-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(9): 618-622
doi:10.5923/j.ajmms.20211109.03
Received: Jul. 10, 2021; Accepted: Aug. 25, 2021; Published: Sep. 15, 2021

Rehabilitation Potential of Children with Traumatic Brain Disease
Rakhimbaeva G. S., Khamraev N. R.
Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Rakhimbaeva G. S., Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article provides data on clinical, neurological and instrumental data from the examination of children with traumatic brain disease, the data obtained give an objective idea of the rehabilitation potential and allow predicting the outcome of rehabilitation measures, differentiated approach to planning and providing rehabilitation assistance.
Keywords: Brain injury, Rehabilitation, Brain disease, Treatment, Cognitive disorders
Cite this paper: Rakhimbaeva G. S., Khamraev N. R., Rehabilitation Potential of Children with Traumatic Brain Disease, American Journal of Medicine and Medical Sciences, Vol. 11 No. 9, 2021, pp. 618-622. doi: 10.5923/j.ajmms.20211109.03.
Article Outline
1. Relevance
- Traumatic brain injury (TBI) is one of the most serious problems of modern medicine, the relevance of which is beyond doubt. Thus, injuries to the skull and brain account for more than a third of all injuries, which, according to WHO, annually increase by at least 2%. The average incidence rate for TBI was 95 per 100 thousand of the population, the mortality rate reached 22%. Most often, TBI occurred in adolescents and people over 75 years old. The most common cause is car accidents and catatrauma. When studying the epidemiology of TBI in various countries, it was revealed that 69 million people in the world receive TBI annually. Mortality as a result of TBI is very high - more than 2.5 million people worldwide, which is 48 deaths per 100 thousand people per year [3,9,10]. An important problem in pediatrics, unfortunately, far from being resolved at the present time, is the objectification of the assessment of restorative treatment. To assess the effectiveness of restorative treatment, control methods used to assess the treatment of an acute episode of the disease (according to the subsidence of clinical symptoms, changes in laboratory parameters, dynamics of radiological data, etc.) are not applicable. The system for evaluating the effectiveness of rehabilitation treatment and rehabilitation of children with TBI should use criteria that monitor the level of health during recovery. In particular, physical, mental and social parameters are subject to monitoring, as well as integral changes in the state of the body with the choice of optimal diagnostic parameters [8].An integral parameter characterizing the level of health and the patient's ability to recover and improve health in the process of recovery can be a complex indicator characterizing the rehabilitation potential (RP) of a child [6].Rehabilitation potential is a scientifically substantiated limit of the possible restoration of deficient (impaired) physiological functions in a specific clinical case, and a rehabilitation prognosis is a medically justified probability of achieving the intended rehabilitation goals in a planned period of time, taking into account the nature of the disease, its course, individual resources and compensatory capabilities. [4]. However, the question of the content and criteria for assessing RP is still controversial and insufficiently developed, in addition, this concept is more often used in scientific literature and does not find proper application in practical medicine [5]. This can be associated both with the ambiguity of the definition of the concept of RP by different authors, and with the complexity of developing criteria for its assessment in certain nosologically forms in connection with the versatility of the concept [7]. One of the definitions of the rehabilitation potential interprets this indicator as a complex of biological and psychophysical characteristics of a person, as well as social and environmental factors that allow, to one degree or another, to realize his potential abilities [1]. As follows from the above definition, RP is a systemic biopsychosocial characteristic of a person's status. The content of this characteristic indicates the objective possibilities of rehabilitation: the nature of the disease, its features, psychophysiological state of the patient, his socio-economic situation and subjective: the patient's attitude, structure of needs, range of interests, and so on. Moreover, RP is an integral characteristic of an individual's status; the allocated components of RP are interconnected, affect each other and have, in this context, significance for all aspects of restorative treatment. A qualitative analysis of the RP allows one to determine the goals and objectives of the rehabilitation of a particular individual, to establish a hierarchy of priorities for these tasks, to substantiate and develop optimal and adequate rehabilitation measures [5].
2. Objective of the Study
- To assess the rehabilitation potential and quality of life of children with traumatic brain diseases.
3. Materials and Research Methods
- To achieve the research goal and solve the set tasks, we examined 150 children, 120 (main group) of whom were hospitalized at the Republican Research Center of Neurosurgery from 2017 to 2019 with TBI. As a control group for a comparative analysis of the quality of life and social adaptation, 30 apparently healthy children were examined, corresponding to the gender-age criteria of the main group. The age of the children ranged from 3 to 18 years old. The number of patients 3-7 years old in our study correlated with patients 7-14 and 14-18 years old as 1: 2, and patients 7-14 and 14-18 years old were represented by an equal number. by gender, the ratio of boys to girls was almost 2:1. At the beginning of the study, patients with TBI were examined according to a single scheme: examined by a pediatric resuscitator, neurosurgeon, surgeon, traumatologist, X-ray examination of the skull, neck, chest, abdomen, pelvis and, if necessary, extremities was performed. The abdominal and thoracic cavities were examined using an ultrasound method. Hemoglobin, hematocrit, sugar, urea, creatinine, blood bilirubin, the state of acid-base balance were urgently investigated. Bone traumatic injuries outside the skull, as well as traumatic injuries of the chest and abdominal organs were not found in the patients participating in the study. In dynamics, the usual laboratory parameters of blood and urine were monitored, the gas composition of the blood was studied, and a dynamic study of the composition of the cerebrospinal fluid was carried out.It should be clarified that our study did not include patients who died in any period of TBI. We studied the mechanism of injury, the timing of hospitalization, the timing of surgical interventions, clinical and neurological manifestations in isolated and concomitant injuries, the structure and clinical picture of complications, the outcomes of surgical and conservative treatment, rehabilitation potential and quality of life, and rehabilitation programs were prescribed in accordance with rehabilitation forecasts. For each patient, we filled out a specially developed medical registration card, including passport data of the child and parents, data of instrumental and clinical research methods. The passport part, which serves to identify patients, displayed the full name, date of birth, exact age (in years and months) and gender of the patient, as well as the number of his inpatient's medical record and length of hospital stay.Closed head injury occurred in 76 patients (63.33%), open non-penetrating head injury - in 41 patients (34.17%), open penetrating head injury - in 3 patients (2.5%). Aims and fulfillment of the assigned tasks, we have developed criteria for the inclusion and exclusion of patients from the study.The inclusion criteria for the study were:• presence of TBI;• the level of consciousness according to the Glasgow Coma Scale 8 or less points;• absence of severe concomitant chronic diseases (clinically pronounced circulatory insufficiency, severe decompensated diabetes mellitus, neurological, hematological diseases);• the absence of conditions limiting the use of the methods of treatment used in the work.The exclusion criteria from the study were:• the presence of oncological, inflammatory and focal neurodegenerative lesions of the brain;• the presence of a neurological deficit due to the decompensation of somatic diseases.The severity of TBI was determined by the classification of TBI severity edited by Professor B.V. Gaidar. from 2002 [2].The degree of impairment of consciousness in the patients participating in the study was assessed using the Glasgow Coma Scale (GCS) in the modification of the Glasgow Coma Scale, Adelaide Coma Scale, and Pediatric Coma Scale. Coma level on the Glasgow scale varied in points: 15 - clear consciousness; 13-14 - stun; 9-12 - stupor; 4-8 - coma; (8 - mild, 7-6 - medium, 4-6 - severe); 3 - brain death. Outcomes of brain damage were assessed using the Glasgow Outcome Scale (GOS). According to the Glasgow Outcome Scale, there are unfavorable outcomes - types 1 and 2, and favorable outcomes - types 3, 4 and 5.The Pediatric Cerebral Performance Category Scale (PCPC) was used to determine delayed outcomes. The scale implies the restoration of brain functions from normal to brain death with a greater focus on the child's social sphere of activity and dependence on others, with 1 point being the norm, and 6 being brain death.To study long-term outcomes, the Pediatric Overall Performance Category Scale (POPC) was used. The scale implies the restoration of functions from normal to brain death with a focus on the social sphere of the child's activity in accordance with the age and the norm of activity, with 1 point being the norm, and 6 being brain death. The visual assessment determined the belonging of the EEG to one of five types according to the classification of E.A. Zhirmunskaya, adapted to childhood. The characteristics of EEG types according to this classification are presented in Table 2.2. Types 2 and 5 are not normally found and are considered pathological.To study the quality of life, we applied the international children's questionnaire of the quality of life Pediatric Quality of Life Inventory - PedsQL ™ 4.0. The questionnaire consists of 23 questions, which are combined into the following scales: physical functioning (FF) - 8 questions, emotional functioning (EF) - 5 questions, social functioning (SF) - 5 questions, role functioning - functioning in kindergarten (FDS ) or school functioning (SHF) - 3 or 5 questions (depending on the age of the children).The data obtained were subjected to statistical processing on a personal computer using programs developed in the EXCEL-2016 package using a library of statistical functions.
4. Research Results
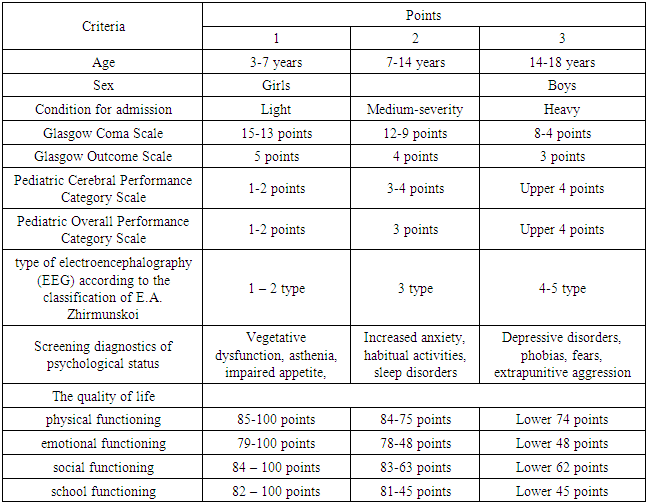
- Rehabilitation potential has 4 levels of assessment:A high rehabilitation potential presupposes the possibility of achieving full recovery of health, all types of activities usual for a disabled person, including the ability to work, and social status (complete rehabilitation).Medium is observed with incomplete recovery with residual manifestations in the form of severe dysfunctions. The performance of the main types of activity is possible in a limited amount or with the help of technical (TCP) or other means of rehabilitation, partial restoration of working capacity is noted, while maintaining a partial decrease in the level and quality of life, the need for social assistance and protection. Low is observed with a slowly progressive course of the disease, severe dysfunction, significant restrictions on life, including the ability to work, the need for constant social assistance and protection. The lack of rehabilitation potential is observed with a progressive course of the disease, a pronounced dysfunction of organs and systems, the inability to compensate for disabilities, the presence of persistent partial or complete disability, the need for constant outside care or supervision, the need for constant social assistance and protection (rehabilitation is impossible - stable disability or its aggravation). For the examined children with TBI, clinical, psychological, and social factors are identified that are reliably associated with the parameters of the quality of life. Physical functioning was influenced by the degree of dysfunction (CC = -0.45), the degree of disability (CC = -0.51), well-being (CC = +0.52), the severity of neurological disorders (CC = +0.50), in turn, it determined the psychological status (CC = +0.49). Role functioning, conditioned by the physical state, was associated with extraversion (CC = +0.49), the level of neuroticism (CC = -0.42), activity (CC = +0.34), relationships with peers (CC = +0, 41). The severity of neurological and psychological disorders significantly depended on the child's age and sex (CC = +0.38 and +0.45), the degree of the main dysfunction (CC = +0.22), influenced the state of health (CC = +0.26).Vital activity turned out to be significantly associated with the presence of concomitant disorders (CC = +0.47), gender of the child (CC = +0.63), extraversion (CC = +0.46), level of neuroticism (CC = -0.36), state of health (CC = +0.38), mood (CC = +0.52), school performance (CC = +0.46). Social functioning depended on the degree of limitation of life activity (CC = +0.34), the level of neuroticism (CC = -0.46), gender and age of the child (CC = +0.38 and +0.41).Role functioning, conditioned by the emotional state, was significantly associated with extraversion (CC = +0.31), the level of neuroticism (CC = -0.53), motivation for success (CC = +0.37), well-being (CC = +0 , 47), activity (CC = 0.40), relationships with peers (CC = +0.52), with the severity of the disease (CC = +0.42). Correlations of mental health and extraversion (CC = +0.32), level of neuroticism (CC = -0.41), well-being (CC = +0.35), activity (CC = +0.35), mood (CC = +0.39), school performance (CC = +0.41), relationships with peers (CC = +0.40). When determining the possible range of risk values for a complex of factors taken, the range from minimum values to maximum values was determined - 13 ÷ 39. It follows that the higher the score as a result of the influence of the complex of the studied factors, the higher the likelihood of the development of a low rehabilitation potential in a child with a brain injury and the more grounds for allocating him to the group of an unfavorable rehabilitation prognosis. Based on statistically significant characteristics, a point assessment of the rehabilitation potential was developed (Table 4.1).
|
5. Conclusions
- 1. An objective quantitative assessment of the rehabilitation potential of a child with traumatic brain disease in the dynamics of rehabilitation treatment allows individualizing the plan of rehabilitation measures, determining the main controllable points of influence, assessing the effectiveness and possible reasons for the insufficient effectiveness of the patient's rehabilitation treatment.2. A differentiated approach to the diagnosis and treatment of cognitive disorders contributes to an increase in the effectiveness of complex rehabilitation and social adaptation in children with the consequences of traumatic brain injury.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML