Sh. N. Khudaybergenov, O. D. Eshonkhodjaev, R. Ya. Khayaliev, Sh. U. Rakhimiy
Republican Specialized Scientific and Practical Centre of Surgery, Named after Acad. V. Vakhidov, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article is devoted to the actual problem of thoracic surgery – the development of bronchopleural fistulas after lung resections. Considering that the frequency of lung resections in various diseases is increasing every year, and the frequency of purulent bronchopleural complications is kept at a high level, which requires long-term inpatient and outpatient treatment, and in some cases may end with disability of patients, there is still a need for in-depth study of this issue. The authors improved the treatment method of the lobar bronchus stump during lobectomy and bilobectomy, which was used in 80 patients. The use of a modified combined suture of the bronchial stump allowed to reduce the frequency of bronchopleural fistulas development from 8.5% to 2.5%.
Keywords:
Bronchopleural fistula, Lung resection, Stump, Lobectomy, Bilobectomy
Cite this paper: Sh. N. Khudaybergenov, O. D. Eshonkhodjaev, R. Ya. Khayaliev, Sh. U. Rakhimiy, Tactical and Technical Aspects of the Improved Method of Strengthening the Stump of the Lobar Bronchus, American Journal of Medicine and Medical Sciences, Vol. 11 No. 8, 2021, pp. 578-582. doi: 10.5923/j.ajmms.20211108.07.
1. Introduction
Open extended lung surgeries due to cancer and destructive organ injury continue to occupy a leading place despite significant progress in minimally invasive interventional and endoscopic surgery, early diagnosis of lung diseases [1-5]. At the same time, bronchopleural fistulas (BPF) and the associated pleural empyema are the main factor in reducing of surgical treatment efficiency of lung cancer, purulent - destructive lung diseases and other surgical pathology of the chest organs. Thoracic surgery and anesthesiology have made significant progress in the prevention and treatment of purulent bronchopleural complications after lung resection for the past 30 years. However, this problem has not been completely solved. Nowadays, there is no significant decrease in the frequency of development of bronchopleural fistulas after lung surgery. According to the literature, BPF occurs in 3-15% of operated patients. The problem of prevention and surgical treatment of BPF is constantly in the focus of attention of pulmonologists, continues to be widely and comprehensively covered in numerous publications [6-11].Aim of the study is to improve the existing methods of treating the lobar bronchus stump during lobo-and bilobectomy.
2. Material and Methods
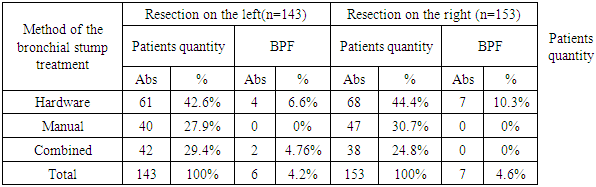
A method for strengthening of the lobar bronchus stump was developed at the Republican Specialized Scientific and Practical Centre of Surgery (RSSPCS) named after acad. V. Vakhidov which was used in 80 patients after lobo-and bilobectomy.Endobronchitis, panbronchitis and bronchial resection at the level of tumor tissues are factors that determine the unreliability of sutures that bring the bronchus walls closer together. In the course of through sutures conducted through the infected bronchial wall, ligature abscesses are formed and their eruption with the development of the bronchial stump failure occurs. A decrease in the reactivity of the body is also accompanied by a low level of reparative-regenerative processes, leading to a violation of the bronchial stump healing in the postoperative period and the development of complications from the side of pleural cavity and the remaining lung. The frequency of lung resections in various diseases increases every year, and the frequency of purulent bronchopleural complications is kept at a high level. All this requires long-term inpatient and outpatient treatment, and in some cases, patients may end up with disabilities. Taking into account all the above mentioned, the need for in-depth study of issues related to the development of BPF becomes social in nature. This stipulates the need to improve existing methods and search for new solutions for predicting and preventing postoperative complications. The task is solved by using a combination of a mechanical suture with the help of a bronchial suture device (UB) and additional strengthening with a manual suture in our own modification. In contrast to the use of only a mechanical or manual suture in isolation, this method allows to increase the reliability of the tightness of the bronchial stump suture.The staff of the Department of Lung Surgery of the RSSPCS named after acad. V. Vakhidov has been engaged in fundamental and applied developments on the problem of improving the diagnosis and treatment of patients with bronchopleural fistulas after lung resections since 2008. The purpose of developing a new method for closing the bronchial lumen during lung resections was to achieve a long-term reliable tightness of the stump; the length of the stump lumen should be minimal and its shape should tend to be wedge-shaped or semilunar. This, first of all, prevents sputum retention, the development of the "long stump" syndrome and creates more favorable aerodynamic conditions. In addition, the possibility of infection of the peribronchial tissues and the pleural cavity at the moment of crossing the bronchus and through the suture channels in the future should have been excluded; the edges of the crossed bronchus and the peribronchial tissue should not be subjected to traumatic manipulations. The continuity of the epithelial cover along the line of closure should be broken, its edges are well adapted; the blood supply must be kept up to the intersection level; the material used for the treatment of the bronchus should not cause reactions in the tissues; the technique of execution should be simple, do not require special tools and skills.The implementation of the claimed method consists of several stages:After the selection of the necessary bronchus and its adequate skeletonization, the UB-25 stitching device is applied to the bronchus in the first stage, the bronchus is stitched and crossed. Moreover, the length of the crossed bronchus stump is 8-10 mm (Fig. 1). | Figure 1. A single-row suture of tantalum staples is applied perpendicular to the axis of the bronchus using the UB-25 device |
After removing the preparation, we proceed to strengthen the bronchus stump with manual sutures. Previously, the so-called "notches" are made along the lateral and medial edges of the flattened bronchusstump which allow to compare the suture lines more closelydue to the dissection of the cartilaginous rings in the corners of the stump. Next, manual sutures are applied on both sides with an atraumatic biosin 4/0 thread, which, according to the "lock" type, strengthen the edges of the crossed bronchus stump, as the loops of the lateral sutures lie on the lateral surface of the bronchus stump. In addition, after stitching the bronchus with the UB-25 device, additional double nodal sutures are applied with a monofilament thread on an atraumatic needle (biosin 3/0), at the same time, punctures of the bronchial wall are carried out between rows of tantalum clips (Fig. 2).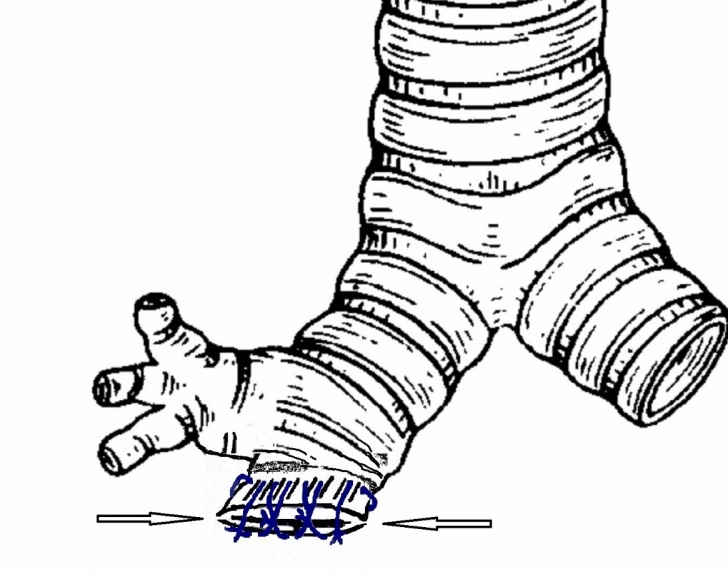 | Figure 2. Applying additional manual stitches after the UKB-25 device. The arrows indicate the "notches" in the corners of the bronchusstump |
With aapparatus suture, the prepared bronchus is raised and wound up between the branches of the open apparatus. A broncho-steapler is applied distally, for which the bronchus is somewhat stretched, which allows to move the device more centrally, to the place where the bronchus will be crossed. The branches of the device are gradually brought closer by the screw to their mark. Too strong screwing is dangerous, since the bronchial wall may be injured or even torn. Then we remove the fuse and squeeze the lock handles - this is how the stitching is carried out. The bronchus is cut off with a scalpel close to the branch of the device and the crossed place is smeared with iodine. The intersection of the bronchus with the help of a stitching device has the following advantages: the use of an inert material (tantalum clips), the speed of execution, the preservation of aseptic conditions, the absence of blood and fluids flowing into the bronchi, a smooth sealed seam. If there was a need to excise the bronchus, for example, when the tumor was located directly at the line of the bronchus intersection, the broncho-steapler was not used. In some cases, we strengthened the suture of the bronchial stump after the apparatus suture with additional nodular sutures with a synthetic resorption thread on an atraumatic needle.After crossing the bronchus, the stump was processed manually according to the Sweet method with atraumatic threads (Biosin 3/0; 4/0, PDS 3/0; 4/0), with the formation of a stump of minimal length. The ends of the threads were not cut off. Before you start hiding the stump of the bronchus, you should make sure that the stump is sealed tightly. A water sample is used for this purpose.
3. Results
When using only a mechanical seam, difficulties may arise if the stitching device malfunctions. The use of a manual suture requires a high qualification of the surgeon, high-quality suture material - the "human factor" can affect the frequency of bronchopleural fistula occurrence. In the proposed method of hiding the stump of the bronchus, these shortcomings are leveled by a combination of mechanical and manual suture, as well as in the modification of suturing in the form of preliminary "notches" in the corners of the stump, followed by strengthening with sutures in the transverse direction. This method allows to increase the reliability of the tightness of the bronchial stump suture and to reduce the frequency of stump insufficiency and bronchopleural fistula. The method is illustrated by the following clinical example.HISTORY CASE №799
 |
| |
|
The patient was admitted to the department of lung and mediastinal surgery as planned, with a directional diagnosis: COPD. Bronchiectasis of the lower lobe of the right lung.Complaints on admission: paroxysmal cough with difficult-to-separate sputum up to 15.0 ml per day, dyspnea with minor physical exertion, pain in the right half of the chest, general weakness.Anamnesis of the disease: pulmonary anamnesis since childhood, she was repeatedly treated both inpatient and outpatient with a diagnosis of chronic bronchitis at the place of residence. The aggravation has a seasonal character. In July 2019, after a cold, the patient began to worry about a paroxysmal cough with mucopurulent sputum, dyspnea with minor physical exertion and pain in the chest area on the left. She was treated on an outpatient basis with a temporary effect. Chest MSCT (23.01.2020): signs of a fibrous-calcified process with an uneven expansion of the bronchial lumen (varicose bronchiectasis) with a decrease in the lower lobe of the right lung. She was hospitalized in the department for further examination and decision of further treatment tactics. 07.02.2020. The surgery performed: thoracotomy on the right, lower bilobectomy, drainage of the right pleural cavity. It was intraoperatively revealed that the lower and middle lobes are low-air, purple-cyanotic color, the upper lobe is pink. The interlobar grooves are welded. Complete pneumolysis was performed. Mediastinotomy. The diaphragmatic nerve was isolated and taken on a holder. The lower pulmonary vein was isolated, taken on a holder. The interlobar groove was isolated, and the arterial branches leading to the lower and middle lobes were exposed. 2 arteries of the middle lobe were isolated, tied twice, sutured and crossed. The artery of the lower lobe was isolated, tied up below the discharge of the middle lobe arteries. Above the discharge of the mid-lobe branches, ligation, stitching and clipping of the arterial vessel was performed, and it was crossed. The next step was to isolate the veins coming from the middle lobe, tied in isolation twice, clipped, stitched and crossed. The lower pulmonary vein, previously taken on a holder, was twice ligated, sutured and crossed. An intermediate bronchus was found along the isolated interlobar groove; after skeletonization, a stitching device for bronchus No. 75 was placed on it. Lower bilobectomy. Suturing of the stump of the bronchus in the modification of the department – manual sutures were applied on both sides with an atraumatic thread of biosin 4/0, which, according to the "lock" type, strengthened the edges of the crossed bronchus stump having fixed themselves on the lateral surface of the bronchus stump with their loops. Additionally, 3 double nodal sutures were applied with a monofilament thread on an atraumatic needle (biosin 3/0), while punctures of the bronchial wall were carried out between rows of tantalum staples. Additional suturing with U-shaped sutures of the depleurized areas of the upper lobe. Checking the tightness of the bronchial stump under a layer of liquid when the pressure in the anesthesia circuit increases to 35 mm of water-tight. The remaining lobe is well ventilated, but does not fill the right hemithorax. In this regard, an additional frenico-exceresis was performed. Thorough hemostasis. Drainage of the pleural cavity. Layer-by-layer suturing of the surgical wound. Macropreparation: the removed middle and lower lobes of the right lung are pneumocyrrotically changed, on an incision with cavities with a putty-like liquid.The postoperative period was relatively satisfactory.The patient received antibacterial, anti-inflammatory, bronchodilating, desensitizing, mucolytic, detoxifying, restorative therapy, as well as endobronchial inhalations of drugs (Berodual, Lazolvan) using a nebulizer in the department. Drainage tubes from the pleural cavity were removed on the 3rd-5th day. During the control chest X-ray, the lungs are straightened, the sinuses are free. The postoperative wound is clean, healing by primary tension. The stitches are removed. Conclusion of histological examination No. 1051-1058 - in the preparations, lung tissue with areas of pronounced fibrosis, edema, vessels are dilated and full-blooded, lymphoid infiltration and tissue hemorrhage. The patient was discharged from the department in a satisfactory condition.Recommended: 1. Physical therapy, respiratory gymnastics. 2. Restriction of physical activity.After 1 month the patient came for a control examination to the polyclinic oftheRSSPCS named after acad. V. Vakhidov: the lungs were straightened on radiography, the postoperative scar was without signs of inflammation. She feltherself satisfactory.
4. Discussion
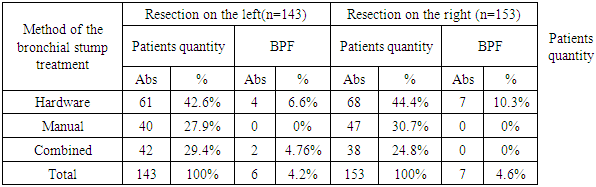
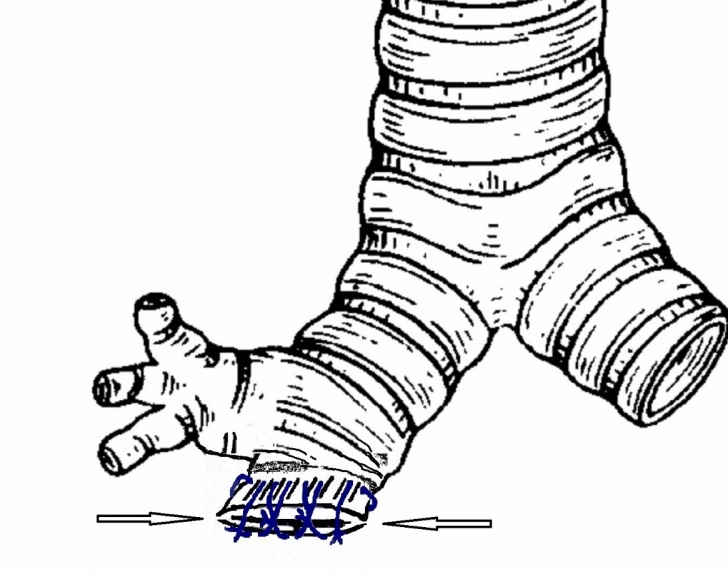
A comparative analysis with the closest analogues showed that when using our method, patients did not experience fatal outcomes, severe complications in the postoperative period in the form of bleeding, respiratory failure and suture failure. A control examination of patients in the period from 1 month to 5 years, which included chest MSCT, tracheobronchofibroscopy (TBFS), showed the formation of a stable stump of the crossed bronchus, depending on the performed surgery.The features of suturing the bronchus stump after lob-bilobectomy consisted in the use of manual or various methods of hardware suture. In 129 (43.6%) cases, the stump was sutured by hardware, in 87 (29.3%) – by manual sutures, in 80 (27.1%) cases a combined method was used. BPF was developed after hardware bronchial suture in 11 (8.5%) cases, after combined one - in 2 (2.5%) cases (Fig. 3).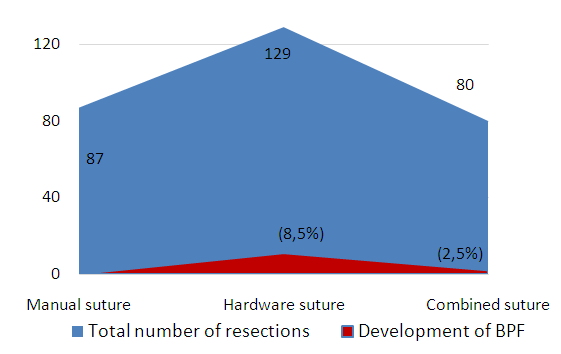 | Figure 3. The frequency of BPF development in patients after lob-bilobectomy, depending on the method of the bronchial stump suturing |
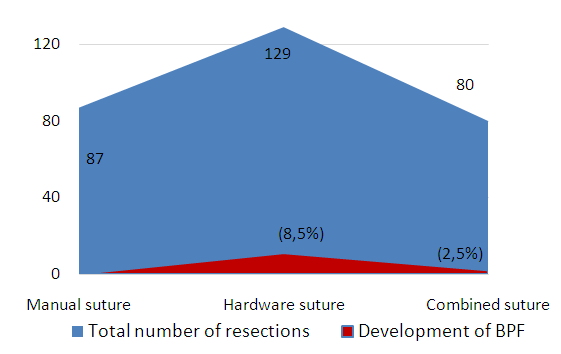
After resections on the left, the hardware method of suturing was used in 61 patients, BPF was developed in 6.6% of patients, the manual method was used in 5 cases, while the development of BPF was not noted. The combined method of the bronchial stump suturing was used in 42 cases, BPF was developed in 4.76% of patients.The difference was not for the better at the resections on the right. BPF was developed in 7 (10.3%) from 68 patients when using a hardware suture. There were no complications at the manual and combined sutures. In general, at lob-bilobectomyon the right, the risk of developing BPF was slightly higher than on the left, 4.6% versus 4.2%, respectively (Tab. 1).Table 1. The frequency of BPF development after resection, depending on the side of the lesion and the method of the bronchial stump treatment
 |
| |
|
Underestimation of risk factors for the development of BPF led to the development of this complication in 8.5% of patients with hardware bronchial suture. Suturing of the bronchus stump with manual sutures, unlike hardware, is the most hermetic, significantly reducing the frequency of BPF development.
5. Conclusions
The high risk of developing BPF after lob-bilobectomy, the frequency of which is definitely influenced by various predisposing factors, makes it necessary to rank patients by risk groups, in the structure of which the question of the bronchial stump suturing method, as well as the possibility of specific preventive measures, should be solved. No method of strengthening the suture of the lobar bronchus stump can 100% guarantee the prevention of BPF, which requires the development and implementation of new effective methods. Suturing of the bronchial stump after lob-bilobectomy with manual sutures is the most hermetic, reducing the frequency of BPF development from 8.5% (when using the hardware method) to 0%. The use of a modified combined suture of the bronchial stump allowed to reduce the frequency of BPF development to 2.5%.
References
| [1] | Porkhanov V.A., Polyakov I.S., Kononenko V.B. et al. Analysis of the results of prevention and treatment of bronchial stump failure after pneumonectomy // Materials of the first international conference on thoraco-abdominal surgery, June 5-8, 2008. Moscow P. 292-293. |
| [2] | Romanchishen A.F., Bakhar S.M. Tactics of treatment of acute patients | purulent lung diseases with bronchopleural fistulas, pyopneumothorax // Vestn. surgery named after I.I. Grekov. - 2001. - No. 3. - P. 86-88. |
| [3] | Chichevatov D.A., Gorshenev A.N., Sinev E.N. Surgical prevention of bronchopleural fistula after lung resections and pneumonectomy // Bulletin of surgery named after I.I. Grekov. - 2004. - Vol. 163, No. 5.- P. 125-127. |
| [4] | Clark JM, Cooke DT, Brown LM. Management of Complications After Lung Resection: Prolonged Air Leak and Bronchopleural Fistula. ThoracSurgClin. 2020 Aug; 30(3): 347-358. doi: 10.1016/j.thorsurg.2020.04.008. Epub 2020 Apr 17. PMID: 32593367. |
| [5] | Cundiff WB, McCormack FX, Wikenheiser-Brokamp K, Starnes S, Kotloff R, Benzaquen S. Successful management of a chronic, refractory bronchopleural fistula with endobronchial valves followed by talc pleurodesis. Am J RespirCrit Care Med 2014; 189: 490-1. |
| [6] | Lorut C, Giraud F, Lefebvre A. Traitementendoscopique des fistulesbronchopleurales [Bronchoscopic treatment of bronchopleural fistula]. Rev PneumolClin. 2018 Oct; 74(5): 359-362. French. doi: 10.1016/j.pneumo.2018.09.005. Epub 2018 Oct 11. PMID: 30316652. |
| [7] | Muthu V, Prasad KT, Agarwal R. Postoperative bronchopleural fistula: Does one size fit all? Lung India. 2020 Mar-Apr; 37(2): 97-99. doi: 10.4103/lungindia.lungindia_89_20. PMID: 32108591; PMCID: PMC7065545. |
| [8] | Salik I, Vashisht R, Abramowicz AE. Bronchopleural Fistula. 2021 May 12. In: StatPearls [Internet]. TreasureIsland (FL): StatPearlsPublishing; 2021 Jan–. PMID: 30521186. |
| [9] | Asamura H., Kondo H., Tsuchiya R. Management of the bronchial stump in pulmonary resections: a review of 533 consecutive recent bronchial closures //European Journal of Cardiothoracic Surgery. - 2000. - Vol. 17. - P.I06 - 110. |
| [10] | Caushi F., Skenduli I., Mezini A., Hatibi A., Bala S., Kokiqi F. The role of bronchial stump reinforcement by flap in prevention of broncho-pleural fistula after major lung resections. // Journal of Thoracic Oncology. April 2018. Vol. 13 No. 4:S53-S54. |
| [11] | Cundiff WB, McCormack FX, Wikenheiser-Brokamp K, Starnes S, Kotloff R, Benzaquen S. Successful management of a chronic, refractory bronchopleural fistula with endobronchial valves followed by talc pleurodesis. Am J RespirCrit Care Med 2014; 189: 490-1. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML