabular dysplasia.X-ray: otmechaetsya podvyvix head of the left hip with klassicheskoy deformatsiey head of the right hip bone of type II: soxa vara, coxa breva et antetorsia, hypertrophy bolshogo vertela. Acetabular dysplasia. Fig. 1 (a, b).Fig. 1 (a). X-ray of the hip joints in the anteroposterior projection with the middle position of the lower extremities.Fig. 1 (b). X-ray of the hip joints in the anteroposterior projection in the position of internal rotation and abduction of the left lower extremity: the head and neck of the femur are shortened and thickened, centered on the bottom of the acetabulum, SDA: 120°, ATD: has a negative value of -5 mm., Shenton's line rupture, acetabular dysplasia.On 09.12.2018, a surgical intervention was performed: open centering of the head of the right femur with intertrochanteric detorsion-valgus-posterior rotational osteotomy of the femur, apophysiodesis of the greater trochanter and Pemberton's roof of the acetabulum. Fig. 1 (c).Fig. 1 (c): the head of the right femur is centered on the bottom of the acetabulum, intertrochanteric corrective osteotomy of the femur with fixation of bone fragments “L” shaped plate and 3 screws, apophysiodesis of the greater trochanter with 1 screw, pericapsular plasty of the acetabular roof depressions with an inclination of the distal fragment anteriorly, outward and downward, with the insertion of an autograft into the formed groove and its synthesis with a wire. SDU: 1250/1300.On June 21, 2018, the following was performed: removal of the hardware of the proximal part of the right femur and from the wing of the ilium. Fig. 1 (c).The result 2 years after the surgical treatment: the head of the left femur is centered on the bottom of the cavity, with a good covering of the roof of the acetabulum, SDA: 1300/1300, ATD 8 mm. Rice # 1 (d).Fig. 1 (d) STO: the head of the right femur is centered on the bottom of the acetabulum, with satisfactory coverage, complete consolidation of the fragments of the femur in the intertrochanteric region, SDA: 125°/130°, the growth of the greater trochanter of the right femur is suspended, (ATD: 12 mm), the continuity of the Shenton line is restored.
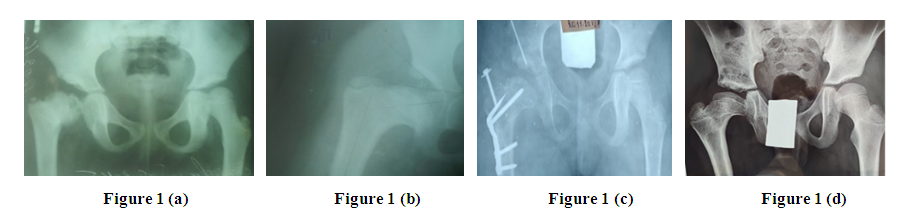 | Figure 1 |
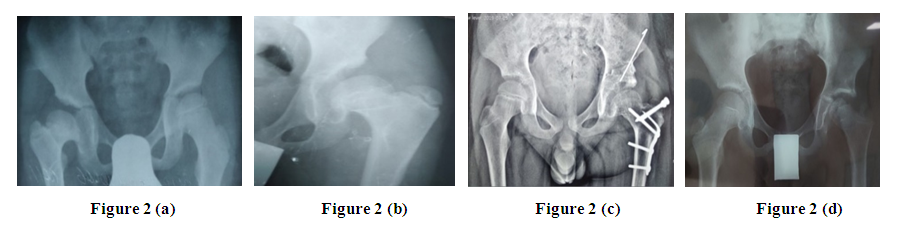 | Figure 2 |
4. Conclusions
- Surgical intervention in childhood must be carried out not only taking into account the existing deviations, but also those deformations that will inevitably arise as a result of the continued functioning of the damaged growth zones of the proximal femur. Dystrophic lesions after bloodless reduction of congenital hip dislocation can affect the head in combination with damage to the growth zone of the femoral neck. Violation of the growth and formation of the proximal femur depends on the premature closure of the growth zone, its partial or total "epiphyseodesis" in one or another of its parts after bloodless reduction. Quite often, the formation of deformity is accompanied by a violation of the stability of the joint, both due to the valgus deviation of the femoral head and in connection with secondary dysplasia of the acetabulum, decentering of the femoral head, incongruence of the articular surfaces, and proximal migration of the greater trochanter. Each type of deformity requires correction of its inherent deviations, including multiplanar ones. Correcting transotrochanteric rotational osteotomies of the femurs can be successfully used in the treatment of deformities in schoolchildren. For acetabular dysplasia, they can be supplemented with acetabular plastic surgery. The operations allow to change the spatial position of the head and neck of the femur in three planes and normalize the position of the greater trochanter. All children who have undergone aseptic necrosis of the femoral head, even without signs of impaired stability of the hip joint, need dynamic observation to select the optimal timing for correction of the emerging deformity, if necessary.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML