Rakhimov Zokir Kayimovich
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Rakhimov Zokir Kayimovich, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The problem of etiology, pathogenesis, prevention, diagnosis and treatment of pyoinflammatory complications in fractures of the mandible remains an urgent problem today. An increase in the trend towards this topic does not reduce, which is explained in this article, a microbiological and immunological approach to the treatment of patients with fractures of the mandible and some of their results are presented.
Keywords:
Fractures of the lower jaw, Microbial adhesion, Colonization resistance of the organism, Sensitization, Dysbiosis
Cite this paper: Rakhimov Zokir Kayimovich, Microbiological and Immunological Approach to the Treatment of Patients with Mandibular Fractures, American Journal of Medicine and Medical Sciences, Vol. 11 No. 9, 2021, pp. 645-648. doi: 10.5923/j.ajmms.20211109.09.
1. Introduction
Patients with purulent-inflammatory diseases and injuries of the maxillofacial region make up from 60% to 90% of the bed capacity of specialized maxillofacial hospitals, there is a tendency to an increase in the incidence of this pathology. Despite the optimization of methods of therapy for pyoinflammatory diseases and complications of injuries to the bones of the facial skeleton; the problem of purulent infection in maxillofacial surgery continues to be relevant. The main pathogenetic link in the development of inflammatory complications in fractures of the lower jaw is a violation of local immune protection, regional blood circulation and innervation in the fracture zone, deterioration of oral hygiene and impaired chewing function.
2. Materials and Research Methods
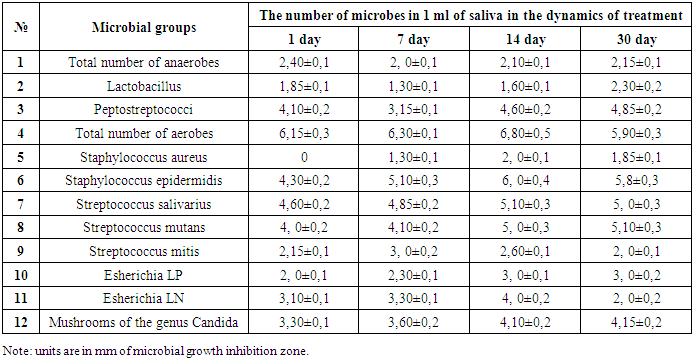
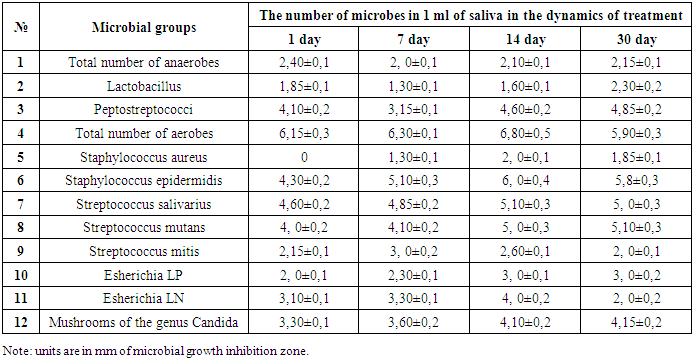
To solve this goal, we divided all the studied patients into 2 groups. At the same time, one group of patients underwent traditional therapy, while in the second group, in addition to the traditional one, special treatment was carried out.The drugs used in traditional therapy included: Furacilin, Chlorhexidine, and Bifidumbacterin. At the same time, the following drugs were used as special therapy: Cerrata, Sekstophag, Azithromycin and Florbiolact.To assess the effectiveness of the use of medicinal products, both in the traditional and in a special way, we studied the quantitative and qualitative indicators of the oral flora in the dynamics of treatment (1-7-14-30 days).Materials of microbiological studies of the oral cavity in patients with fractures of the mandible when using drugs related to traditional therapy are presented in table 1.Table 1. The state of the microflora of the oral cavity in patients with fractures of the mandible in dynamics after traditional treatment (Lg (M ± m) KOE ̸ ml)
 |
| |
|
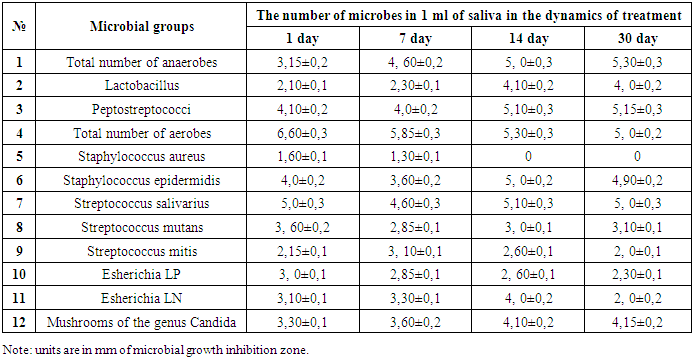
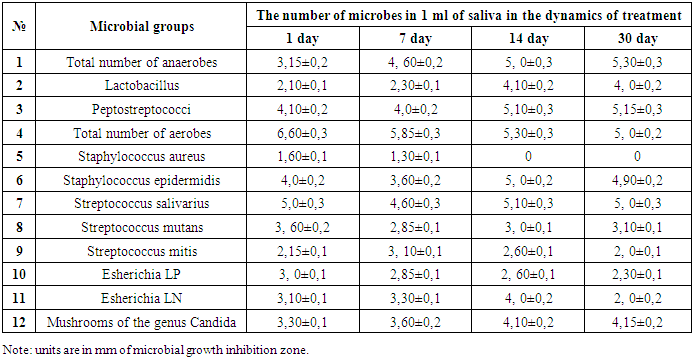
In most of the examined patients with fractures of the lower jaw, we also studied the state of colonization resistance of the most important biotopes of the oral cavity: the gum, the surface of the tongue, cheek and palate. For this, sleeves with a certain surface area were initially prepared, after sterilization they were filled with highly selective nutrient media, placed in Petri dishes and brought into the refrigerator. When examining patients, these sleeves touched the mucous membranes of the biotopes of the oral cavity for 2-3 seconds, and then these sleeves were placed back into Petri dishes, and then they were brought into a thermostat at 37° for 18-24 hours.After the indicated incubation times, the dishes were removed from the thermostat, the sleeves were removed and the grown colonies were counted, then smears were prepared from these colonies, stained according to Gram, and the morphology of the microbe was studied. After that, studying the cultural and biochemical properties, the type of microbe was determined. The number of microbes was expressed in ̸ M ± m / CFU / cm².The table shows that on the next day after traditional therapy in the oral cavity in patients with fractures of the mandible, dysbiotic shifts were noted throughout the studied group of microbes.Analysis of the state of the oral flora in patients on the 7th day after treatment shows that the dysbiotic changes that took place in the oral cavity on the first day, not only did not improve, but, on the contrary, deepened even more.Although, it should be noted that some positive changes were noted in the quantitative parameters of streptococci. At the same time, it should be noted that pathogenic strains of staphylococci (St. aureus) began to be seeded in the oral cavity.Microbiological studies on the 14th day after traditional treatment show that positive changes have appeared in all parameters of the oral flora, especially they concern the anaerobic flora and cocci. Although it should be noted that, on the contrary, a negative picture is observed for gram-negative flora, that is, the sowing rate has increased.At the same time, the analysis of microbiological studies of the oral cavity on the 30th day convinces us that the positive changes noted on the 14th day are fully preserved, and according to some indicators, especially this concerns lactobacilli, they are even more positive. Although it should be noted that we have a negative picture of the sowing rate of fungi of the genus Candida.Apparently, the medicinal preparations used by us lack antifungicidal properties.The next group of our studies consisted of patients with fractures of the mandible, in which, along with traditional therapy, special treatment was carried out. The materials of these studies are presented in Table 2, the table shows that already on the 7th day in the oral cavity in patients there are positive changes in all the studied flora. It should be noted that pathogenic strains (St. aureus) of staphylococci began to be sown in this group of patients on the 7th day. The analysis of microbiological studies in the same patients on the 14th day indicates that the positive changes that were noted on the 7th day not only remained, but improved even more.Table 2. Characteristics of the microflora of the oral cavity in patients with fractures of the mandible in dynamics with special treatment (Lg (M ± m) KOE ̸ ml)
 |
| |
|
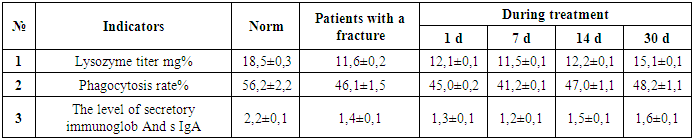
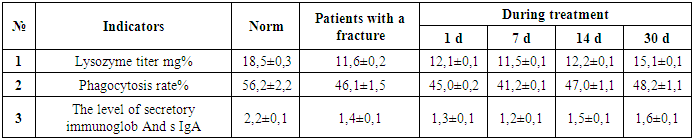
In these same patients who received special treatment on the 21st day, the picture of dysbiosis was virtually eliminated in all respects. It is gratifying to note that these positive changes in patients with fractures of the mandible in the oral cavity were also noted in relation to pathogenic strains of staphylococci and Candida fungi.It is interesting to note that in the same patients after special treatment on the 30th day, it is noted that the positive shifts in the flora of the oral cavity that took place on the 21st day were not only preserved, but deepened even more. Apparently, these positive changes occurred due to the use of general and local eubiotics.In all examined patients with fractures of the lower jaw, in parallel with microbiological studies, we also studied the state of local factors of protection of the oral cavity. Materials of these studies are presented in table 3,4, which are also studied in the dynamics of traditional and special treatment.As can be seen from table 3 after traditional treatment, there is an immunodeficiency in all studied parameters. In this case, the immunodeficiency is reliably expressed on the 1st and 7th days after treatment. Starting from the 14th day of traditional treatment and especially on the 30th day, there is a significant improvement in the picture. However, there is no need to talk about a complete recovery of immunodeficiency indicators.Table 3. Indices of local factors of protection of the oral cavity in patients with fractures of the mandible in the dynamics of traditional treatment
 |
| |
|
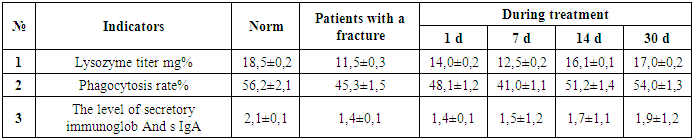
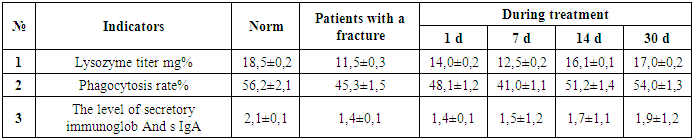
Table 4 shows the indices of local factors of protection of the oral cavity in patients with fractures of the mandible in the dynamics of special treatment. The table shows that the immunodeficiency is most reliably expressed in terms of 1 and 7 days. However, starting from 14 days, there is a significant improvement in the picture of immunodeficiency in all indicators. At the same time, in the same patients on the 30th day of special treatment, in fact, all indicators of local factors of protection of the oral cavity are close to the control figures.Table 4. The state of local factors of protection in patients with fractures of the mandible with special treatment in dynamics
 |
| |
|
3. Results and Discussion
It is interesting to note that dynamic changes in the state of indices of local factors of protection of the oral cavity in patients with fractures of the mandible have a direct correlation with changes in dysbiosis in the oral cavity both after traditional and after special treatment. | Picture 1. Healthy |
 | Picture 2. Sick |
The state of local factors of protection of the oral cavity in patients with fractures of the mandibleThe most interesting data obtained by us in the study of the colonization resistance of microbes in the biotopes of the oral cavity such as the gum, surface of the tongue, cheek and palate in patients with fractures of the mandible.According to our research, it has been established that the density of the microbial population in the oral cavity in healthy people is a fundamental characteristic of the community and largely depends on the topography of the ecological niche. At the same time, the highest value was noted in the gums (4.20 ± 0.3 CFU cm2), the minimum on the mucous membranes of the palate (1.25 ± 0.1 CFU cm2).At the same time, Gram-positive flora, which colonized 100% of the subjects, was predominant in terms of the number and species composition in the biocenosis, it is interesting to note that the main part of the oral microflora in healthy individuals was made up of representatives of the genus streptococci, while the dominant species was Str. salivarius. It is quite obvious that the study of the ability of microbes to colonize various biotopes in the oral cavity makes it possible to understand those intimate processes that occur in the oral cavity, which are apparently undoubtedly associated with the state of the oral cavity liquids, as well as from the presence of special receptors in our cells on which microbes can specifically adhere.
4. Conclusions
Thus, based on the data obtained on the study of the state of the flora, local protective factors and the ability of microbes to colonize in the oral cavity in patients with fractures of the mandible, the following conclusions can be drawn: However, the use of traditional therapy in such patients does not allow to completely eliminate dysbiosis even on the 30th day. 2. At the same time, in patients with fractures of the lower jaw during a special course of treatment, already on day 21, it makes it possible to almost completely restore dysbiosis to the control table 3. It is interesting to note that the information obtained after both traditional and special treatment has a direct correlation with changes in dysbiosis, immunodeficiency and colonization resistance. These data once again testify to the unity of our body in homeostasis.
References
| [1] | Agarkov N.M., Gontarev S.N., Zelensky V.A., Domenyuk D.A., Makkonen K.F., Afanasova E.P., Ivanov A.V., Subbotina T.I. Mathematical prediction of the development of phlegmon in acute odontogenic osteomyelitis of the jaw in terms of blood and systemic immunity / Medical Bulletin of the North Caucasus, 2018; 1: 62-65. |
| [2] | Belovolova R.A., Novosyadlaya N.V., Novgorodsky S.V. Features of the immune status and the possibility of immunocorrection in post-traumatic inflammatory complications in patients with open fractures of the lower jaw // Immunology, 2002; 5S: 287-293. |
| [3] | Ivanushko T. P., Gankovskaya L. V., Shamanaev S. V., Svich O. A., Kartashov D. D., Grechenko V. V., Balykin R. A. Study of the content of defensins in patients with purulent -inflammatory diseases of the maxillofacial region // Dentistry, 2014; 93: 2. - S. 23-26. |
| [4] | Matrosov V. I. EHF-therapy in the complex treatment of acute purulent-inflammatory diseases of the maxillofacial region // dissertation for the degree of candidate of medical sciences / Vladivostok State Medical University. Vladivostok, 2002. |
| [5] | Nikitin A.A., Lapshin V.P., Kosyakov M.N., Stuchilov V.A., Malychenko N.V. Modern methods of diagnosis and treatment of odontogenic mediastinitis / Russian otorhinolaryngology, 2004; 5: 15-18. |
| [6] | Robustova T.G. New trends during odontogenic osteomyelitis of the jaw / Russian Dental Journal, 2006; 5: 32-34. |
| [7] | Rakhimov Z.K. “Purulent - inflammatory complications of fractures of the lower jaw” monograph, 2019. |
| [8] | Zokir K. Rakhimov Characterization of the sensitivity of microbes to certain drugs in vitro!, Journal of Natural Remedies Vol. 22, No. 1(1), (2021) 123-127. |
| [9] | Olawale O. Adamson, Olalekan M. Gbotolorun, Olalekan Odeniyi, Oyinlola O. Oduyebo, Wasiu L. Adeyemo. Assessment of predictors of treatment outcome among patients with bacterial odontogenic infection / Saudi Dent J., Oct., 2018; 30(4): 337–341. |
| [10] | Rishi Kumar Bali, Parveen Sharma, Shivani Gaba, Avneet Kaur, Priya Ghanghas. A review of complications of odontogenic infections / Natl J Maxillofac Surg, Jul-Dec., 2015; 6(2): 136–143. |
| [11] | “Changes in the dynamics of transmission of the disease by the causative agents of osteomyelitis” Nuraliev N.A., Ergashev V.A. “Journal of Theoretical and Clinical Medicine” Tashkent, 2018; 2: 68-71. |
| [12] | Sagdullayeva G.U., Nazarov J.-S.E., Suleymanov S.F., Olimova N.I. “Comparative analysis of the immune system at often and rarely ill children depending on the stage of disease” // Academicia, December, 2019; 12: 22-25. ISSN: 2249 -7137: 9 DOI Number: 10.5958 / 2249-7137.2019.00118.6. |
| [13] | Malakhov A.B., Kolosova N.G., Khabibulina E.V. Bacterial lysates in programs for the prevention of respiratory infections in children // Practical Pulmonology, 2015; 4: 16-19. |
| [14] | Del-Rio-Navarro BE, Espinosa Rosales F., Flenady V., SienraMonge JJL Immunostimulants for preventing respiratory tract infection in children // Cochrane Database Syst. Rev., 2996; 4: CD004974. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML