Ismailov S. I., Devyatov A. V., Babadjanov A. Kh., Tuksanov A. I., Baybekov R. R.
Republican Specialized Scientific and Practical Medical Center for Surgery named after Academician V.Vakhidov, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
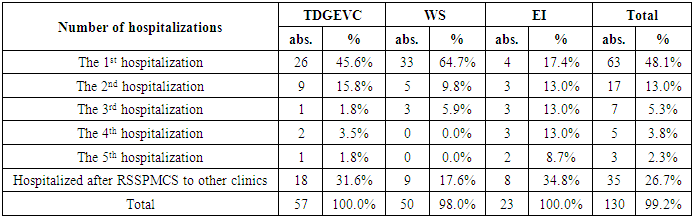
Aim of the study was to evaluate in a comparative aspect the efficiency of various methods of preventing hemorrhagic syndrome in patients with extrahepatic portal hypertension. Material and methods. The study included 131 patients with various forms of extrahepatic portal hypertension, who underwent surgical prevention of recurrent bleeding from varices in the Republican Specialized Scientific and Practical Medical Center for Surgery named after academician V.Vakhidov for the period from 2006 to 2020. The majority of patients were at adolescence (41,2%) and young (45,0%) ages. Total dissociation of the gastro-esophageal collector was performed in 57 (43.5%) patients, portosystemic bypass surgery – in 51 (38.9%) patients and endoscopic interventions – in 23 (17.6%) cases. Results. In 48.1% of cases, a good result was obtained in one stage of treatment, in 16.8% patients additional sessions of endoscopic interventions were required. The best results were obtained with portosystemic bypass surgery. In general, the proportion of successful treatment was 82.4%. The comparative frequency of recurrent bleeding showed a significantly low efficiency of endoscopic interventions, in which repeated episodes of hemorrhagic syndrome were developed in 65.2% of patients after an average of 13.5±2.9 months. The total dissociation of the gastroesophageal collector provided a relapse-free course lasting 25.9±4.4 months (p<0.05) in 35.1% of cases (p=0.014). Conclusion. The efficiency of the methods used to prevent bleeding from varicose veins of the esophagus and stomach in extrahepatic portal hypertension at one stage of treatment made up only 48.1%. At the same time, the most difficult categories were portal system thrombosis and splenoportal thrombosis with good results of single-stage or combined surgical approaches in 60% of cases. At the cavernous transformation of the portal vein this indicator was 65.0%, isolated thrombosis of the splenic vein - 71.4% and portal vein thrombosis - 73.5%.
Keywords:
Extrahepatic portal hypertension, Variceal bleeding, Surgical treatment, Results, Immediate and long-term complications
Cite this paper: Ismailov S. I., Devyatov A. V., Babadjanov A. Kh., Tuksanov A. I., Baybekov R. R., Surgical Treatment Results of Extrahepatic Portal Hypertension, American Journal of Medicine and Medical Sciences, Vol. 11 No. 8, 2021, pp. 583-589. doi: 10.5923/j.ajmms.20211108.08.
1. Introduction
The extrahepatic form of portal hypertension (EPH) is a syndrome of portal hypertension (PH) which is not associated with cirrhotic or oncological lesion of the hepatic parenchyma, while including a fairly wide range of diseases of various etiologies and pathogenesis affecting the hepatic vascular system at various levels: from the microcirculatory bed to the main vessels [1-3]. Causal factors that can lead to portal vein thrombosis (PVT) are various pathological conditions. The direct etiology of EPH includes extrahepatic obstruction (thrombosis) of the portal vein (PV), portal fibrosis of non-cirrhotic genesis (the so-called idiopathic PH), nodular regenerative hyperplasia, partial nodular transformation, congenital portal liver fibrosis, schistosomiasis, liver peliosis, etc. [2,4-5]. Up to 30% of PVT is due to extrahepatic thrombosis [5-6]. According to the literature, PVT is the cause of bleeding from the esophageal varices (EV) in 25-30% of cases and in children up to 68-84% of cases [6-7]. The understanding of the etiopathogenesis of portal vein obstruction has significantly expanded which has led to a significant improvement in treatment results, thanks to the selection of patients and, accordingly, to the choice of the most optimal method for correcting EPH for recent years. In clinical practice, the choice of an operative aid for EPH is decided on the basis of the patency of the splenoportal bed, which determines the tactics of surgical intervention as a radical way to correct PH (reducing portal pressure due to one of the variants of Warren shunt (WS), conditionally-radical (dissociation of the asigo-portal venous collector) or paliative (a variant of temporary endoscopic intervention by ligation or EV sclerotherapy in acute bleeding or its threat). [3,5,7].The immediate and long-term results of various EPH correction options were analyzed and evaluated in the article.Aim of the study was to evaluate in a comparative aspect the efficiency of various methods of preventing hemorrhagic syndrome in patients with extrahepatic portal hypertension.
2. Material and Methods
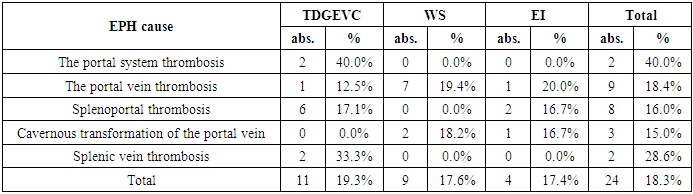
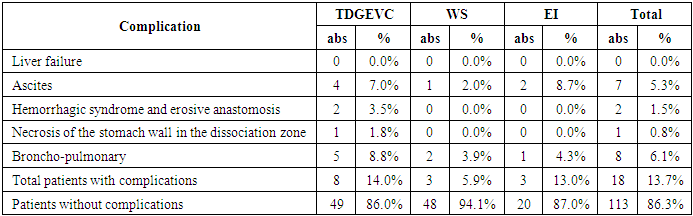
The study included 131 patients with various forms of EPH who underwent various options for surgical prevention of recurrent bleeding from EV in RSSPMCS named after academic V. Vakhidov for the period from 2006 to 2020. Male patients were 58.0%, while female patients were 42.0%, respectively. The majority of patients were at adolescence (41,2%) and young (45,0%) ages. Patients of mature and elderly age made up a total of only 13.7%.Anamnesis collection showed that acquired thrombophilia occurred in 4 (3.0%) young patients who had a confirmed hematological status - an elevated level of clotting factor VIII; hereditary thrombophilia associated with a mutation of the methylenetetrahydrofolate reductase gene and antithrombin deficiency was observed in two (1.5%) and one (0.76%) cases, respectively. The development of EPH associated with the pathological course of pregnancy was noted in 3 (2.3%) patients and in 5 (3.8%) patients was associated with prolonged use of contraceptive drugs and changes in the hormonal background of the body. The largest number of adolescent (42 / 32.0%) and young (31 / 23.6%) patients with a history of EPH had previous umbilical sepsis associated in most cases with exchange transfusions in the neonatal period and improper processing of the umbilical cord.In 5 (3.8%) patients with EPH, concomitant Crohn's disease (3/2.3%) and ulcerative colitis (2/1. 5%), which could cause EPH, were noted. Two patients (1.5%) were undergoing specific treatment due to tuberculosis mesadenitis for a long time. In 19 (14.5%) patients EPH was interpreted against the background of idiopathic liver fibrosis and in the remaining cases (10/7. 6%) as a cryptogenic etiology.Isolated "portal vein thrombosis" and "splenoportal thrombosis" were diagnosed in 49 and 50 (38.1%) patients, respectively. "Portal system thrombosis" and isolated "splenic vein thrombosis" were observed in only 5 (3.8%) and 7 (5.3%) cases, respectively. There was a "cavernous transformation of the portal vein" in other cases. There were 24 patients with total EV (18.3%), the spread of the process in the area of gastric cardia was noted in 94 (71.8%) patients. At the same time, patients with the maximum expansion of venous veins mainly prevailed. The most common complaints during the planned hospitalization of patients with EPH to the hospital were: general weakness, pain and heaviness in the left hypochondrium, nosebleeds. According to ultrasound data, an enlarged spleen was determined in 119 (90.8%) patients. All patients were hospitalized to RSSPMCS named after academic V. Vakhidov for surgical treatment. The distribution of patients by the nature of surgical intervention showed that total dissociation of the gastro-esophageal venous collector (TDGEVC) was performed in 57 (43.5%) patients, portosystemic bypass surgery (PBS) – in 51 (38.9%) patients and endoscopic interventions (EI) – in 23 (17.6%). At the same time, only TDGEVC (5/3. 8%) was performed in patients with "portal system thrombosis". The largest number of WS was performed in patients with "portal vein thrombosis" and its "cavernous transformation" - 36 (27.5%) and 11 (8.4%), respectively. In contrast, with splenoportal thrombosis, 35 (26.7%) patients underwent TDGEVC and only 3 (2.3%) patients underwent WS.Endoscopic interventions were performed as an independent aid in 23 (17.6%) cases, in the absence of indications for one of the types of open interventions in 18 (13.7%) and when the patient refused surgery - in 5 (3.8%) cases. EI by sclerotherapy methods of EV was performed in 7 patients and by ligation - in 16 patients.The variants of WS were: the applying of a distal splenorenal anastomosis (DSRA), performed in 16 (12.2%) patients; splenosuprarenal anastomosis (SSRA) - in 14 (10.7%) cases; laterolateral splenorenal anastomosis (LLSRA) - in 5 (3.8%) patients; H-shaped mesenteric-caval anastomosis (H-MCA) - in 7 (5.3%); H-shaped mesentericorenal anastomosis (H-MRA) - in 3 (2.3%); proximal splenorenal anastomosis – PSRA) - in 2 (1.5%); H-shaped splenorenal anastomosis – H-SRA-in 4 (3.1%) patients. The largest (11/8. 4%) amount of DSRA was performed for portal vein thrombosis.The research materials were subjected to statistical processing using parametric and nonparametric analysis methods in Microsoft Office Excel 2016 spreadsheets and using the STATISTICA 13.3 program (developed by StatSoft. Inc).Quantitative indicators were evaluated for compliance with the normal distribution (Kolmogorov-Smirnov criterion). When comparing the average values in normally distributed sets of quantitative data, the Student's t-test was calculated. The obtained values of the Student's t-test were evaluated by comparison with the critical values. The differences in the indicators were considered statistically significant at a significance level of p<0.05.The comparison of nominal data was carried out using the Pearson criterion χ2 allowing to assess the significance of differences between the actual number of outcomes or qualitative characteristics of the sample falling into each category, and the theoretical number that can be expected in the studied groups if the null hypothesis is valid.
3. Results and Discussion
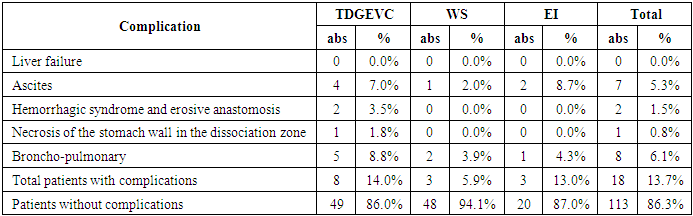
Table 1 shows the distribution of patients with EPH by the frequency of immediate complications after various interventions, which shows that in almost all cases there was no development of liver failure which is the main complication in patients with liver cirrhosis (LC). However, the development of edematous ascitic syndrome was noted in 4 (7.0%) patients after TDGEVC, in 1 (2.0%) patient after WS and in 2 (8.7%) after EI. Such specific complications as anastomositis (2 (3.5%)) and necrosis of the stomach wall (1 (1.8%)) were typical for TDGEVC. Bronchopulmonary complications were observed among patients in all the compared groups. There were 18 (13.7%) patients with a complicated course of the immediate postoperative period, and the absence of complications was noted in 113 (86.3%) patients (Tab. 1).Table 1. Distribution of patients with EPH by the frequency of immediate complications after various interventions
 |
| |
|
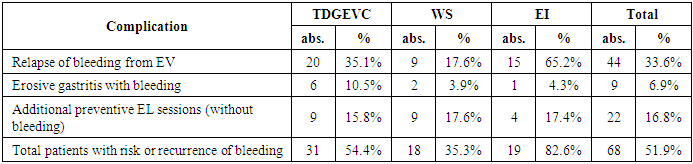
The main complication in the long-term period was gastroesophageal bleeding from EV or due to the development of hemorrhagic gastritis (Tab. 2).Table 2. Distribution of patients with EPH by the frequency of long-term complications or the need for additional stages for the prevention of recurrent bleeding from EV
 |
| |
|
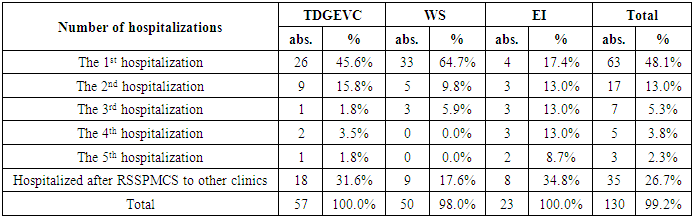
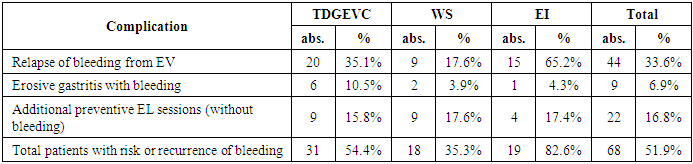
Thus, when distributing patients with EPH by the frequency of long-term complications or the need for additional stages for the prevention of recurrent bleeding from EV, which is presented in Table 2, it was noted that a recurrence of bleeding from EV was observed in 20 (35.1%) patients after TDGEVC, in 9 (17.6%) patients after WS and in 15 (65.2%) patients after EI. Erosive-hemorrhagic gastritis was observed in 6 (10.5%) patients after TDGEVC, in 2(3.9%) patients after WS and in 1 (4.3%) patient after EI. At the same time, the largest number of repeated hospitalizations (54.4%) was noted after TDGEVC (the distribution of patients by the number of inpatient treatment courses is shown in Table 3).Table 3. Distribution of patients by the number of inpatient treatment courses
 |
| |
|
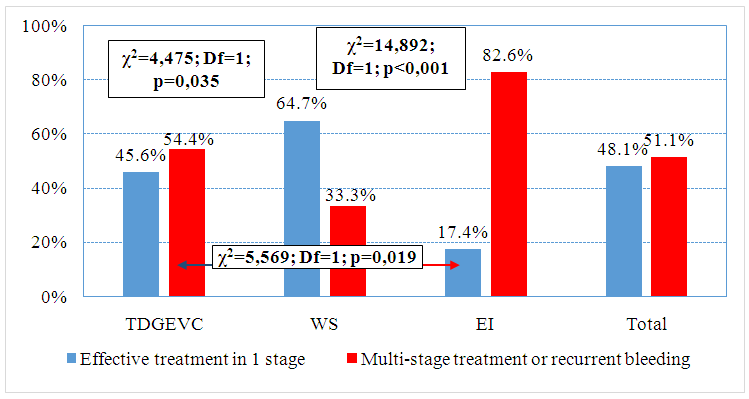
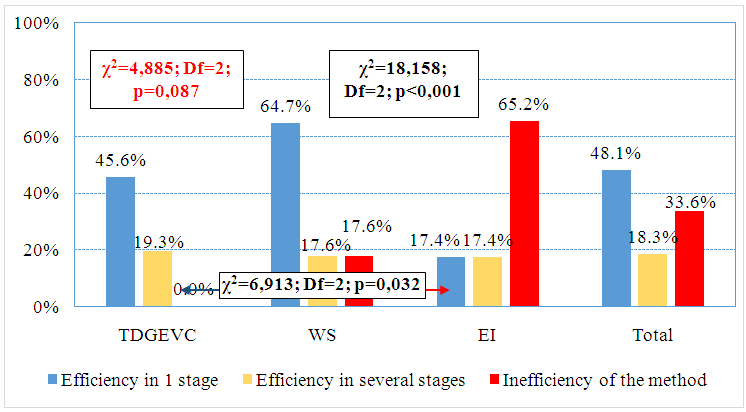
A more informative detail of the efficiency of the method for preventing recurrent bleeding at EPH is presented in the diagram Fig. 1. As it can be seen from the diagram, the efficiency of treatment in one stage was noted only in 45.6% of patients after TDGEVC, whereas after WS - in 64.7% of patients. Despite the fact that EI is mainly an additional or pre-stage aid, nevertheless, in 17.4% of patients, this intervention was the final procedure. The overall effectiveness, regardless of the method of preventing bleeding from EV, in one stage was noted only in 48.1% of patients with EPH (Fig. 1).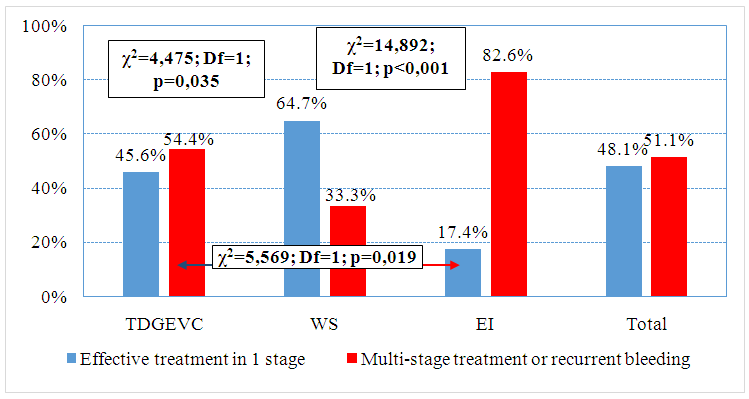 | Figure 1. The probability of effective one-stage prevention of recurrent bleeding from EV at EPH |
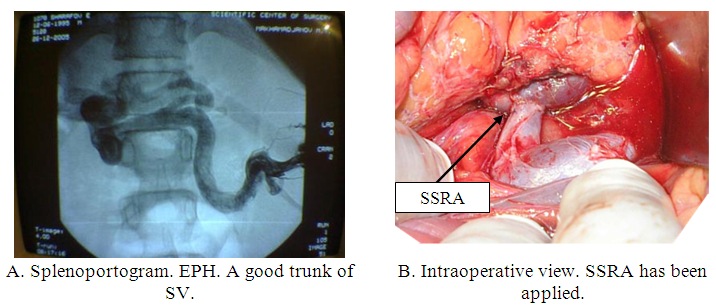
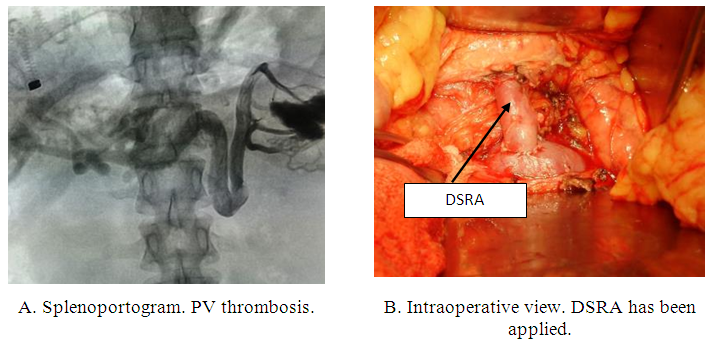
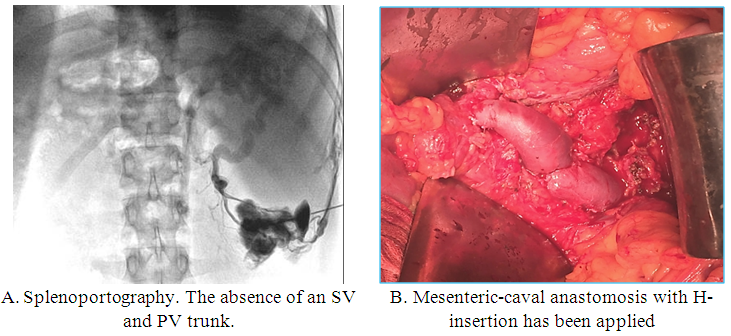
Various types of successful WS execution in patients with EPH are shown in Fig. 2, 3, 4.As it can be seen in Fig. 2 (A, B), the splenoportogram (A) shows a freely passable trunk of the splenic and portal veins, which determined the possibility of performing WS, in particular, the SSRA variant (B) was performed. In Fig. 3 (A, B), also on the splenoportogram (A), a variant favorable for performing WS is noted, in particular, it was possible to anastomose (DSRA) the distal end of the splenic vein into the side of the main trunk of the left renal vein (B).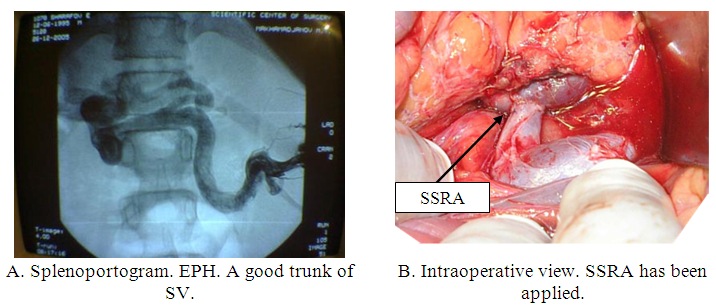 | Figure 2. EPH. Cavernous transformation of PV. Application of SSRA |
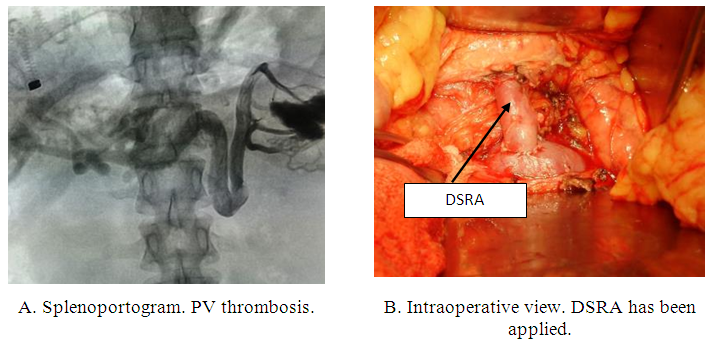 | Figure 3. EPH. PV thrombosis. Application of DSRA |
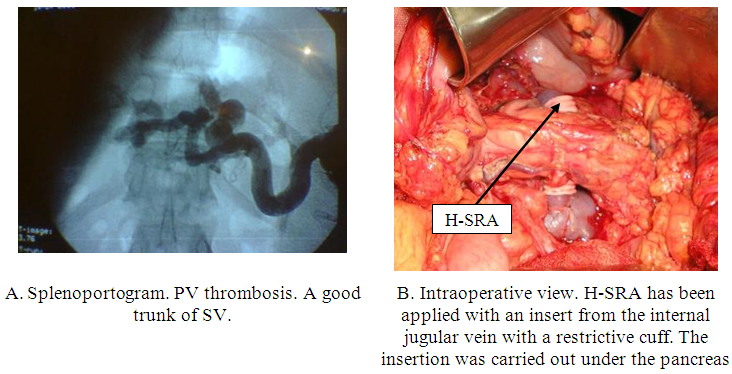
An interesting option is to use the right internal jugular vein under the condition of evident anatomical diastasis between the anastomosed vessels, as shown in Fig. 4. 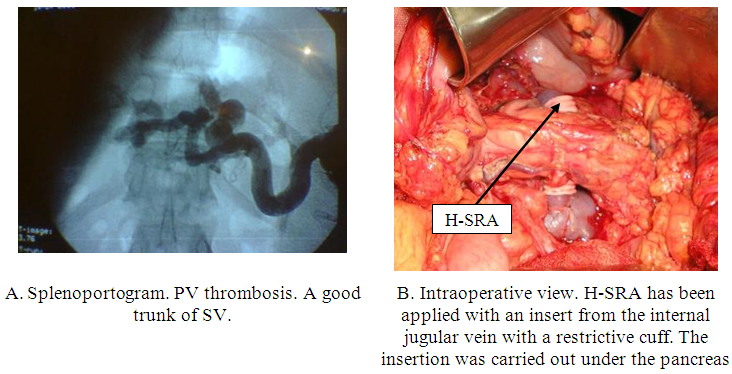 | Figure 4. EPH. PV thrombosis. Application of Н-СРА |
One of the most common options for performing WS in patients with EPH is the use of one of the venous mesenteric vessels. Thus, Fig. 5 shows a clinical case of using the mesenteric vein with its anastomosis either into the inferior vena cava or into the trunk of the left renal vein. 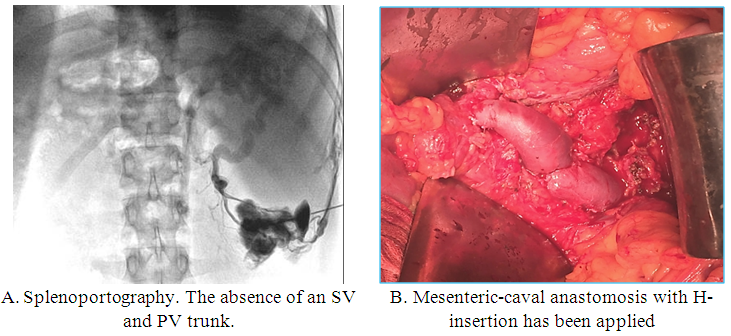 | Figure 5. EPH. Splenoportal thrombosis. Application of H-MCA |
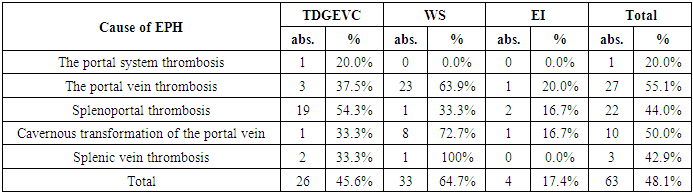
In the absence of the splenoportal bed patency TDGEVC was performed.From a clinical point of view, an analysis of the efficiency of one-stage prevention of recurrent bleeding from EV, depending on the causes of EPH development, deserves attention (Tab. 4). Thus, for TDGEVC, the most effective one-stage prevention is splenoportal thrombosis, with an indicator of 54.3%, and for WS – portal vein thrombosis, with an indicator of 63.9%. It should be noted that a small number of observations with EPH due to isolated thrombosis of the splenic vein, excludes the possibility of a reliable assessment of the efficiency of any intervention, however, the use of mesenteric venous inflow in WS makes it possible to perform a radical PH correction.Table 4. The probability of effective one-stage prevention of relapses depending on the cause of EPH
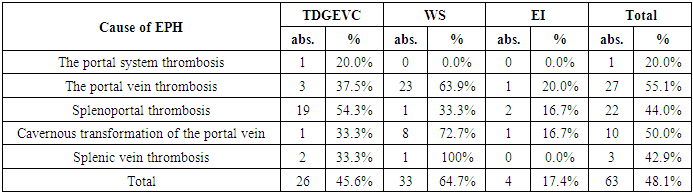 |
| |
|
The use of multi-stage tactics in this category of patients, depending on the causes of the development of EPH, determined that the most vulnerable group of patients were the patients with portal system thrombosis, to whom in 40.0% of cases we had to perform a multi-stage correction using TDGEVC (Tab. 5).Table 5. The probability of a multi-stage approach efficiency to the prevention of relapses
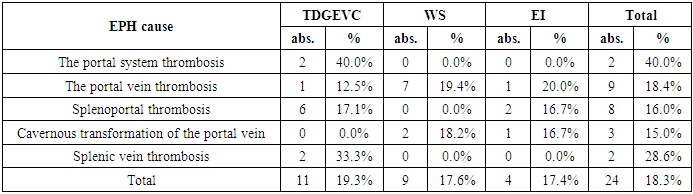 |
| |
|
Figure 6 shows the efficiency of the tactic taken. For TDGEVC, the one-stage tactic was effective only in 45.6% of patients, in several stages - in 19.3%, and the technique was evaluated as ineffective in 35.1% of patients with EPH. The most effective intervention in one stage was WS, with an indicator of 64.7%, while the inefficiency of the methodology was estimated at 17.6%. 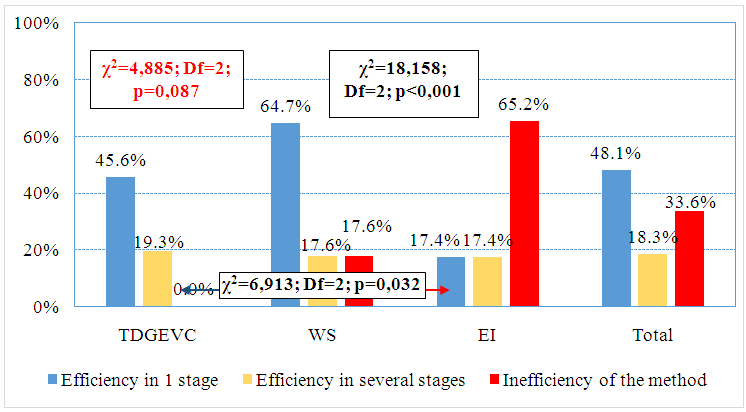 | Figure 6. The efficiency of the tactics taken to prevent relapses of bleeding from EV at EPH |
4. Discussion
The only treatment option for portal system thrombosis was TDGEVC, which was associated with the lack of suitable vessels for WS and the presence of varicose veins spreading to the stomach with the formation of nodes in areas that were difficult to reach for EL, while the dissociation efficiency was 20% (in 1 from 5), another 40% (2) required additional preventive EL sessions. At PV thrombosis, the single-stage efficiency of WS was 63.9% (in 23 from 36 patients), additional endoscopic sessions were required in 19.4% (7) patients, in general, having accounted for the share of successful treatment – 83.3% (30); when performing TDGEVC, these indicators were 37.5% (in 3 from 8), 12.5% (1) and in general - 50% (4), respectively; EI led to effective treatment only in 20% (in 1 from 5), 20% and in general in 40% (2) cases.In splenoportal thrombosis, TDGEVC was the most effective – 54.3% (in 19 from 35 patients in one stage), 17.1% (in 6 in several stages) and in general 71.4% (25) cases; at WS one-stage efficacy was noted only in 1 from 3 (33.3%) patients; EI led to effective treatment also in 33.3% (in 4 from 12), 16.7% (2) each in one and several stages.At the cavernous transformation of PV, WS was the most effective – 72.7% (in 8 from patients in one stage), 18.2% (in 2 in several stages) and in general in 90.9% (10); at TDGEVC, one-stage efficacy was achieved only in 33.3% (in 1 from 3) patients; EI also led to effective treatment in 33.3% (in 2 from 6), 16.7% (1) each in one and several stages.At SV thrombosis TDGEVC allowed to achieve a good result in 66.7% (4 from 6) cases, in one stage - in 33.3% and in several stages - in 33.3% (2) cases; WS (H-MCA) was performed in only 1 patient with a good effect; EI was not performed in this variant of EPH. After the performed DSRA, an adequate discharge from the splenic vein into the trunk of the left renal vein was noted, thereby having unloaded the conglomerates of the veins of the gastroesophageal zone. At the same time, 5 years after TDGEVC, the appearance of new venous trunks in the area of the cardioesophageal transition is noted which requires a step-by-step EI.
5. Conclusions
The combination of all the methods taken to prevent recurrent bleeding from EV at EPH allowed to get a good result in one stage treatment only in 48.1% of cases, 16.8% required additional EI sessions due to the absence of EV regression. At the same time, taking into account the reason for the formation of the subhepatic block, the most difficult category was portal system thrombosis and splenoportal thrombosis with the efficiency of single-stage or combined surgical approaches in 60% of cases.At cavernous transformation of PV, this indicator was 65.0%, at isolated thrombosis SV-71.4% and at thrombosis PV-73.5%. Depending on the variant of surgical prevention of recurrent bleeding from EV at EPH, the best results were obtained with WS, the efficiency of which in one stage was 64.7%. Additional endoscopic sessions were required to 17.6% of patients, in general, having accounted for the share of successful treatment – 82.4%. However, the implementation of this intervention is limited by anatomical conditions in various variants of the subhepatic block (38.9%). When performing TDGEVC, these indicators were 45.6%, 19.3% and 64.9% in general, respectively (to WS – χ2=4.885; Df=2; р=0.087); EI led to effective treatment only in general in 34.8% of cases (to WS – χ2=18.158; Df=2; р<0.001; to TDGEVC - χ2=6.913; Df=2; р=0.032).
References
| [1] | Kumar A, Sharma P, Arora A. Review article: portal vein obstruction--epidemiology, pathogenesis, natural history, prognosis and treatment. Aliment Pharmacol Ther. 2015; 41(3): 276-92. doi: 10.1111/apt.13019. |
| [2] | Pargewar S.S, Desai S., Rajesh S. et al. Imaging and radiological interventions in extra-hepatic portal vein obstruction // World J Radiol. 2016 Jun 28; 8(6): 556-70. doi: 10.4329/wjr.v8.i6.556. |
| [3] | Aman Elwadhi, Sharmila B Mukherjee Extra Hepatic Portal Vein Obstruction – Unobstructed. Indian Pediatr. 2018; 55(3): 239-240. |
| [4] | Khanna R, Sarin S.K. Idiopathic portal hypertension and extrahepatic portal venous obstruction. Hepatol Int. 2018; 12(1): 148-167. doi: 10.1007/s12072-018-9844-3. |
| [5] | Sharma R, Pradhan B, Karki P, Bartaula B. Clinico-epidemiological Profile of Extra Hepatic Portal Vein Obstruction: A Tertiary Care Hospital Based Retrospective Study. Kathmandu Univ Med J (KUMJ) 2019; 17(65): 30-34. |
| [6] | Yogesh K. C., Vijay B. Portal vein thrombosis. J Clin Exp Hepatol. 2015; 5(1): 22-40. doi: 10.1016/j.jceh.2014.12.008. |
| [7] | Samant H., Asafo-Agyei K. O., Garfield K. Portal Vein Thrombosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. 2021 Feb 3. |
| [8] | Sharma R, Pradhan B, Karki P, Bartaula B. Clinico-epidemiological Profile of Extra Hepatic Portal Vein Obstruction: A Tertiary Care Hospital Based Retrospective Study. Kathmandu Univ Med J (KUMJ) 2019; 17(65): 30-34. |
| [9] | Yogesh K. C., Vijay B. Portal vein thrombosis. J Clin Exp Hepatol. 2015; 5(1): 22-40. doi: 10.1016/j.jceh.2014.12.008. |
| [10] | Samant H., Asafo-Agyei K. O., Garfield K. Portal Vein Thrombosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. 2021 Feb 3. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML