-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(7): 535-537
doi:10.5923/j.ajmms.20211107.07
Received: Jun. 26, 2021; Accepted: Jul. 14, 2021; Published: Jul. 26, 2021

Assessment of Parameters of Remodeling of the Right Heart Regions and the Level of Pulmonary Hypertension in Surgical Patients with Intra-Abdominal Pressure
Azizova Farida Fakhritdin Kizi, Sabirov Djura Marifbaevich, Djamaldinova Rimma Kamilovna, Nuralieva Dilafruz Mamadiyorovna, Abdukadirova Nodira Miranvarovna
Center for the Development of Professional Qualifications of Medical Workers, Uzbekistan
Correspondence to: Azizova Farida Fakhritdin Kizi, Center for the Development of Professional Qualifications of Medical Workers, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

When a patient has a severe degree of intra-abdominal pressure, the signs of remodeling of the right and left ventricles with the signs of volumetric hypertrophy of the left ventricle (LV) will develop, the cavity of the right ventricle (RV) and the RV outflow tract expands, the thickness of the anterior wall of RV (AWRV) increases, the trunk of the left pulmonary artery (PA) expands, the systolic pressure in the PA (SDPA) increases, as well as type first diastolic dysfunction of the ventricles of the heart will occur.
Keywords: Right ventricle, Remodeling, Surgical patients
Cite this paper: Azizova Farida Fakhritdin Kizi, Sabirov Djura Marifbaevich, Djamaldinova Rimma Kamilovna, Nuralieva Dilafruz Mamadiyorovna, Abdukadirova Nodira Miranvarovna, Assessment of Parameters of Remodeling of the Right Heart Regions and the Level of Pulmonary Hypertension in Surgical Patients with Intra-Abdominal Pressure, American Journal of Medicine and Medical Sciences, Vol. 11 No. 7, 2021, pp. 535-537. doi: 10.5923/j.ajmms.20211107.07.
Article Outline
1. Introduction
- Acute diseases of the abdominal organs are often accompanied by the development of severe complications, including multiple organ failure, which are the main cause of death in 95-97% of cases [1-3]. One of the reasons for the development of multiple organ failure syndrome in this category of patients is intra-abdominal hypertension (IAH). Intra-abdominal hypertension syndrome (IAHS) is a complex of symptoms that develop as a result of increased pressure in the abdominal cavity and is characterized by the development of multiple organ failure [4,5].
2. Purpose of the Research
- To study the parameters of remodeling of the right heart and the level of pulmonary hypertension in surgical patients with intra-abdominal pressure.
3. Material and Methods
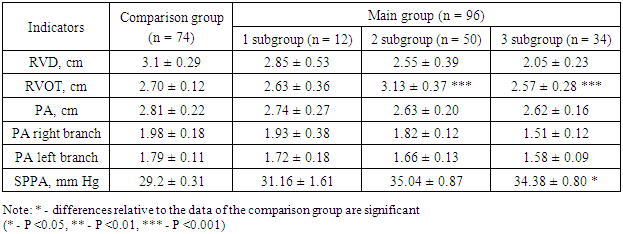
- The research was based on clinical and laboratory examination of 170 patients whose IAP has increased during and after surgery and 40 apparently healthy people of comparable age for an adequate assessment of laboratory data.The comparison group included 74 (43.5%) patients without increased IAP, who were treated in the intensive care unit, and the main group included 96 (56.5%) patients with increased IAP of varying degrees.During the study of RV systolic function, the following parameters were studied: RV diameter in diastole (RVD), RV outflow tract (RVOT), RV anterior wall thickness in diastole, diameter of the pulmonary artery (PA) and its branches, systolic pressure in PA (SPPA). The systolic pressure in the pulmonary artery (PPP) was calculated as the sum of the systolic pressure gradient between the RV and the atrium and the pressure in the RV:SDPA = Gd systolic TC + right atrial pressure.The systolic transtricuspid pressure gradient was calculated from the speed of the maximum tricuspid regurgitation stream, substituted into the simplified Bernoulli formula (4V2). The flow of tricuspid regurgitation was assessed using continuous wave Doppler from the apical four-chamber position or, in poor visualization, from the subcostal position of the long axis of the heart.
4. Results
- When comparing the parameters of the right ventricle in patients of subgroup 1 compared with subgroup 3, significant signs of hypertrophy were revealed (0.74 ± 0.11 and 0.49 ± 0.07, P <0.001) compared with subgroup 3 (0.66 ± 0, 08 and 0.49 ± 0.07, respectively, P <0.001). When comparing the 1st and 2nd subgroups, a more pronounced thickening of the RV wall was found in the group of patients with a strangulated ventral hernia (P <0.01).Right heart function indicators are presented in Table 1.
|
5. Clinical Example
- Patient H.R., 34 years old, No. IB, No. 1001. Was admitted to the Emergency Medical Center on 13.01. 2006.Discharged on January 21, 2006.Clinical diagnosis: Traumatic rupture of the extraperitoneal rectum. Ruptures of the parietal peritoneum of the recto-vesical part. Intra-abdominal bleeding. The laparotomy operation, sigmostomy, suturing of the rectal defect procedures are carried out. Cleansing and drainage of the abdominal cavity. The operation time was from 10.25 minutes to 15.50 minutes on January 13, 2006.A preliminary premedication was carried out followed by induction with the connection of mechanical ventilation O2-3.0 l / min, DO -600 ml, MOD-9.2 l / min. SP O2-100%.The blood loss was 2000 ml. Infusion -4200ml. Diuresis 1500 ml.Initially, IAP 17.5 mm Hg, CVD-50, AD-110/70 mm Hg, HR-92 per minute.Echocardiographic examination: Parasternal access, position of the long axis of the aorta: diameter of the aorta - 3.3 cm; left atrial diameter-3.8 cm; Apical approach, four-chambered section through the chambers of the heart: end-diastolic LV dimension -5.8 cm; L-left ventricle -7.2 cm, end-systolic LV size - 4.2 cm; thickness of IVS -1.1 cm; LV posterior wall -1.0 cm, LV ejection fraction by disc method (Simpson) - 47%, AS - 26%.Anteroposterior dimension of the right ventricle - 3.3 cm, the outflow tract of the right ventricle - 3.2 cm, the thickness of the anterior wall of the right ventricle - 0.5 cm... The diameter of the pulmonary artery at the level of the cusps is 2.4 cm. Apical four-chamber position - the dimensions of the RA 3.5 × 4.7 cm. PG Tricuspid valve is 59 mm Hg. The systolic pressure in the PA is 49 mm Hg. A clinical diagnosis was established.Doppler study of transmitral flow: E-0.48 m/s, flow A-0.54 m/s, E/A 0.88, Trans tricuspid flow (by pulse-wave Doppler method) peak E-0.34, peak A-0.4, the ratio of the peaks E/A 0.80. Study of the systolic flow on the RA, at the level of the valves: the speed was 0.40 m/s.This clinical example demonstrates the presence in a patient of severe IAH with the development of signs of remodeling of the right and left ventricles with signs of LV volumetric hypertrophy, expansion of the RV cavity, RV outflow tract, an increase in the thickness of the AWRV, expansion of the PA trunk, an increase in SPPA, and the occurrence of type first diastolic dysfunction of the ventricles of the heart.In dynamics - with a decrease in intra-abdominal pressure with other postoperative changes, there is a significant regression of pathological changes in cardiac and central hemodynamics. Such as improving the ventricular ejection fraction and increasing the percentage of myocardial fiber shortening fraction, restoring the diastolic function of the ventricles of the heart, as well as a decrease in the pressure gradient on Tricuspidal valve and RA valve. That is the negative effect in the form of an increase in resistance in the small and large circle of blood circulation by an increase in IAP, with its decrease or stabilizing, contributes to the stabilization of cardiac hemodynamic parameters.An echocardiogram has been provided on the third day after the operation, as well as in the background of constant drainage of the abdominal cavity, along with monitoring of hemostasis indicators, calculation of infused and excreted fluid, body temperature, blood pressure, heart rate. IAP during the study was 11 mm Hg. CVP -16 mm Hg, Blood pressure 115/70 mm Hg, heart rate - 84 per minute.Echocardiography indicators: diameter Ao -3.3 cm, LA - 3.5 cm, LVID ED - 5.6 cm, L - 7.4 cm, LVID ES - 3.7 cm, IVS -1.1 cm, Posterior wall of LV - 1,0 cm. EF -52%, AS 29%.The RV-anteroposterior dimension was -3.1 cm, the outflow tract of the RV-2.9 cm. RA -3.3 × 4.1 cm, PG TV 48 mm Hg. SDRA - 35 mm Hg. Doppler sonography of flows: on MV peak E 0.62, peak A-0.58, E / A mitral - 1.0 tricuspid flows - peak E-0.40, peak A-0.38, E/A tricusp. 1.0. Pressure gradient on TR ventricle amounted to 0.48 mm Hg. The systolic flow rate on the RA was 0.48 m/s.
6. Conclusions
- The negative effect of IAP in the form of an increase in resistance in the small and large circulation due to an increase in IAP, with its decrease or stabilization contributes to the normalization of cardiac hemodynamic parameters.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML