-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(10): 690-698
doi:10.5923/j.ajmms.20211110.06
Received: Oct. 5, 2021; Accepted: Oct. 12, 2021; Published: Oct. 30, 2021

Predictions of the Viability of Early Intrauterine Pregnancies by Using Ultrasound Scan Parameters - PEPU Study (A Prospective Cohort Study)
Samarawickrama N. G. C. L.1, Kariyawasam G. L. D.2
1Senior Registrar, Department of Obstetrics & Gynaecology, University of Sri Jayewardenepura, Colombo South Teaching Hospital, Sri Lanka
2Senior Obstetrician & Gynaecologist, Castle Street Hospital fro Women, Sri Lanka
Correspondence to: Samarawickrama N. G. C. L., Senior Registrar, Department of Obstetrics & Gynaecology, University of Sri Jayewardenepura, Colombo South Teaching Hospital, Sri Lanka.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

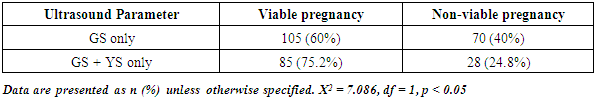
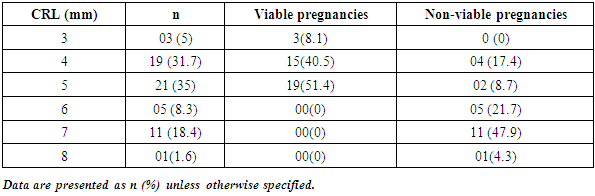
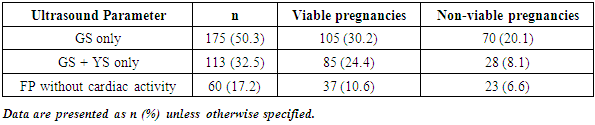
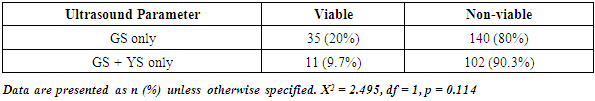
Introduction: There is no uniformity in the evaluation criteria used at present to discriminate viable from non-viable pregnancy by using the ultrasound parameters. Missing a viable pregnancy will unfortunately lead to a termination of one embryo, which may destine to be a human live birth in future. On the other hand, continuous surveillance without demonstrating desirable outcome will increase woman's anxiety over time. Objectives: To determine the minimum ultrasound-scan cut off values to predict the subsequent viability of an intrauterine pregnancy of uncertain viability. Methods: Prospective cohort study carried out in tertiary care hospitals in Sri Lanka. The Sample (n = 348) was categorized in to three groups. End point is to demonstrate fetal cardiac activity. The sensitivity, specificity and false positive rates (FPR) for a miscarriage was calculated. Results: Among the 348 women who were included in the study and diagnosed initially as having pregnancy of uncertain viability, 227 (65%) women were found to have viable pregnancies in subsequent scans. Presence of yolk sac, when compared to gestational sac (GS) only, improves the outcome by increasing the number of viable pregnancies (p < 0.05). In the GS only group when the mean sac diameter (MSD) is 16 mm, the FPR (viable pregnancy) for a miscarriage was 21.9%. At the MSD of 20 mm the FPR declined to 1.9% and above 21 mm there was no misdiagnosis, where FPR is 0%. In the GS with yolk sac group FPR for miscarriage was 20.5% at MSD of 16 mm, 1.3% at 20 mm and 0% beyond 21 mm. In fetal pole without cardiac activity group FPR for miscarriage was 51.4% at crown rump length (CRL) of 4 mm, 17.4% at CRL of 5 mm. Above CRL of 5 mm, FPR was 0% for a non- viable pregnancy. Conclusions and Recommendations: Findings of this study support the current Royal College of Obstetricians and Gynaecologists recommendations. Even though we were unable to demonstrate fetal cardiac activity above MSD of 21 mm, given the consideration of intra and inter observer variability in obtaining USS parameters, it appears to be a safe option to adhere to the current cutoff of 25 mm to avoid any inadvertent interventions. Above 5 mm CRL there were no demonstrable fetal cardiac activity in subsequent scans suggests that inter and intra observer variability adjusted fetal pole cut off of 7 mm is the margin of choice to diagnose a miscarriage.
Keywords: Pregnancy of uncertain viability, Mean sac diameter, Crown rump length, Miscarriage
Cite this paper: Samarawickrama N. G. C. L., Kariyawasam G. L. D., Predictions of the Viability of Early Intrauterine Pregnancies by Using Ultrasound Scan Parameters - PEPU Study (A Prospective Cohort Study), American Journal of Medicine and Medical Sciences, Vol. 11 No. 10, 2021, pp. 690-698. doi: 10.5923/j.ajmms.20211110.06.
Article Outline
1. Introduction
- It is well-recognized fact that significant number of pregnancies ends up as miscarriages instead of progressing in to viable pregnancies. Numbers may reach as high as 50% of total conceptions [1] whereas 12% to 15% of clinically recognized pregnancies [2]. Vaginal bleeding in early pregnancy is one of the common gynecological reasons for hospital admissions. It is well accepted that ultrasonography plays an important role in the diagnosis of the location and viability of pregnancies [3]. Among the indications for early pregnancy scans, vaginal bleeding in early pregnancy, booking scan in early trimesters, abdominal pain with positive urine hCG (human Chorionic Gonadotropin) test are the commonest reasons. Among these scans up to 29% of the cases clinicians unable to readily diagnose the viability of an intrauterine pregnancy. Therefore these patients are categorized as having a Pregnancy of Uncertain Viability (PUV). By definition PUV is the presence of an intrauterine gestational sac of < 20 mm without the demonstrable cardiac activity.These patients may continue their pregnancies as either a viable pregnancy or may end up as a miscarriage. Some of these women with positive human Chorionic Gonadotropin test found to have an intra-uterine gestational sac on ultrasound scan without other distinct features of a viable pregnancy. Therefore such women need to be reevaluated by an ultrasound scan after some time to confirm its viability and the time duration for repeat scan may vary from 7 days to 14 days [3,4].Keeping patients in uncertain mind about their ongoing pregnancy till the follow up scan will affect them psychologically [5]. This may also lead them to seek second opinion from different health care persons or institutes, especially in the local setup. On the other hand early warning may either aggravate or improve their psychological morbidity associated with uncertainty. Following a miscarriage it will take some time for the patient to recover psychologically to carry out her normal day today activities as well as to consider about a next pregnancy [5]. Therefore it is an integral aspect of management to pay due consideration on psychological (needs) aspects of these women who were diagnosed to have a pregnancy of uncertain viability.Performing an early follow up scan also might not be very conclusive, and also will add additional strain on most health care systems, particularly so in limited resource settings. Since Sri Lanka is a low resource country, doing frequent scans may create more strain on already marginalized health resources. Performing non rational sequential ultra sound assessments are accountable for higher cost and additional burden over the health care system without any significant improvement in overall outcome. There had been not many studies carried out globally as well as locally to evaluate the ideal time period to perform a repeat scan for a patient who diagnosed to have a PUV and also to achieve consensus with regard to the number of follow up scan to be performed.There is no clear guidance as for how many ultrasound scans to be performed to determine the viability of a pregnancy. Even though some studies are carried out in other countries regarding the application of ultrasound parameters to predict the viability of an intra-uterine pregnancy, importance of such study to be performed in Sri Lanka needs to be addressed. That is because the populations among which those studies are carried out are different from Sri Lankan population in demographic aspect since they encompass different population dynamics with regard to biological, physiological, environmental factors. Such study not only will give customized parameters for the Sri Lankan women who diagnosed to have PUV, will assist in comparison with the global parameters to assess the degree of deviation or the similarity.The aim of this study is to determine a reasonable cut off values that would predict the outcome of a PUV with a reasonable degree of confidence. This will also help to achieve standard time duration for the re-evaluation of pregnancies of uncertain viability and to manage them without undue delay. Early treatment will also help to reduce physical and psychological morbidity associated with non- viable pregnancies. As Sri Lanka is a country with limited health resources, such preventive measures will save both money as well as the available resources, thus they can be utilized optimally. Ultrasound scan is the gold standard method for the diagnosis of the viability of an intrauterine pregnancy [4]. Diagnosis of the pregnancy as either viable or non-viable one is associated with subsequent set of separate management plan. According to some studies the incidence of spontaneous miscarriages even after detection of the fetal heartbeat by trans-vaginal scan can be as high as 5% to 20% [6,7]. The embryo is typically around 1–2 mm long when first detectable by ultrasound and increases in length by approximately 1 mm per day [8]. Embryonic cardiac activity has been documented in normal pregnancies at as early as 37 days of gestation [9], which is when the embryonic heart tube starts to beat [10]. Cardiac activity is often evident when the embryo measures 2 mm or more [11], but is not evident in around 5–10% of viable embryos measuring between 2 and 4 mm [12,13]. Mean Sac Diameter (MSD) is the ideal method to express the gestational sac size and MSD is the average of the three orthogonal measurements of the fluid filled space within the gestational sac [14]. Even though it has been highlighted in some studies that the growth of both gestational sac and the fetal pole has similar growth rate, some other studies counter argue this statement by quoting the existence of different growth rates between the two [8]. This may be the reason for late demonstration of viable pregnancy following initial diagnosis of PUV. Current criteria used to define PUV are not uniform. According to the latest guidelines of Royal College of Obstetricians and Gynaecologists (RCOG), presence of empty sac of a MSD of ≥ 25 mm or presence of embryonic pole without visible heart beat at ≥ 7 mm Crown Rump Length (CRL) can be categorized as a miscarriage [15] (non-viable pregnancy). According to the RCOG guidelines an empty gestational sac of ≤ 20 mm or presence of fetal pole without cardiac activity with CRL < 7 mm is defined as intrauterine PUV and suggests repeating a Transvaginal Scan (TVS) at least 7 days apart to come to a definite diagnosis with regard to the viability [3,4]. The American College of Radiologists (ACR) recommends a diagnosis of non-viable pregnancy when the CRL is 5 mm or more without cardiac activity [16] or the presence of empty gestational sac of MSD ≥ 16 mm. The Society of Gynaecologists of Canada (SOGC) suggests the non-viability of a pregnancy if MSD of ≥ 8 mm without a yolk sac or MSD of ≥ 16 mm without an embryo in TVS [17].Currently it is accepted that, for the prediction of the viability of an early pregnancy, the MSD and the CRL can be used with certain degree of confidence. But combination of sonographic parameters along with other demographic feature such as maternal age, gestational age, amount of per vaginal bleeding may have more predictive power than the sonographic parameters alone [18].Based on initial parameters and findings of subsequent follow up scans, it is possible to make a reasonable diagnosis with regard to the viability. The definitions used to make such diagnosis should be precise since the concern is about a human embryo and any error may end up with an inadvertent termination of a viable pregnancy.One study highlights that gestational sac diameter and embryonic growth are not useful in predicting the viability of a pregnancy with uncertain viability (PUV) [19]. According to this study a cut off value 0.2 mm / day was always associated with miscarriage [19]. The same study indicate that finding an empty sac more than 7 days apart is very likely to indicate a miscarriage irrespective of the growth of the gestational sac.Previously it was a common agreement that embryo and its associated structures grow at a similar rate [19], both the CRL and MSD increase by 1 mm per day. However more recent studies suggest that these speeds are variable. A smaller than expected first trimester embryo has been strongly linked with subsequent miscarriage.It has also been shown that when diagnosing a non- viable pregnancy, there is a higher inter and intra - observer variability for the measurement of MSD along with absence of the viable embryo or yolk sac thus one must take all the precautions to minimize such errors [20].
2. Objectives of the Study
- General objective:To determine the minimum ultrasound-scan cut off values to predict the subsequent viability of an intrauterine pregnancy of uncertain viability. Specific objectives:1. To determine the minimum cut off value of Crown Rump Length (CRL) in an intrauterine pregnancy of uncertain viability to predict a miscarriage2. To determine the minimum cut off value of Mean Sac Diameter (MSD) in an intrauterine pregnancy of uncertain viability to predict a miscarriage
3. Methodology
- This prospective cohort study was carried out in Castle Street Hospital for Women (Ward 7, Gynaecology Unit) and Colombo South Teaching Hospital (University Obstetrics and Gynaecology Unit). Patients who consecutively presented to the ward 7, Castle Street Hospital for Women and to University Obstetrics and Gynaecology Unit, Colombo South Teaching Hospital, Colombo, Sri Lanka who poses the inclusion criteria and consented to participate in the study were recruited in to the study.From every participant written informed consent obtained prior to recruit in to the study.A specially prepared questionnaire was given to all the participants to obtain their demographic details, obstetric history, pregnancy symptoms and socio economic data. The questionnaire was prepared in English language and the principal investigator, prior to the scans, entered the data.Indications for ultrasonography were lower abdominal pain with positive urine hCG test, bleeding per vagina with positive urine hCG test, routine early pregnancy ultrasound scan evaluation of women with positive urine hCG test as per the unit policies and for the estimation of gestational age. None of the participants were pre evaluated by performing TVS for the index pregnancy and did so will eliminate them from the study. Women categorized as having PUV were eligible for inclusion to the study unless they were clinically unstable.To minimize the inter-observer variations in obtaining the data all the ultrasound the principle investigator obtained parameters. Ultrasound scan findings were cross-validated in random basis.A pilot study was carried out to see the feasibility of the study and the validity of the questionnaire. The pilot test was also used to assess the accuracy of the sonographic data for a two weeks period. Participants of the study were underwent Transvaginal Scan (TVS) assessment to obtain the initial ultrasound parameters by using either ALOKA GmbH Prosound alpha 7 (Japan) ultrasound scan machine or Volusion E8 (GE Medical systems, Austria) ultrasound scan machine with 3.5 MHz to 11.0 MHz transducer (Multi Frequency Convex Endovaginal Probe) for B Mode imaging with pulse wave Doppler facility.All the participants were followed up weekly for 2 weeks by performing TVS and the outcome measures were documented.Depending on the outcome, during and after the follow up period, each participant was managed according to the ward protocols and guidelines thereafter.
4. Statistical Analysis
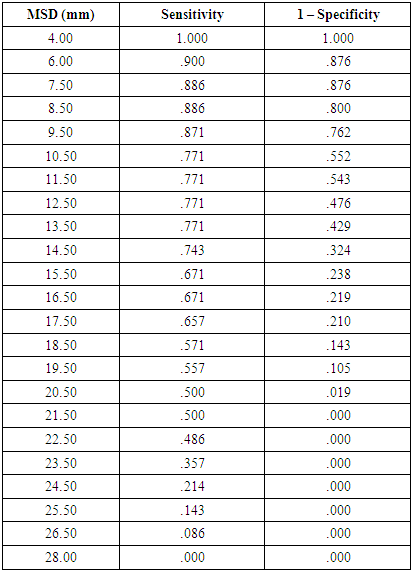
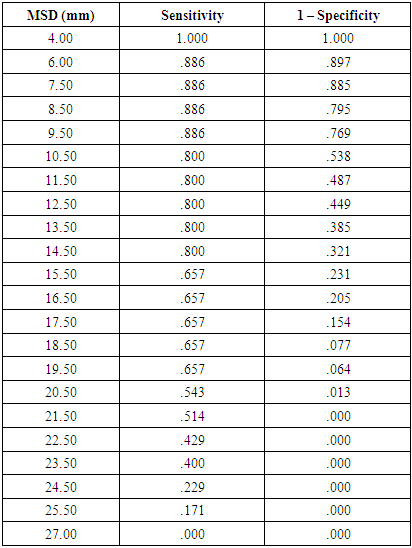
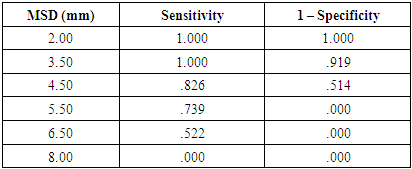
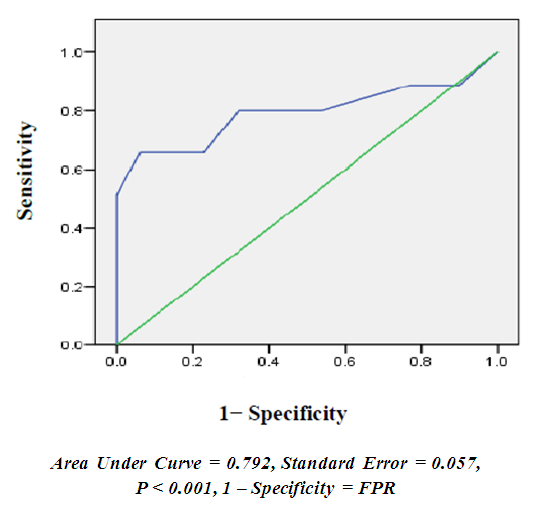
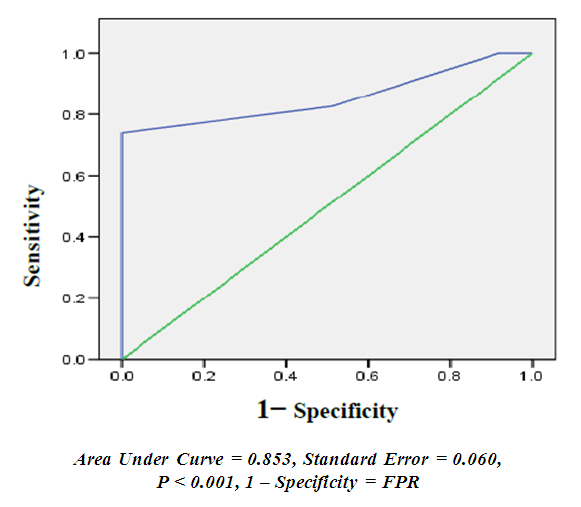
- Data was collected on to Microsoft Excel 2010 (Microsoft Corp, USA) spread sheet.Statistical analyses were performed using the Statistical Package for the Social Sciences version 15.0 (SPSS Inc., USA).The relevant descriptive statistics, frequency and percentage, were computed for categorical variables age, parity, period of gestation and blood group. Mean, standard deviation, median and 95% confidence interval were computed for quantitative variables.The chi square test was applied to compare the risk and outcome at 95% confidence interval and the p- value < 0.05 will be considered to be statistically significant.For all three groups the sensitivity, specificity, positive predictive value, negative predictive value and false positive rates (FPR) for a miscarriage were calculated by using Receiver Operating Characteristic curve (ROC curve) according to the cutoff values of 16 mm, 20 mm and 21 mm for GS with or without YS group. FPR obtained from ROC curve for 4 mm, 5 mm & 6 mm CRLs in fetal pole only group.
5. Results
- Age distribution of the participants of the study was between 17 years and 38 years (Figure 1). Among these women majority of the participants were in the age group between 26 years to 30 years.
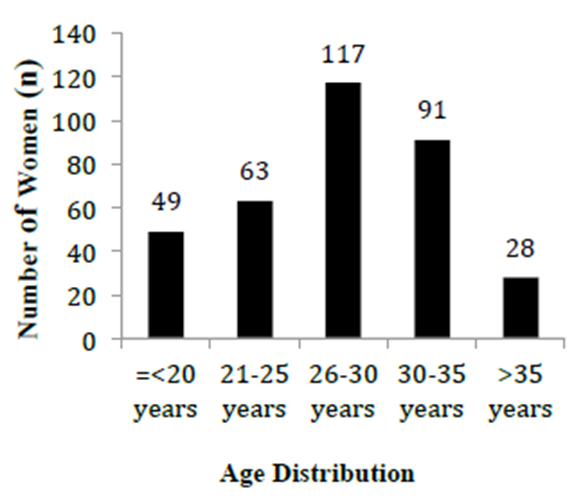 | Figure 1. Age distribution among the participants in the study |
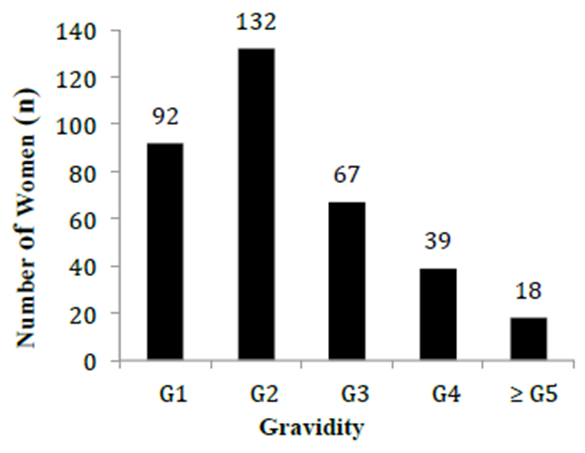 | Figure 2. Distribution of gravidity among the participants in the study |
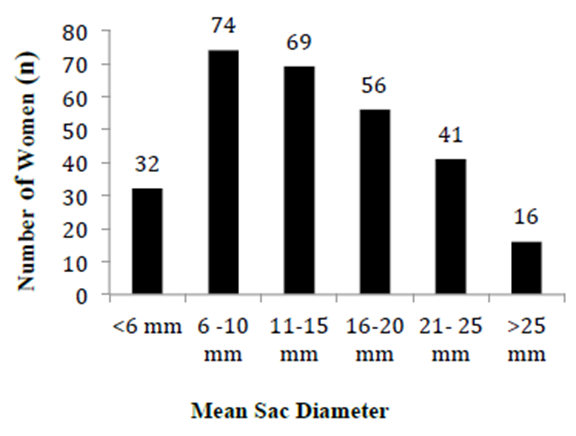 | Figure 3. Distribution of MSD among GS only and GS with yolk sac groups |
|
|
|
|
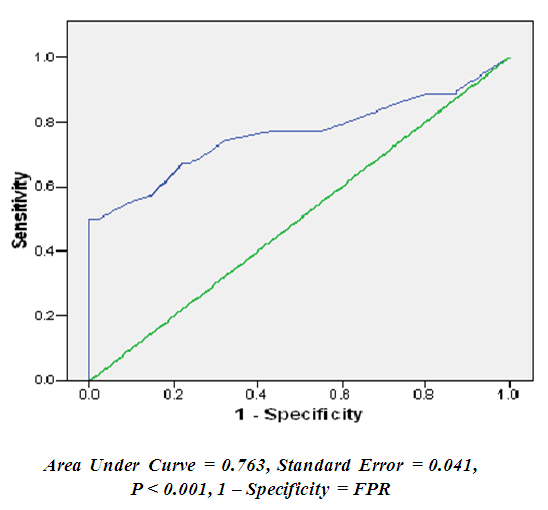 | Figure 4. ROC curve for the performance of different cut off values of MSD in GS only group for prediction on non-viability (n = 175) |
|
 | Figure 5. ROC curve for the performance of different cut off values of MSD in GS with YS only group for prediction on non-viability (n = 113) |
|
 | Figure 6. ROC curve for the performance of different cut off values of CRL in Fetal pole without cardiac activity group for prediction on non-viability (n = 60) |
|
6. Discussion
- To our knowledge this is the largest study carried out in Sri Lanka in this context and the findings of this study will be a useful tool for the reference of future studies of similar objectives and for the comparison of the global figures. The data were obtained in prospective manner where certain bias and confounding factors were safely eliminated during the process of data collection. The data collection was carried out in two different gynaecology centers where mixing of population parameters and characters has contributed to more generalization of the findings to the population.At present majority of the gynaecology units in Sri Lanka use the current RCOG recommendations in managing pregnancies of uncertain viability and miscarriages [4]. Even though some studies are carried out in other countries regarding the application of ultrasound parameters to predict the viability of an intra-uterine pregnancy, we noticed the importance of such studies to be performed in Sri Lanka. This is because the populations among which those studies were carried out are different from Sri Lankan population in demographic aspect since they encompass different population dynamics with regard to biological, physiological, environmental factors. Among the basic aims of our study we specifically looked for any influences that can exist due to the different demographic and social factors within our population when compared to the findings of global population.The aim of this study is to compare the validity of different cut off values, which has been used in different guidelines to determine the viability of pregnancy of uncertain viability. American college of Radiologists defined a miscarriage at MSD cut off of 16 mm when the empty gestational sac with or without yolk sac present at initial TVS. But this is associated with the risk of an inadvertent termination of a possibly viable pregnancy. This has been demonstrated by several studies where the MSD cut off of 16 mm at the initial TVS have subsequently develop in to live embryos [15,22]. In our study, even though we were unable to demonstrate subsequent embryonic cardiac activity for a fetal pole without initial cardiac activity above 5 mm CRL, recent evidence supports the possibility of demonstrating the subsequent viability between CRL of 5mm and 6mm [15]. Presence of different population characteristics in the participants in the study may be the reasonable justification for this observation, but other confounding factors including intra and inter observer variation in obtaining ultrasound parameters should have a higher place in the list.Ultrasound measurements of embryo detailing are subjected to significant intra and inter observer variability. For MSD measurement, the degree of variability is expected to be + / − 18.78% [20].Therefore a MSD measurement of 20 mm would be measured anywhere between 16.8 mm and 24.5 mm by two different observers. This is the same for the measurement of CRL where one observer’s measurement of 6 mm can be in between 5.4 mm and 6.7 mm for the second observer [20]. Thus it is important to be cautious in interpreting ultrasound findings in an early pregnancy to avoid any inadvertent interventions. Since we have observed subsequent viable pregnancies at the MSD measurements between 16 mm and 21 mm the above inter and intra observer variability in obtaining measurements can be explained.MSD in majority of the gestational sacs observed in the gestational sac only group is less than 15 mm at the initial scan. This may be the reason for the observation of relatively higher subsequent viable pregnancy rates in gestational sac only group when compared to other similar studies [15]. Therefore it is reasonable to state that initial size of an empty gestational sac in PUV is inversely proportionate to the subsequent viability of that pregnancy.The presence of yolk sac with the gestational sac need to be treated with extra care since it is associated with relatively higher chances of subsequent viable pregnancy rates when compared to the gestational sac only pregnancies of uncertain viability. The comparison of gestational sac only group with gestational sac with yolk sac group by using Chi squared test demonstrate positive relationship between the viability and the presence of yolk sac (p < 0.05). Even though there are some studies [24] which demonstrate the presence of yolk sac does not associate with the subsequent viability of the pregnancy, depending on the analysis of our data we would like to highlight the fact that the presence of yolk sac is relatively reassuring when compared to the presence of an empty sac alone in predicting the future viability.It has been demonstrated that when MSD cut off of 16 mm was used to define a non-viable pregnancy, there is a higher false positive rate for the miscarriage (to be misdiagnosed) when compared to 20 mm cutoff. The FPR becomes zero at 21.5 mm MSD cutoff where probability of erroneously terminating a possible viable pregnancy is non- existing. According to the finding of this study we noticed that the diagnosis of non-viable pregnancy made at the gestational sac cut off of 16 mm without yolk sac or fetal pole, there was a risk of inadvertent termination of 23 possibly viable pregnancies. This observation is same for both gestational sac only group and gestational sac with yolk sac group. Therefore it is reasonable to use the MSD of 21.5 mm as the cut off value to diagnose a non-viable pregnancy when only gestational sac with or without yolk sac detected in the initial scan. Since there is a statistically significant increase in intra and inter observer variation in measuring ultra sound scan parameters, our recommendation is to apply the current recommended cut off of 25 mm by the RCOG. At present the American College of Obstetricians and Gynaecologists (ACOG) in the management of pregnancy of uncertain viability [23] also recommend these cut off values.In our study, we were unable to demonstrate subsequent cardiac activity once the initial finding is only the fetal pole without the cardiac activity with CRL above 5 mm. This finding is further supported by the fact that the FPR at 5.5 mm CRL is being zero. But due to the same reason of inter and intra observer variation in obtaining the ultrasound scan measurements we agreed with the cut off of 7 mm which is recommended by the RCOG and ACOG for diagnosis of miscarriage. Similar findings were observed by Abdalla et al, in his study, where the cut off 25 mm for MSD and 7 mm for the CRL [15] were suggested for the diagnosis of non-viable pregnancy. It is important to highlight the fact that, the study sample in this sub group (fetal pole without cardiac activity) is comparatively lower to make any firm conclusions. But the trend of the outcome pattern obtained from this group may support the existing RCOG recommended cut off values.Expectant management for the diagnosed miscarriage is well-recognized option, which has the added benefit of delaying the medical and surgical interventions. Due to the advancements in overall facilities and readily accessibility to health care services, significant morbidity associated with the expectant management is minimal. Even though this may associate with some added element of psychological morbidity due to the uncertainty about the subsequent outcome, this option should be offered to a woman who has concerns about the viability of her pregnancy unless indicated otherwise due to other medical backgrounds.The observations obtained from our study supports the current recommendation of RCOG and ACOG guidelines in the management of pregnancies of uncertain viability. In the absence of fetal cardiac activity MSD cut off value of 25 mm and CRL cut off of 7 mm are reasonably safe margins for implementation of further management of pregnancy of uncertain viability in the context of miscarriage.
7. Conclusions and Recommendations
- In summary, this study examined the several cut off values utilized by several early pregnancy units and guideline formulating bodies in diagnosing a miscarriage following initial diagnosis of pregnancy of uncertain viability. We have notice that several cut off margins used to diagnose miscarriage by some guidelines are not safe as it might misdiagnosed a possible viable pregnancy as a miscarriage.In this study we were unable to demonstrate fetal cardiac activity during subsequent follow up scans when initial presenting MSD is above 21 mm and/or CRL of above 5 mm. This is further supported by the fact that the false positive rate for a miscarriage is being zero above these cut off values. Due to the possible intra and inter observer variability in obtaining USS parameters, our recommendation for implementation of further management in the context of a miscarriage for a PUV is when MSD cut off value of 25 mm and/or CRL cut off of 7 mm as they are reasonably safe margins.Further researches in local setup with larger sample sizes are recommended in order to improve the possible outcome to extrapolate the findings in developing local guideline in the diagnosis of miscarriage.In conclusion, 100% reliability in prediction of the viability of an intra-uterine pregnancy of uncertain viability is far beyond the reality since there can be always a possibility for the unexpected to be happened. Clinicians who are dealing with the early pregnancy management therefore should have a pre-defined validated approach to avoid any inadvertent termination of any conception, which may have the potential to be a live birth one day. At the same time, it is important to avoid any additional physical and psychological morbidity to the woman, which associated with the context of a miscarriage. Therefore the current cut off values recommended by the RCOG should be the safest approach at present in managing PUV until proven otherwise with the light of new evidence in the future.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML